J Korean Neurosurg Soc.
2012 Oct;52(4):423-426. 10.3340/jkns.2012.52.4.423.
Reverse Latissimus Dorsi Muscle Flap for an Extensive Soft Tissue Defect Accompanied by Infectious Spondylitis
- Affiliations
-
- 1Department of Neurosurgery, Gyeongsang National University School of Medicine, Jinju, Korea. ns4793@hanmail.net
- KMID: 2190666
- DOI: http://doi.org/10.3340/jkns.2012.52.4.423
Abstract
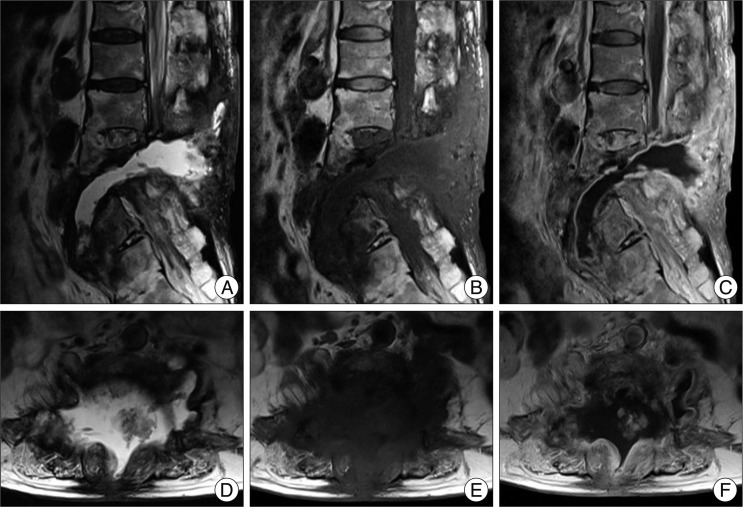
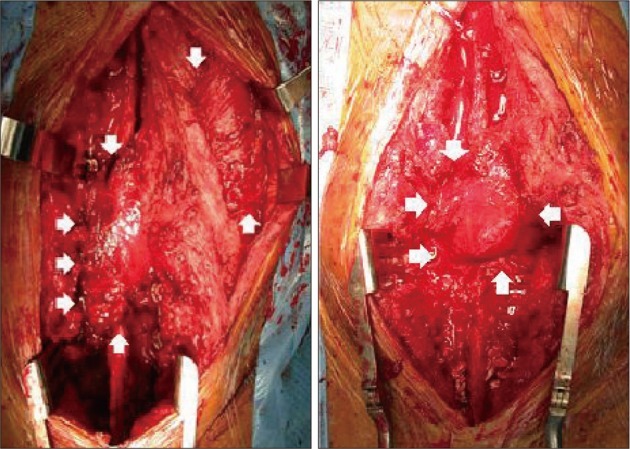
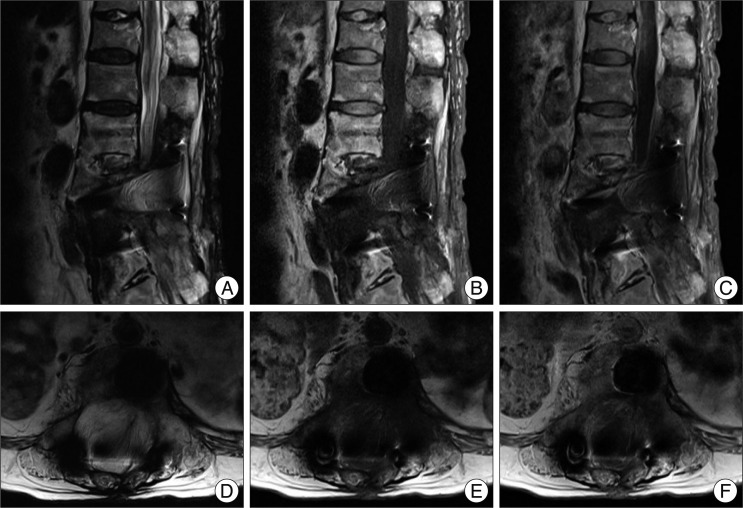
- Spinal infection is an inflammatory process around the vertebral body, and it can extend to the epidural space, posterior elements and paravertebral soft tissues. Infectious spondylitis is a rare infectious disorder, which is often associated with significant neurologic deficits and mortality. When an extensive soft tissue defect is accompanied by infectious spondylitis, effective infection control and proper coverage of soft tissue are directly connected to successful outcomes. However, it is not simple to choose the appropriate treatment methods for infectious spondylitis accompanied by a soft tissue defect. Herein, we report a case of severe infectious spondylitis that was accompanied by an extensive soft tissue defect which was closed with a reverse latissimus muscle flap after traumatic spinal epidural hemorrhage.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Characteristics of Spinal Epidural Abscess Accompanied by Bacteremia
Ho-jun Chae, Jiha Kim, Choonghyo Kim
J Korean Neurosurg Soc. 2021;64(1):88-99. doi: 10.3340/jkns.2020.0278.
Reference
-
1. Casas LA, Lewis VL Jr. A reliable approach to the closure of large acquired midline defects of the back. Plast Reconstr Surg. 1989; 84:632–641. PMID: 2780905.
Article2. Chen HC, Chen HH, Chen WJ, Tang YB. Chronic osteomyelitis of the spine managed with a free flap of latissimus dorsi. A case report. Spine (Phila Pa 1976). 1996; 21:2016–2018. PMID: 8883204.
Article3. Frank CJ, Brantigan J, Cronan J. Bilateral interconnected latissimus dorsi-gluteus maximus muscular cutaneous flaps for closure of subfascial infections in lumbar spinal surgery. A technical note. Spine (Phila Pa 1976). 1997; 22:564–567. PMID: 9076890.
Article4. Garvey PB, Rhines LD, Dong W, Chang DW. Immediate soft-tissue reconstruction for complex defects of the spine following surgery for spinal neoplasms. Plast Reconstr Surg. 2010; 125:1460–1466. PMID: 20134362.
Article5. Hanaoka N, Kawasaki Y, Sakai T, Nakamura T, Nanamori K, Nakamura E, et al. Percutaneous drainage and continuous irrigation in patients with severe pyogenic spondylitis, abscess formation, and marked bone destruction. J Neurosurg Spine. 2006; 4:374–379. PMID: 16703904.
Article6. Hung SJ, Chen HC, Wei FC. Free flaps for reconstruction of the lower back and sacral area. Microsurgery. 2000; 20:72–76. PMID: 10702740.
Article7. Khanna RK, Malik GM, Rock JP, Rosenblum ML. Spinal epidural abscess : evaluation of factors influencing outcome. Neurosurgery. 1996; 39:958–964. PMID: 8905751.
Article8. Klink BK, Thurman RT, Wittpenn GP, Lauerman WC, Cain JE. Muscle flap closure for salvage of complex back wounds. Spine (Phila Pa 1976). 1994; 19:1467–1470. PMID: 7939976.
Article9. Kroll SS, Rosenfield L. Perforator-based flaps for low posterior midline defects. Plast Reconstr Surg. 1988; 81:561–566. PMID: 3279442.
Article10. Manstein ME, Manstein CH, Manstein G. Paraspinous muscle flaps. Ann Plast Surg. 1998; 40:458–462. PMID: 9600427.
Article11. Meiners T, Flieger R, Jungclaus M. Use of the reverse latissimus muscle flap for closure of complex back wounds in patients with spinal cord injury. Spine (Phila Pa 1976). 2003; 28:1893–1898. PMID: 12923481.
Article12. Nagata K, Ohashi T, Ariyoshi M, Sonoda K, Imoto H, Inoue A. Percutaneous suction aspiration and drainage for pyogenic spondylitis. Spine (Phila Pa 1976). 1998; 23:1600–1606. PMID: 9682317.
Article13. Paonessa KJ, Hostnik WJ, Zide BM. Use of tissue expanders for wound closure of spinal infections or dehiscence. Orthop Clin North Am. 1996; 27:155–170. PMID: 8539046.
Article14. Stevenson TR, Rohrich RJ, Pollock RA, Dingman RO, Bostwick J 3rd. More experience with the "reverse" latissimus dorsi musculocutaneous flap : precise location of blood supply. Plast Reconstr Surg. 1984; 74:237–243. PMID: 6463148.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Combined Scapular Flap and Latissimus Dorsi Flap
- Reconstruction of Extensive Lower Extermity Soft Tissue Defect Using Free Latissimus Dorsi Muscle Flap with STSG
- A Combined Scapular Flap and Latissimus Dorsi Flap
- The Benegits of Segnental Latissimus Dorsi Muscle Free Flap
- Reconstruction of an abdominal wall defect using a latissimus dorsi musculocutaneous free flap after high-intensity focused ultrasound: a case report