Clin Endosc.
2019 Sep;52(5):510-515. 10.5946/ce.2018.191.
Duodenal Stricture due to Necrotizing Pancreatitis following Endoscopic Ultrasound-Guided Ethanol Ablation of a Pancreatic Cyst: A Case Report
- Affiliations
-
- 1Department of Internal Medicine and Liver Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. gidoctor@snuh.org
- KMID: 2464675
- DOI: http://doi.org/10.5946/ce.2018.191
Abstract
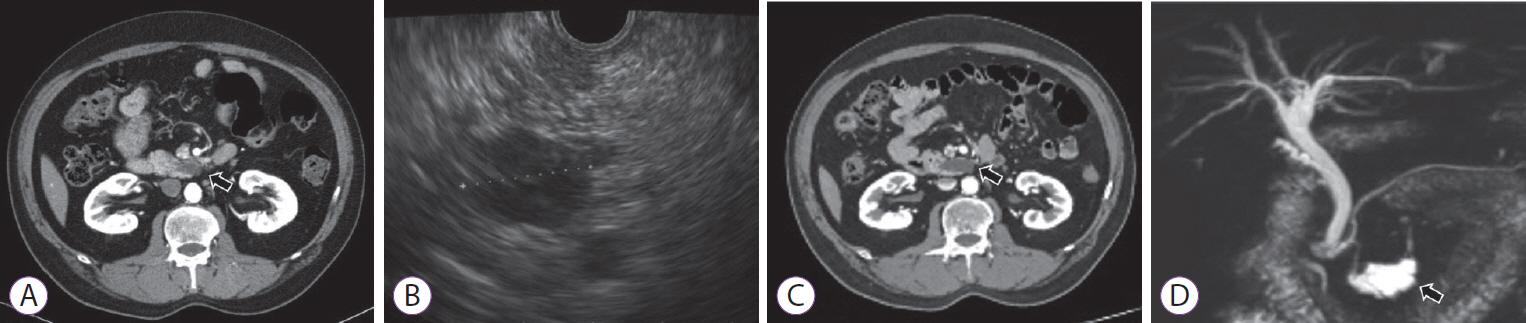
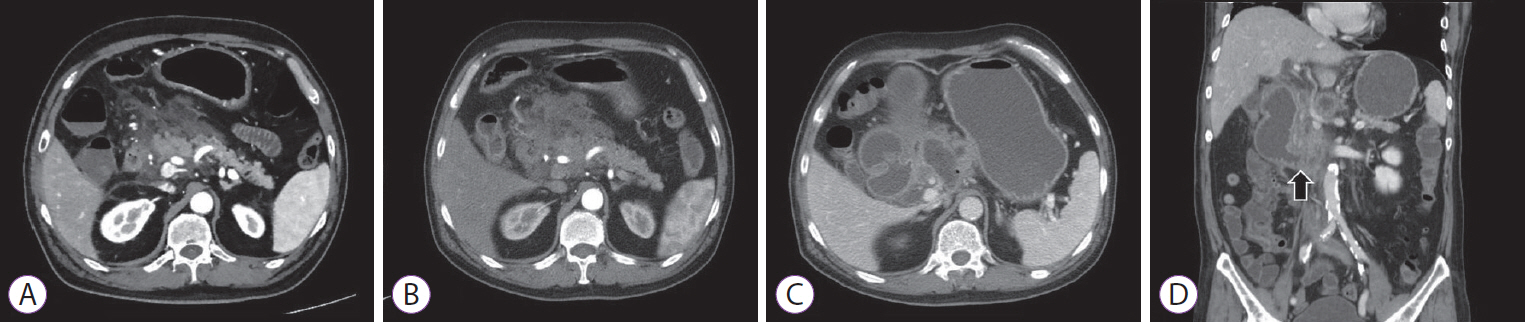
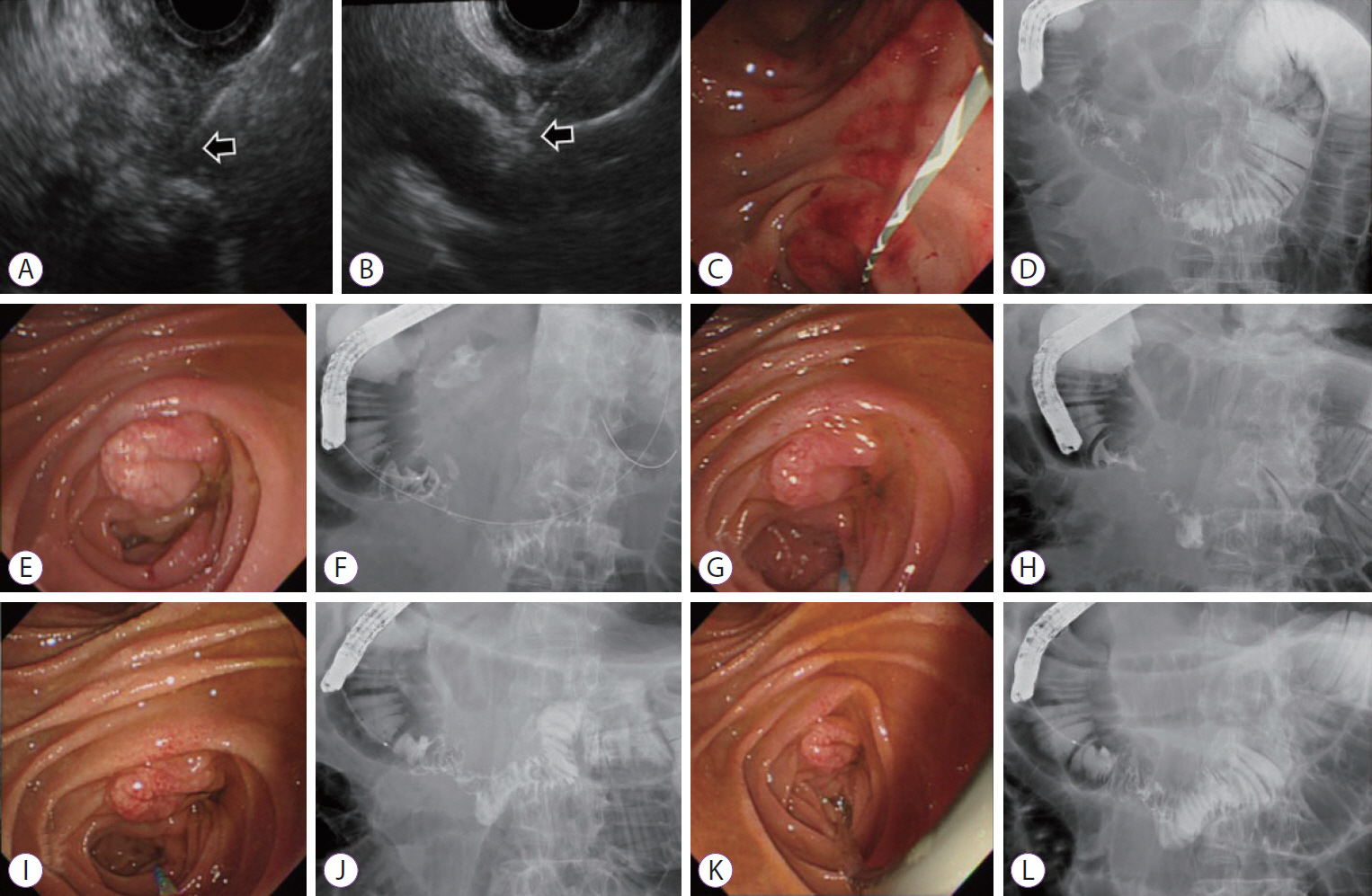
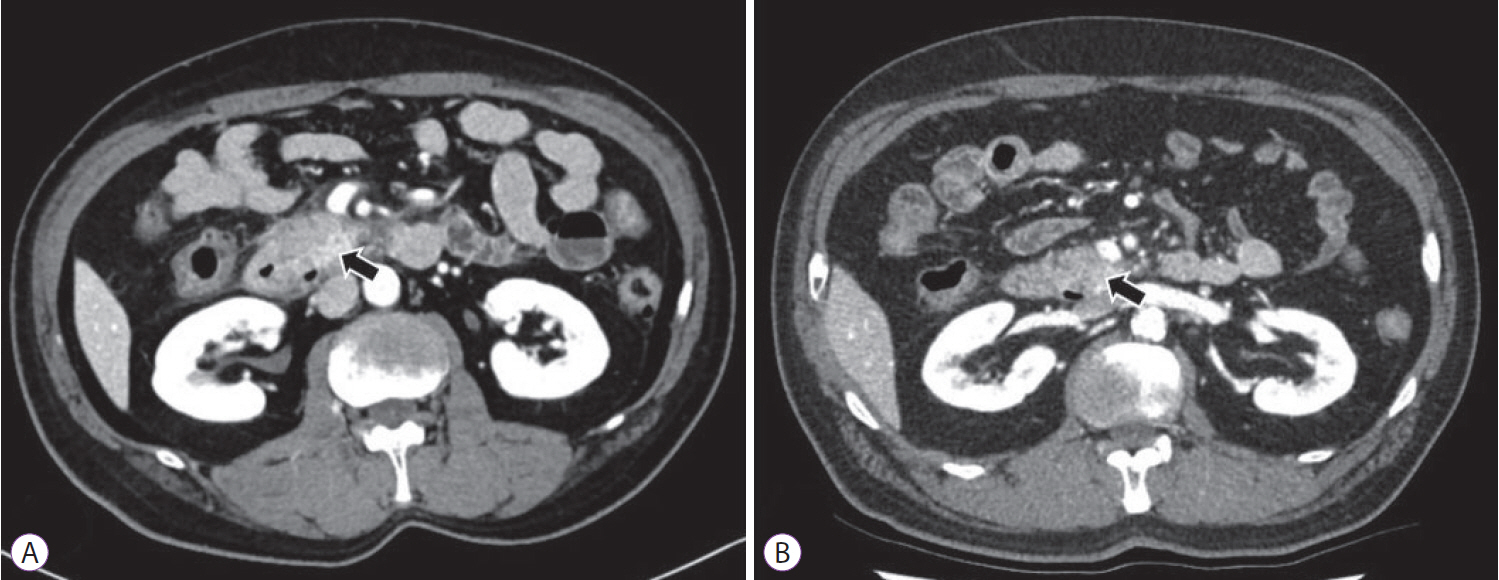
- The frequency of incidental detection of pancreatic cystic lesions (PCLs) is increasing because of the frequent use of cross-sectional imaging. The appropriate treatment for PCLs is challenging, and endoscopic ultrasound-guided ablation for PCLs has been reported in several studies. Although the feasibility and efficacy of this therapeutic modality have been shown, the safety issues associated with the procedure are still a concern. We present a case of a 61-year-old man who underwent ultrasound-guided ethanol ablation for PCL and needed repeated endoscopic balloon dilatation for severe duodenal stricture caused by necrotizing pancreatitis after the cyst ablation therapy.
MeSH Terms
Figure
Reference
-
1. Basar O, Brugge WR. My treatment approach: pancreatic cysts. Mayo Clin Proc. 2017; 92:1519–1531.
Article2. Lee SH. [Endoscopic treatment for pancreatic cystic lesions]. Korean J Gastroenterol. 2018; 71:10–17.
Article3. Park JK, Song BJ, Ryu JK, et al. Clinical outcomes of endoscopic ultrasonography-guided pancreatic cyst ablation. Pancreas. 2016; 45:889–894.
Article4. Tanaka M, Fernández-Del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017; 17:738–753.
Article5. Allen PJ. The diagnosis and management of cystic lesions of the pancreas. Chin Clin Oncol. 2017; 6:60.
Article6. Gan SI, Thompson CC, Lauwers GY, Bounds BC, Brugge WR. Ethanol lavage of pancreatic cystic lesions: initial pilot study. Gastrointest Endosc. 2005; 61:746–752.
Article7. Oh HC, Seo DW, Lee TY, et al. New treatment for cystic tumors of the pancreas: EUS-guided ethanol lavage with paclitaxel injection. Gastrointest Endosc. 2008; 67:636–642.
Article8. Oh HC, Seo DW, Kim SC, et al. Septated cystic tumors of the pancreas: is it possible to treat them by endoscopic ultrasonography-guided intervention? Scand J Gastroenterol. 2009; 44:242–247.
Article9. DeWitt J, McGreevy K, Schmidt CM, Brugge WR. EUS-guided ethanol versus saline solution lavage for pancreatic cysts: a randomized, double-blind study. Gastrointest Endosc. 2009; 70:710–723.
Article10. Oh HC, Seo DW, Song TJ, et al. Endoscopic ultrasonography-guided ethanol lavage with paclitaxel injection treats patients with pancreatic cysts. Gastroenterology. 2011; 140:172–179.
Article11. DiMaio CJ, DeWitt JM, Brugge WR. Ablation of pancreatic cystic lesions: the use of multiple endoscopic ultrasound-guided ethanol lavage sessions. Pancreas. 2011; 40:664–668.12. Caillol F, Poincloux L, Bories E, et al. Ethanol lavage of 14 mucinous cysts of the pancreas: a retrospective study in two tertiary centers. Endosc Ultrasound. 2012; 1:48–52.
Article13. DeWitt JM, Al-Haddad M, Sherman S, et al. Alterations in cyst fluid genetics following endoscopic ultrasound-guided pancreatic cyst ablation with ethanol and paclitaxel. Endoscopy. 2014; 46:457–464.
Article14. Gómez V, Takahashi N, Levy MJ, et al. EUS-guided ethanol lavage does not reliably ablate pancreatic cystic neoplasms (with video). Gastrointest Endosc. 2016; 83:914–920.
Article15. Choi JH, Seo DW, Song TJ, et al. Long-term outcomes after endoscopic ultrasound-guided ablation of pancreatic cysts. Endoscopy. 2017; 49:866–873.
Article16. Moyer MT, Sharzehi S, Mathew A, et al. The safety and efficacy of an alcohol-free pancreatic cyst ablation protocol. Gastroenterology. 2017; 153:1295–1303.
Article17. Choi JH, Lee SH, Choi YH, et al. Clinical outcomes of endoscopic ultrasound-guided ethanol ablation for pancreatic cystic lesions compared with the natural course: a propensity score matching analysis. Therap Adv Gastroenterol. 2018; 11:1756284818759929.
Article18. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.
Article19. Choi JH, Lee SH, You MS, et al. Safety and adverse events of EUS-guided ethanol ablation for pancreatic cystic lesions: a single center experience. In : Joint Meeting of the Asian-Oceanic Pancreatic Association, the Korean Pancreatobiliary Association, and the Korean Pancreas Surgery Club 2018; 2018 Apr 26-28; Seoul, Korea. Seoul: Korean Pancreatobiliary Association, Korean Pancreas Surgery Club;2018. p. 386–387.20. Oh HC, Brugge WR. EUS-guided pancreatic cyst ablation: a critical review (with video). Gastrointest Endosc. 2013; 77:526–533.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Ultrasound-Guided Treatment of Pancreatic Cystic and Solid Masses
- Endoscopic ultrasound-guided ablation of pancreatic cystic lesions
- Recent developments in endoscopic ultrasound-guided ablation treatment
- Successful Endoscopic Ultrasound-Guided Alcohol Ablation of Sporadic Insulinoma Using Three-Dimensional Targeting (with Video)
- Recent developments in endoscopic ultrasound-guided diagnosis and therapy of pancreatic cystic neoplasms