J Korean Neurosurg Soc.
2019 Jul;62(4):487-491. 10.3340/jkns.2018.0052.
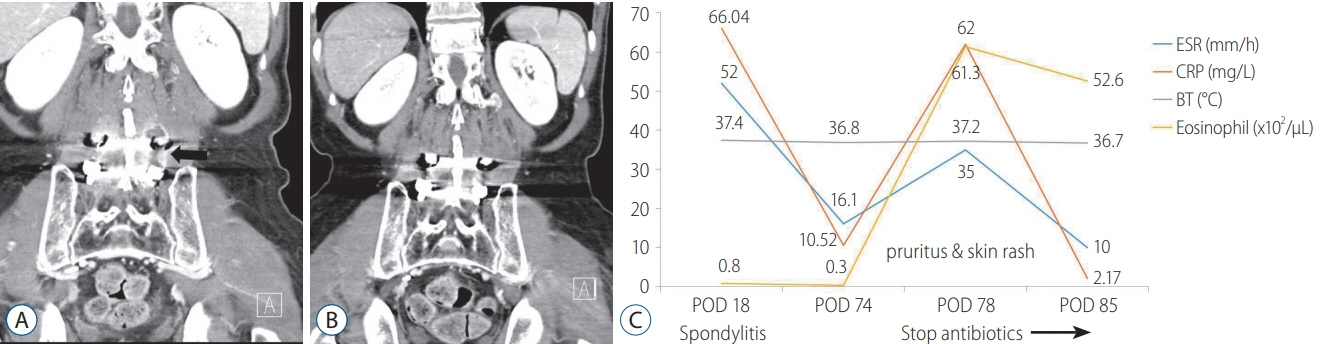
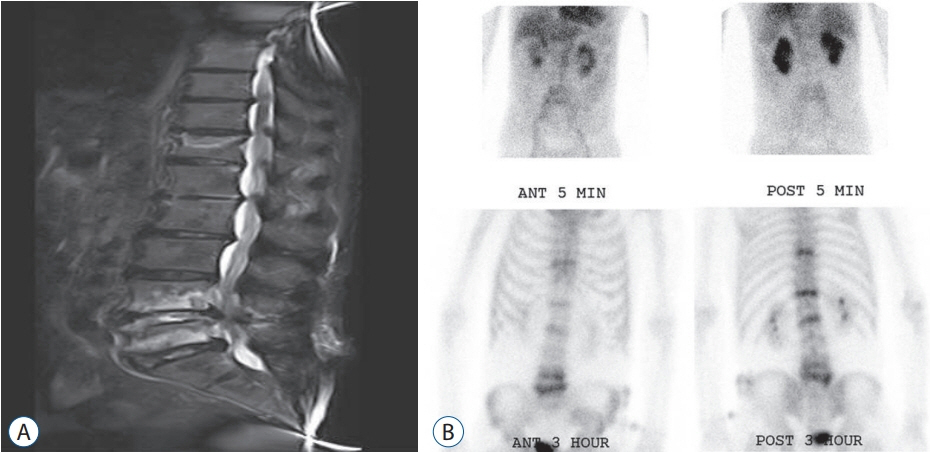
Antibiotic-Induced Increase in Inflammatory Markers in Cured Infectious Spondylitis: Two Case Reports
- Affiliations
-
- 1Department of Neurosurgery, Wonkwang University School of Medicine, Iksan, Korea. kseom@wonkwang.ac.kr
- KMID: 2463680
- DOI: http://doi.org/10.3340/jkns.2018.0052
Abstract
- Conservative therapy with appropriate antibiotics is essential for most patients with infectious spondylitis. Although most antibiotics do not cause problems if it used properly and serious side effects are rare, side effects can occur with any class of drugs and adverse reactions of antibiotics can range from mild allergic reactions to serious and fulminant adverse events. These side effects are also extremely variable from patient to patient and from antibiotic to antibiotic. A side effect of antibiotics may paradoxically increase inflammatory marker levels. Here, the author presents two cases of antibiotic-induced increase in inflammatory markers in cured infectious spondylitis. The patients were successfully treated after stopping the antibiotic therapy. The differential diagnosis between antibiotic side effects and infection should be considered very carefully because the treatment is completely different. Although the exact mechanisms underlying successful treatment without antibiotics are unclear, we should consider the side effects of antibiotics when following inflammatory markers during treatment of infectious spondylitis.
Keyword
MeSH Terms
Figure
Reference
-
References
1. An SY, Hwang EK, Kim JH, Kim JE, Jin HJ, Jin SM, et al. Vancomycinassociated spontaneous cutaneous adverse drug reactions. Allergy Asthma Immunol Res. 3:194–198. 2011.
Article2. Ball P, Stahlmann R, Kubin R, Choudhri S, Owens R. Safety profile of oral and intravenous moxifloxacin: cumulative data from clinical trials and postmarketing studies. Clin Ther. 26:940–950. 2004.
Article3. Bartlett JG. Clinical practice. Antibiotic-associated diarrhea. N Engl J Med. 346:334–339. 2002.4. Carragee EJ, Kim D, van der Vlugt T, Vittum D. The clinical use of erythrocyte sedimentation rate in pyogenic vertebral osteomyelitis. Spine (Phila Pa 1976). 22:2089–2093. 1997.
Article5. Chelsom J, Solberg CO. Vertebral osteomyelitis at a Norwegian university hospital 1987-97: clinical features, laboratory findings and outcome. Scand J Infect Dis. 30:147–151. 1998.
Article6. Cheung WY, Luk KD. Pyogenic spondylitis. Int Orthop. 36:397–404. 2012.
Article7. Harrison M. Erythrocyte sedimentation rate and C-reactive protein. Aust Prescr. 38:93–94. 2015.
Article8. Osei-Bimpong A, Meek JH, Lewis SM. ESR or CRP? A comparison of their clinical utility. Hematology. 12:353–357. 2007.
Article9. Park JH, Shin HS, Park JT, Kim TY, Eom KS. Differentiation between tuberculous spondylitis and pyogenic spondylitis on MR imaging. Korean J Spine. 8:283–287. 2011.
Article10. Ray WA, Murray KT, Hall K, Arbogast PG, Stein MC. Azithromycin and the risk of cardiovascular death. N Engl J Med. 366:1881–1890. 2012.
Article11. Reeves G. C-reactive protein. Aust Prescr. 30:74–76. 2007.12. Shin YS, Lee YW, Choi YH, Park B, Jee YK, Choi SK, et al. Spontaneous reporting of adverse drug events by Korean regional pharmacovigilance centers. Pharmacoepidemiol Drug Saf. 18:910–915. 2009.
Article13. Son DW, Song KS. Infectious spondylitis. In : Zhang HY, editor. The Textbook of Spiney. ed 2. Seoul: Koonja;2013. p. 966–977.14. Tefferi A. Blood eosinophilia: a new paradigm in disease classification, diagnosis, and treatment. Mayo Clin Proc. 80:75–83. 2005.
Article15. Usatine RP, Sandy N. Dermatologic emergencies. Am Fam Physician. 82:773–780. 2010.16. Wiström J, Norrby SR, Myhre EB, Eriksson S, Granström G, Lagergren L, et al. Frequency of antibiotic-associated diarrhoea in 2462 antibiotictreated hospitalized patients: a prospective study. J Antimicrob Chemother. 47:43–50. 2001.
Article17. Wright J, Paauw DS. Complications of antibiotic therapy. Med Clin North Am. 97:667–679. xi. 2013.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Streptococcus Spondylitis Concomitant Infectious Endocarditis: A Case Report
- Infectious Spondylitis following Kyphoplasty: A case report
- Reverse Latissimus Dorsi Muscle Flap for an Extensive Soft Tissue Defect Accompanied by Infectious Spondylitis
- Epidemiology and management of infectious spondylitis in Korea: a narrative review
- Efficacy and Tolerability of Linezolid for Treatment of Infectious Spondylitis