Allergy Asthma Respir Dis.
2019 Jul;7(3):116-121. 10.4168/aard.2019.7.3.116.
PM(2.5) and pediatric asthma
- Affiliations
-
- 1Department of Pediatrics, Busan St. Mary's Hospital, Busan, Korea. hyh190@naver.com
- KMID: 2461403
- DOI: http://doi.org/10.4168/aard.2019.7.3.116
Abstract
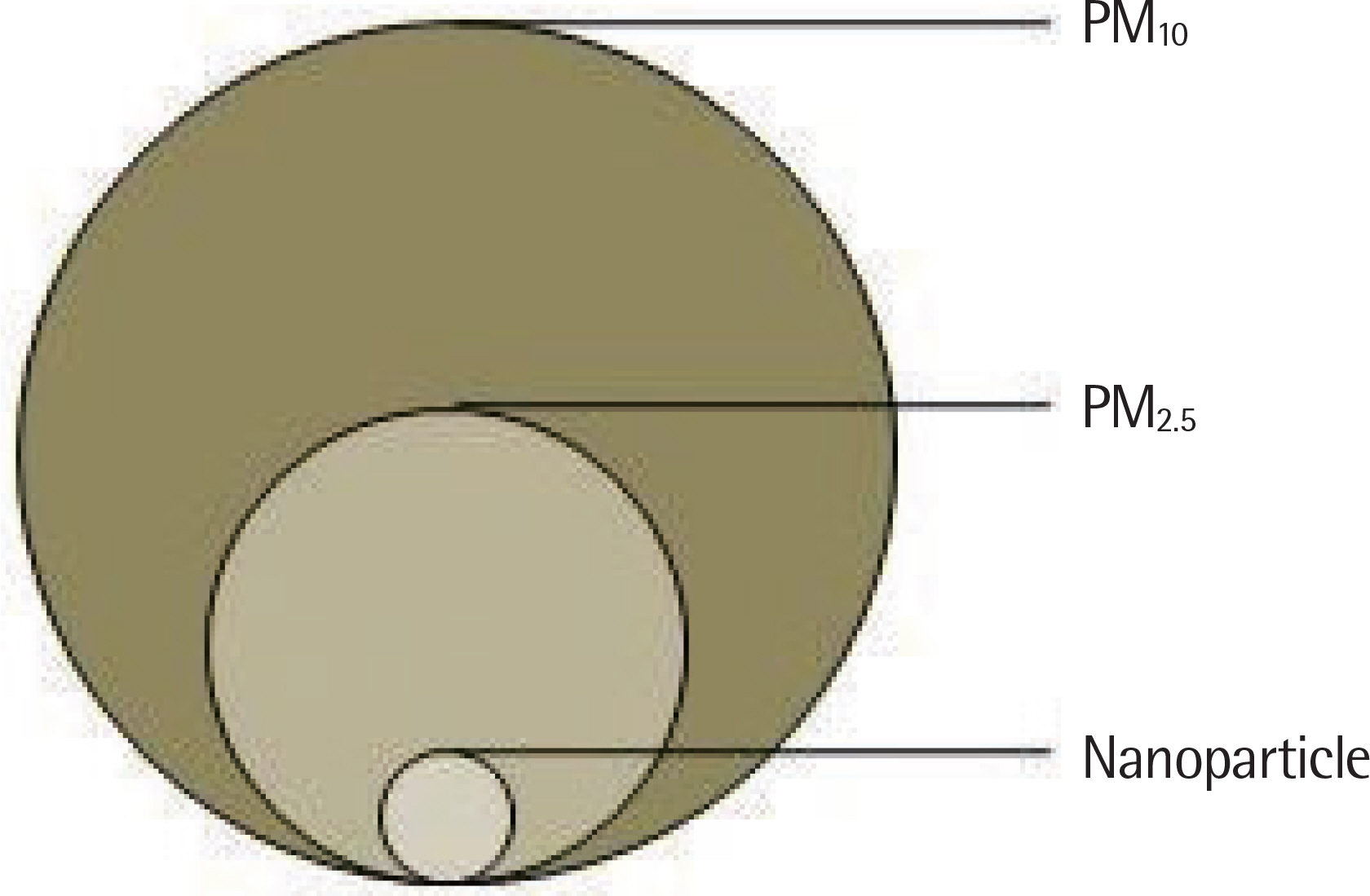
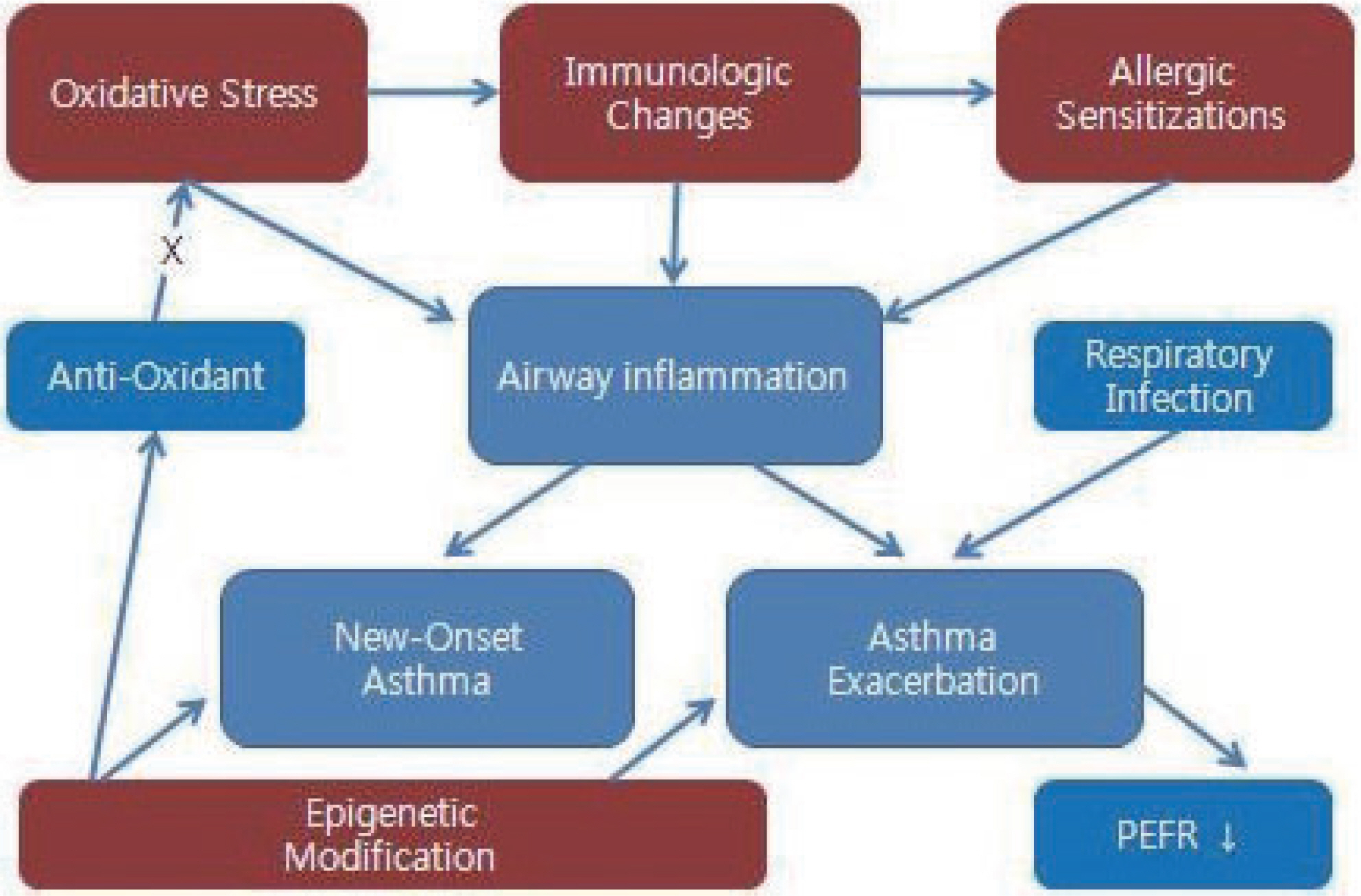
- Air pollution does harm to the respiratory tracts. Fine particulate matter (PM(2.5)) attacks the lung directly passing through mucosal ciliary clearance, causes new-onset asthma, or exacerbates asthma symptoms in children. Oxidative stresses, immunologic changes, allergic sensitization, and epigenetic modification are associated with bronchial asthma. Furthermore, it causes respiratory tract infection and lung function decline. We have to protect the children who are more vulnerable to PM(2.5) than adults. We will investigate individual exposure, influences by the components of air pollution, and genetic susceptibility.
Keyword
MeSH Terms
Figure
Reference
-
References
1. Kelly FJ, Fussell JC. Size, source and chemical composition as determinants of toxicity attributable to ambient particulate matter. Atmos Environ. 2012; 60:504–26.
Article2. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014; 383:1581–92.
Article3. de Kok TM, Driece HA, Hogervorst JG, Briedé JJ. Toxicological assessment of ambient and traffic-related particulate matter: a review of recent studies. Mutat Res. 2006; 613:103–22.
Article4. Bateson TF, Schwartz J. Children's response to air pollutants. J Toxicol Environ Health A. 2008; 71:238–43.
Article5. Miller MD, Marty MA. Impact of environmental chemicals on lung development. Environ Health Perspect. 2010; 118:1155–64.
Article6. Ciencewicki J, Trivedi S, Kleeberger SR. Oxidants and the pathogenesis of lung diseases. J Allergy Clin Immunol. 2008; 122:456–68.
Article7. Li N, Xia T, Nel AE. The role of oxidative stress in ambient particulate matter-induced lung diseases and its implications in the toxicity of engineered nanoparticles. Free Radic Biol Med. 2008; 44:1689–99.
Article8. Gilliland FD, Li YF, Saxon A, Diaz-Sanchez D. Effect of glutathione-S-transferase M1 and P1 genotypes on xenobiotic enhancement of allergic responses: randomised, placebo-controlled crossover study. Lancet. 2004; 363:119–25.
Article9. Patel MM, Chillrud SN, Deepti KC, Ross JM, Kinney PL. Traffic-related air pollutants and exhaled markers of airway inflammation and oxidative stress in New York City adolescents. Environ Res. 2013; 121:71–8.
Article10. Delfino RJ, Staimer N, Gillen D, Tjoa T, Sioutas C, Fung K, et al. Personal and ambient air pollution is associated with increased exhaled nitric oxide in children with asthma. Environ Health Perspect. 2006; 114:1736–43.
Article11. Dales R, Wheeler A, Mahmud M, Frescura AM, Smith-Doiron M, Neth-ery E, et al. The influence of living near roadways on spirometry and exhaled nitric oxide in elementary schoolchildren. Environ Health Perspect. 2008; 116:1423–7.
Article12. Wang P, Thevenot P, Saravia J, Ahlert T, Cormier SA. Radical-containing particles activate dendritic cells and enhance Th17 inflammation in a mouse model of asthma. Am J Respir Cell Mol Biol. 2011; 45:977–83.
Article13. van Voorhis M, Knopp S, Julliard W, Fechner JH, Zhang X, Schauer JJ, et al. Exposure to atmospheric particulate matter enhances Th17 polarization through the aryl hydrocarbon receptor. PLoS One. 2013; 8:e82545.
Article14. Brandt EB, Kovacic MB, Lee GB, Gibson AM, Acciani TH, Le Cras TD, et al. Diesel exhaust particle induction of IL-17A contributes to severe asthma. J Allergy Clin Immunol. 2013; 132:1194–204.e2.15. Rabinovitch N, Jones MJ, Faino A, Strand M, Morin AM, MacIsaac J, et al. Cysteinyl leukotriene receptor 1 and health effects of particulate exposure in asthma. Ann Am Thorac Soc. 2018; 15(Supplement_2):S129.
Article16. Nadeau K, McDonald-Hyman C, Noth EM, Pratt B, Hammond SK, Balmes J, et al. Ambient air pollution impairs regulatory T-cell function in asthma. J Allergy Clin Immunol. 2010; 126:845–52.e10.
Article17. Nel AE, Diaz-Sanchez D, Ng D, Hiura T, Saxon A. Enhancement of allergic inflammation by the interaction between diesel exhaust particles and the immune system. J Allergy Clin Immunol. 1998; 102(4 Pt 1):539–54.
Article18. Diaz-Sanchez D, Garcia MP, Wang M, Jyrala M, Saxon A. Nasal challenge with diesel exhaust particles can induce sensitization to a neoallergen in the human mucosa. J Allergy Clin Immunol. 1999; 104:1183–8.
Article19. Morgenstern V, Zutavern A, Cyrys J, Brockow I, Koletzko S, Krämer U, et al. Atopic diseases, allergic sensitization, and exposure to traffic-related air pollution in children. Am J Respir Crit Care Med. 2008; 177:1331–7.
Article20. Bowatte G, Lodge C, Lowe AJ, Erbas B, Perret J, Abramson MJ, et al. The influence of childhood traffic-related air pollution exposure on asthma, allergy and sensitization: a systematic review and a metaanalysis of birth cohort studies. Allergy. 2015; 70:245–56.
Article21. Gruzieva O, Gehring U, Aalberse R, Agius R, Beelen R, Behrendt H, et al. Meta-analysis of air pollution exposure association with allergic sensitization in European birth cohorts. J Allergy Clin Immunol. 2014; 133:767–76.e7.22. Kelly FJ, Fussell JC. Air pollution and airway disease. Clin Exp Allergy. 2011; 41:1059–71.
Article23. Brunst KJ, Leung YK, Ryan PH, Khurana Hershey GK, Levin L, Ji H, et al. Forkhead box protein 3 (FOXP3) hypermethylation is associated with diesel exhaust exposure and risk for childhood asthma. J Allergy Clin Immunol. 2013; 131:592–4.e1–3.
Article24. Kohli A, Garcia MA, Miller RL, Maher C, Humblet O, Hammond SK, et al. Secondhand smoke in combination with ambient air pollution exposure is associated with increasedx CpG methylation and decreased expression of IFN-γ in T effector cells and Foxp3 in T regulatory cells in children. Clin Epigenetics. 2012; 4:17.
Article25. Dong GH, Chen T, Liu MM, Wang D, Ma YN, Ren WH, et al. Gender differences and effect of air pollution on asthma in children with and without allergic predisposition: northeast Chinese children health study. PLoS One. 2011; 6:e22470.
Article26. Zelikoff JT, Schermerhorn KR, Fang K, Cohen MD, Schlesinger RB. A role for associated transition metals in the immunotoxicity of inhaled ambient particulate matter. Environ Health Perspect. 2002; 110(Suppl 5):871–5.
Article27. Harrod KS, Jaramillo RJ, Berger JA, Gigliotti AP, Seilkop SK, Reed MD. Inhaled diesel engine emissions reduce bacterial clearance and exacerbate lung disease to Pseudomonas aeruginosa infection in vivo. Toxicol Sci. 2005; 83:155–65.
Article28. Lin M, Stieb DM, Chen Y. Coarse particulate matter and hospitalization for respiratory infections in children younger than 15 years in Toronto: a case-crossover analysis. Pediatrics. 2005; 116:e235–40.
Article29. Yang Q, Chen Y, Krewski D, Shi Y, Burnett RT, McGrail KM. Association between particulate air pollution and first hospital admission for child-hood respiratory illness in Vancouver, Canada. Arch Environ Health. 2004; 59:14–21.
Article30. Brauer M, Hoek G, Smit HA, de Jongste JC, Gerritsen J, Postma DS, et al. Air pollution and development of asthma, allergy and infections in a birth cohort. Eur Respir J. 2007; 29:879–88.
Article31. Wong GW, Chow CM. Childhood asthma epidemiology: insights from comparative studies of rural and urban populations. Pediatr Pulmonol. 2008; 43:107–16.
Article32. Robinson CL, Baumann LM, Romero K, Combe JM, Gomez A, Gilman RH, et al. Effect of urbanisation on asthma, allergy and airways inflammation in a developing country setting. Thorax. 2011; 66:1051–7.
Article33. Brunekreef B, Stewart AW, Anderson HR, Lai CK, Strachan DP, Pearce N, et al. Self-reported truck traffic on the street of residence and symptoms of asthma and allergic disease: a global relationship in ISAAC phase 3. Environ Health Perspect. 2009; 117:1791–8.
Article34. Keet CA, Keller JP, Peng RD. Long-term coarse particulate matter exposure is associated with asthma among children in medicaid. Am J Respir Crit Care Med. 2018; 197:737–46.
Article35. Tétreault LF, Doucet M, Gamache P, Fournier M, Brand A, Kosatsky T, et al. Childhood exposure to ambient air pollutants and the onset of asthma: an administrative cohort study in Québec. Environ Health Perspect. 2016; 124:1276–82.
Article36. Zhou C, Baïz N, Zhang T, Banerjee S, Annesi-Maesano I. EDEN Mother-Child Cohort Study Group. Modifiable exposures to air pollutants related to asthma phenotypes in the first year of life in children of the EDEN mother-child cohort study. BMC Public Health. 2013; 13:506.
Article37. Carlsten C, Dybuncio A, Becker A, Chan-Yeung M, Brauer M. Traffic-related air pollution and incident asthma in a high-risk birth cohort. Occup Environ Med. 2011; 68:291–5.
Article38. Clark NA, Demers PA, Karr CJ, Koehoorn M, Lencar C, Tamburic L, et al. Effect of early life exposure to air pollution on development of child-hood asthma. Environ Health Perspect. 2010; 118:284–90.
Article39. Anderson HR, Favarato G, Atkinson RW. Long-term exposure to air pollution and the incidence of asthma: metaanalysis of cohort studies. Air Qual Atmos Health. 2013; 6:47–56.
Article40. Anderson HR, Favarato G, Atkinson RW. Long-term exposure to outdoor air pollution and the prevalence of asthma: metaanalysis of multi-community prevalence studies. Air Qual Atmos Health. 2013; 6:57–68.
Article41. Gowers AM, Cullinan P, Ayres JG, Anderson HR, Strachan DP, Holgate ST, et al. Does outdoor air pollution induce new cases of asthma? Biological plausibility and evidence; a review. Respirology. 2012; 17:887–98.
Article42. Odajima H, Yamazaki S, Nitta H. Decline in peak expiratory flow according to hourly short-term concentration of particulate matter in asthmatic children. Inhal Toxicol. 2008; 20:1263–72.
Article43. Delfino RJ, Staimer N, Tjoa T, Gillen D, Kleinman MT, Sioutas C, et al. Personal and ambient air pollution exposures and lung function decre-ments in children with asthma. Environ Health Perspect. 2008; 116:550–8.
Article44. O'Connor GT, Neas L, Vaughn B, Kattan M, Mitchell H, Crain EF, et al. Acute respiratory health effects of air pollution on children with asthma in US inner cities. J Allergy Clin Immunol. 2008; 121:1133–9.e1.45. Liu L, Poon R, Chen L, Frescura AM, Montuschi P, Ciabattoni G, et al. Acute effects of air pollution on pulmonary function, airway inflammation, and oxidative stress in asthmatic children. Environ Health Perspect. 2009; 117:668–74.
Article46. Tang CS, Chang LT, Lee HC, Chan CC. Effects of personal particulate matter on peak expiratory flow rate of asthmatic children. Sci Total Environ. 2007; 382:43–51.
Article47. Yamazaki S, Shima M, Ando M, Nitta H, Watanabe H, Nishimuta T. Effect of hourly concentration of particulate matter on peak expiratory flow in hospitalized children: a panel study. Environ Health. 2011; 10:15.
Article48. Jacobson Lda S, Hacon Sde S, Castro HA, Ignotti E, Artaxo P, Ponce de Leon AC. Association between fine particulate matter and the peak expiratory flow of schoolchildren in the Brazilian subequatorial Amazon: a panel study. Environ Res. 2012; 117:27–35.49. Mann JK, Balmes JR, Bruckner TA, Mortimer KM, Margolis HG, Pratt B, et al. Short-term effects of air pollution on wheeze in asthmatic children in Fresno, California. Environ Health Perspect. 2010; 118:1497–502.
Article50. Delamater PL, Finley AO, Banerjee S. An analysis of asthma hospitalizations, air pollution, and weather conditions in Los Angeles County, California. Sci Total Environ. 2012; 425:110–8.
Article51. Iskandar A, Andersen ZJ, Bønnelykke K, Ellermann T, Andersen KK, Bisgaard H. Coarse and fine particles but not ultrafine particles in urban air trigger hospital admission for asthma in children. Thorax. 2012; 67:252–7.
Article52. Meng YY, Rull RP, Wilhelm M, Lombardi C, Balmes J, Ritz B. Outdoor air pollution and uncontrolled asthma in the San Joaquin Valley, California. J Epidemiol Community Health. 2010; 64:142–7.
Article53. Silverman RA, Ito K. Age-related association of fine particles and ozone with severe acute asthma in New York City. J Allergy Clin Immunol. 2010; 125:367–73.e5.
Article54. Neidell M. Air quality warnings and outdoor activities: evidence from Southern California using a regression discontinuity design. J Epidemiol Community Health. 2010; 64:921–6.
Article55. McLaren J, Williams ID. The impact of communicating information about air pollution events on public health. Sci Total Environ. 2015; 538:478–91.
Article56. Friedman MS, Powell KE, Hutwagner L, Graham LM, Teague WG. Impact of changes in transportation and commuting behaviors during the 1996 Summer Olympic Games in Atlanta on air quality and childhood asthma. JAMA. 2001; 285:897–905.
Article57. Chen BY, Chen CH, Chuang YC, Wu YH, Pan SC, Guo YL. Changes in the relationship between childhood asthma and ambient air pollution in Taiwan: results from a nationwide survey repeated 5 years apart. Pediatr Allergy Immunol. 2019; 30:188–94.58. West JJ, Smith SJ, Silva RA, Naik V, Zhang Y, Adelman Z, et al. Co-bene-fits of global greenhouse gas mitigation for future air quality and human health. Nat Clim Chang. 2013; 3:885–9.59. von Klot S, Wölke G, Tuch T, Heinrich J, Dockery DW, Schwartz J, et al. Increased asthma medication use in association with ambient fine and ultrafine particles. Eur Respir J. 2002; 20:691–702.60. Delfino RJ, Zeiger RS, Seltzer JM, Street DH, McLaren CE. Association of asthma symptoms with peak particulate air pollution and effect modification by anti-inflammatory medication use. Environ Health Perspect. 2002; 110:A607–17.
Article61. Hasunuma H, Yamazaki S, Tamura K, Hwang YH, Ono R, Amimoto Y, et al. Association between daily ambient air pollution and respiratory symptoms in children with asthma and healthy children in western Japan. J Asthma. 2018; 55:712–9.
Article62. Williams AM, Phaneuf DJ, Barrett MA, Su JG. Short-term impact of PM(2.5) on contemporaneous asthma medication use: behavior and the value of pollution reductions. Proc Natl Acad Sci U S A. 2019; 116:5246–53.63. Jhun I, Gaffin JM, Coull BA, Huffaker MF, Petty CR, Sheehan WJ, et al. School environmental intervention to reduce particulate pollutant exposures for children with asthma. J Allergy Clin Immunol Pract. 2017; 5:154–9.e3.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Particulate Matter and Bronchial Asthma
- Particulate matter and childhood allergic diseases
- Biomarkers of the relationship of particulate matter exposure with the progression of chronic respiratory diseases
- Particulate-Matter Related Respiratory Diseases
- Association between Time of Injury and Injury Severity after Pediatric Pedestrian Injury