Cancer Res Treat.
2019 Apr;51(2):727-736. 10.4143/crt.2018.262.
Early Decline in Left Ventricular Ejection Fraction Can Predict Trastuzumab-Related Cardiotoxicity in Patients with Breast Cancer: A Study Using 13 Years of Registry Data
- Affiliations
-
- 1Division of Cardiology, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Division of Hematology-Oncology, Department of Medicine, Inha University Hospital, Inha University School of Medicine, Incheon, Korea.
- 3Division of Hematology-Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. yeonh.park@samsung.com
- KMID: 2464418
- DOI: http://doi.org/10.4143/crt.2018.262
Abstract
- PURPOSE
While concerns regarding trastuzumab-related cardiac dysfunction (TRCD) in patients with breast cancer are increasing, there is a lack of evidence supporting the current recommendations for TRCD monitoring. We aimed to investigate the clinical predictors of TRCD in the adjuvant setting of human epidermal growth factor receptor 2-positive breast cancer patients.
MATERIALS AND METHODS
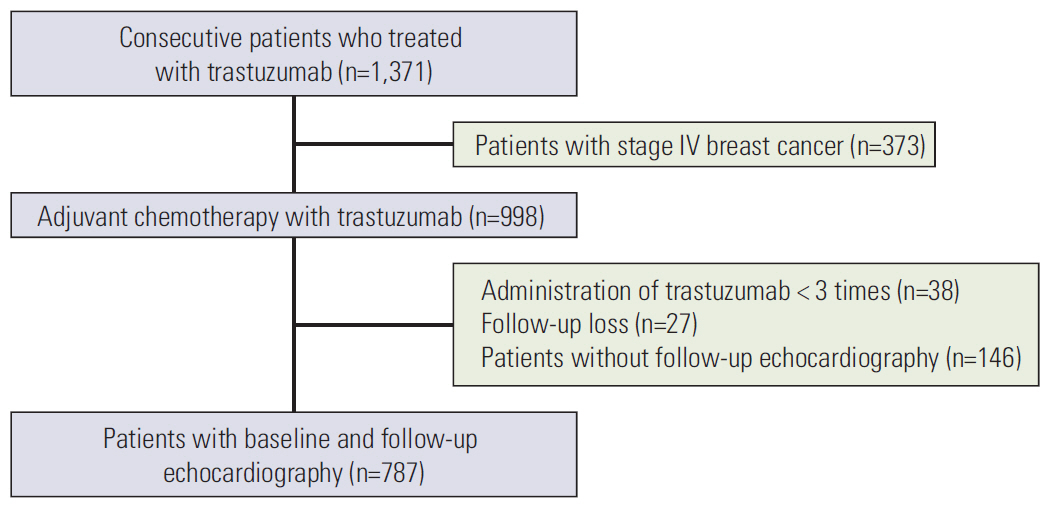
From August 2003 to April 2016, consecutive 998 patients who were treated with adjuvant trastuzumab for breast cancer were retrospectively evaluated. TRCD was defined as a decrease ≥10% in left ventricular ejection fraction (LVEF), with a decline below the normal limit or symptomatic heart failure.
RESULTS
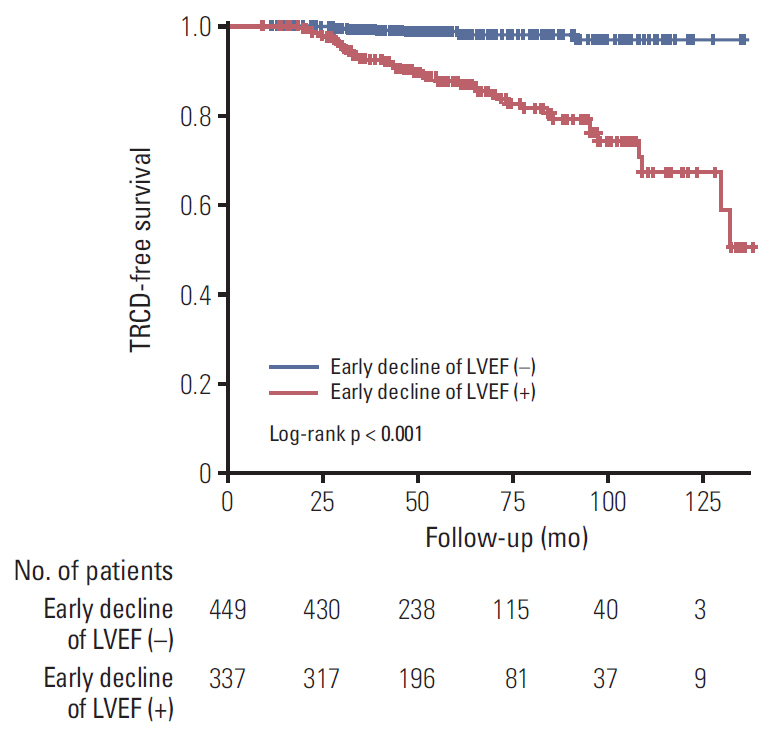
Among 787 eligible patients who had complete data sets consisting of both baseline and follow-up assessment of left ventricular systolic function by echocardiography (mean age, 49.9±9.5 years), 58 (7.4%) developed TRCD. TRCD patients had lower baseline LVEF (63% [59-66] vs. 65% [61-68], p=0.016) and more frequently administered Adriamycin (98% vs. 89%, p=0.022) than those without TRCD. On follow-up echocardiography, a drop in LVEF ≥5% within the first 3 months was more frequent in TRCD patients (78.3% vs. 38.4%, p<0.001). Regardless of baseline LVEF and Adriamycin treatment, a drop in LVEF ≥5% within the first 3 months of trastuzumab administration was strongly associated with the development of TRCD (adjusted hazard ratio, 45.1[17.0-127.6], p<0.001).
CONCLUSION
The overall incidence of TRCD was 7.4% in Asian breast cancer patients treated with adjuvant trastuzumab. A decline in LVEF ≥5% within the first 3 months of trastuzumab initiation was strongly associated with TRCD development in patients with breast cancer.
MeSH Terms
Figure
Reference
-
References
1. Romond EH, Perez EA, Bryant J, Suman VJ, Geyer CE Jr, Davidson NE, et al. Trastuzumab plus adjuvant chemotherapy for operable HER2-positive breast cancer. N Engl J Med. 2005; 353:1673–84.
Article2. Jones LW, Haykowsky MJ, Swartz JJ, Douglas PS, Mackey JR. Early breast cancer therapy and cardiovascular injury. J Am Coll Cardiol. 2007; 50:1435–41.
Article3. Hahn VS, Lenihan DJ, Ky B. Cancer therapy-induced cardiotoxicity: basic mechanisms and potential cardioprotective therapies. J Am Heart Assoc. 2014; 3:e000665.
Article4. Telli ML, Hunt SA, Carlson RW, Guardino AE. Trastuzumab-related cardiotoxicity: calling into question the concept of reversibility. J Clin Oncol. 2007; 25:3525–33.
Article5. Ewer SM, Ewer MS. Cardiotoxicity profile of trastuzumab. Drug Saf. 2008; 31:459–67.
Article6. Wadhwa D, Fallah-Rad N, Grenier D, Krahn M, Fang T, Ahmadie R, et al. Trastuzumab mediated cardiotoxicity in the setting of adjuvant chemotherapy for breast cancer: a retrospective study. Breast Cancer Res Treat. 2009; 117:357–64.
Article7. Tan-Chiu E, Yothers G, Romond E, Geyer CE Jr, Ewer M, Keefe D, et al. Assessment of cardiac dysfunction in a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel, with or without trastuzumab as adjuvant therapy in node-positive, human epidermal growth factor receptor 2-overexpressing breast cancer: NSABP B-31. J Clin Oncol. 2005; 23:7811–9.
Article8. Zamorano JL, Lancellotti P, Rodriguez Munoz D, Aboyans V, Asteggiano R, Galderisi M, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur Heart J. 2016; 37:2768–801.9. Curigliano G, Cardinale D, Suter T, Plataniotis G, de Azambuja E, Sandri MT, et al. Cardiovascular toxicity induced by chemotherapy, targeted agents and radiotherapy: ESMO Clinical Practice Guidelines. Ann Oncol. 2012; 23 Suppl 7:vii155–66.
Article10. de Azambuja E, Procter MJ, van Veldhuisen DJ, Agbor-Tarh D, Metzger-Filho O, Steinseifer J, et al. Trastuzumab-associated cardiac events at 8 years of median follow-up in the Herceptin Adjuvant trial (BIG 1-01). J Clin Oncol. 2014; 32:2159–65.
Article11. Shah AM, Solomon SD. Myocardial deformation imaging: current status and future directions. Circulation. 2012; 125:e244–8.12. Romond EH, Jeong JH, Rastogi P, Swain SM, Geyer CE Jr, Ewer MS, et al. Seven-year follow-up assessment of cardiac function in NSABP B-31, a randomized trial comparing doxorubicin and cyclophosphamide followed by paclitaxel (ACP) with ACP plus trastuzumab as adjuvant therapy for patients with node-positive, human epidermal growth factor receptor 2-positive breast cancer. J Clin Oncol. 2012; 30:3792–9.13. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39. e14.
Article14. Piccart-Gebhart MJ, Procter M, Leyland-Jones B, Goldhirsch A, Untch M, Smith I, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005; 353:1659–72.15. Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, et al. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2014; 27:911–39.
Article16. McArthur HL, Chia S. Cardiotoxicity of trastuzumab in clinical practice. N Engl J Med. 2007; 357:94–5.
Article17. Perez EA, Suman VJ, Davidson NE, Sledge GW, Kaufman PA, Hudis CA, et al. Cardiac safety analysis of doxorubicin and cyclophosphamide followed by paclitaxel with or without trastuzumab in the North Central Cancer Treatment Group N9831 adjuvant breast cancer trial. J Clin Oncol. 2008; 26:1231–8.
Article18. Lin CH, Shen CY, Lee JH, Huang CS, Yang CH, Kuo WH, et al. High prevalence of the BIM deletion polymorphism in young female breast cancer in an East Asian country. PLoS One. 2015; 10:e0124908.
Article19. Seidman A, Hudis C, Pierri MK, Shak S, Paton V, Ashby M, et al. Cardiac dysfunction in the trastuzumab clinical trials experience. J Clin Oncol. 2002; 20:1215–21.
Article20. Guglin M, Cutro R, Mishkin JD. Trastuzumab-induced cardiomyopathy. J Card Fail. 2008; 14:437–44.
Article21. Suter TM, Procter M, van Veldhuisen DJ, Muscholl M, Bergh J, Carlomagno C, et al. Trastuzumab-associated cardiac adverse effects in the herceptin adjuvant trial. J Clin Oncol. 2007; 25:3859–65.
Article22. Choi JY, Cho EY, Choi YJ, Lee JH, Jung SP, Cho KR, et al. Incidence and risk factors for congestive heart failure in patients with early breast cancer who received anthracycline and/or trastuzumab: a big data analysis of the Korean Health Insurance Review and Assessment service database. Breast Cancer Res Treat. 2018; 171:181–8.
Article23. Zagar TM, Cardinale DM, Marks LB. Breast cancer therapy-associated cardiovascular disease. Nat Rev Clin Oncol. 2016; 13:172–84.
Article24. Rutqvist LE, Lax I, Fornander T, Johansson H. Cardiovascular mortality in a randomized trial of adjuvant radiation therapy versus surgery alone in primary breast cancer. Int J Radiat Oncol Biol Phys. 1992; 22:887–96.
Article25. Haybittle JL, Brinkley D, Houghton J, A'Hern RP, Baum M. Postoperative radiotherapy and late mortality: evidence from the Cancer Research Campaign trial for early breast cancer. BMJ. 1989; 298:1611–4.
Article26. Halyard MY, Pisansky TM, Dueck AC, Suman V, Pierce L, Solin L, et al. Radiotherapy and adjuvant trastuzumab in operable breast cancer: tolerability and adverse event data from the NCCTG Phase III Trial N9831. J Clin Oncol. 2009; 27:2638–44.
Article27. Zambelli A, Della Porta MG, Eleuteri E, De Giuli L, Catalano O, Tondini C, et al. Predicting and preventing cardiotoxicity in the era of breast cancer targeted therapies: novel molecular tools for clinical issues. Breast. 2011; 20:176–83.
Article28. Angeras O, Albertsson P, Karason K, Ramunddal T, Matejka G, James S, et al. Evidence for obesity paradox in patients with acute coronary syndromes: a report from the Swedish Coronary Angiography and Angioplasty Registry. Eur Heart J. 2013; 34:345–53.29. Lavie CJ, Milani RV, Ventura HO. Impact of obesity on outcomes in myocardial infarction combating the "obesity paradox". J Am Coll Cardiol. 2011; 58:2651–3.30. Pingitore A, Di Bella G, Lombardi M, Iervasi G, Strata E, Aquaro GD, et al. The obesity paradox and myocardial infarct size. J Cardiovasc Med (Hagerstown). 2007; 8:713–7.
Article31. Mohamed-Ali V, Goodrick S, Bulmer K, Holly JM, Yudkin JS, Coppack SW. Production of soluble tumor necrosis factor receptors by human subcutaneous adipose tissue in vivo. Am J Physiol. 1999; 277:E971–5.32. Tamarappoo B, Dey D, Shmilovich H, Nakazato R, Gransar H, Cheng VY, et al. Increased pericardial fat volume measured from noncontrast CT predicts myocardial ischemia by SPECT. JACC Cardiovasc Imaging. 2010; 3:1104–12.
Article33. Walker J, Bhullar N, Fallah-Rad N, Lytwyn M, Golian M, Fang T, et al. Role of three-dimensional echocardiography in breast cancer: comparison with two-dimensional echocardiography, multiple-gated acquisition scans, and cardiac magnetic resonance imaging. J Clin Oncol. 2010; 28:3429–36.
Article34. Sawaya H, Sebag IA, Plana JC, Januzzi JL, Ky B, Tan TC, et al. Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes, and trastuzumab. Circ Cardiovasc Imaging. 2012; 5:596–603.
Article35. Thavendiranathan P, Poulin F, Lim KD, Plana JC, Woo A, Marwick TH. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J Am Coll Cardiol. 2014; 63:2751–68.36. Villarraga HR, Herrmann J, Nkomo VT. Cardio-oncology: role of echocardiography. Prog Cardiovasc Dis. 2014; 57:10–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk of Trastuzumab-Related Cardiotoxicity in Early Breast Cancer Patients: A Prospective Observational Study
- MicroRNA-130a Increases and Predicts Cardiotoxicity during Adjuvant Chemotherapy in Human Epidermal Growth Factor Receptor-2-Positive Breast Cancer
- Early Cardiac Function Monitoring for Detection of Subclinical Doxorubicin Cardiotoxicity in Young Adult Patients with Breast Cancer
- Chemotherapy-Induced Left Ventricular Dysfunction in Patients with Breast Cancer
- Cardioprotective Effect of Dexrazoxane in Patients with HER2-Positive Breast Cancer Who Receive Anthracycline Based Adjuvant Chemotherapy Followed by Trastuzumab