Tuberc Respir Dis.
2019 Oct;82(4):319-327. 10.4046/trd.2018.0082.
Diagnostic Performance of Radial Probe Endobronchial Ultrasound without a Guide-Sheath and the Feasibility of Molecular Analysis
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kj2011.lee@samsung.com
- KMID: 2459056
- DOI: http://doi.org/10.4046/trd.2018.0082
Abstract
- BACKGROUND
Radial probe endobronchial ultrasound (R-EBUS), is effective for tissue diagnosis of lung lesions. We evaluated the diagnostic performance of R-EBUS both a guide-sheath and fluoroscopy and identified factors associated with accurate diagnosis. The feasibility of molecular and genetic testing, using specimens obtained by R-EBUS, was also investigated.
METHODS
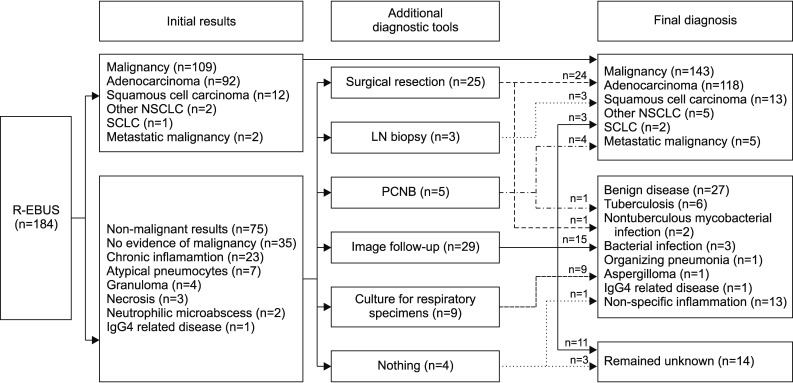
The study retrospectively reviewed 211 patients undergoing R-EBUS without a guide-sheath and fluoroscopy, June 2016-May 2017. After excluding 27 patients of which the target lesion was not reached, 184 were finally included. Multivariate logistic regression was used, to identify factors associated with accurate diagnosis.
RESULTS
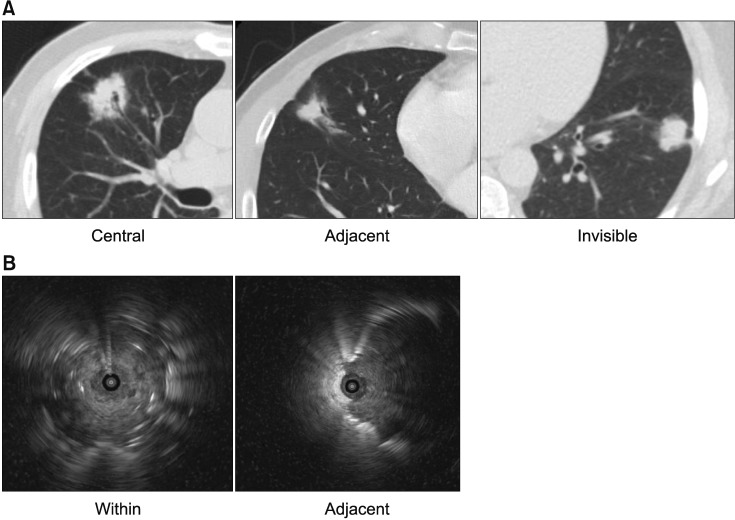
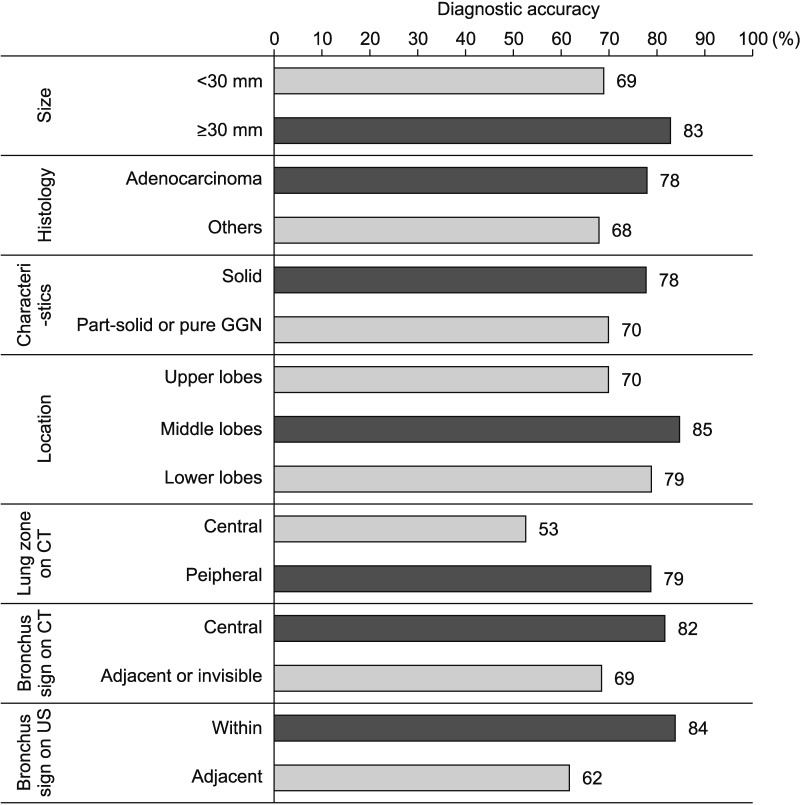
Among 184 patients, R-EBUS-guided biopsy diagnosed malignancy in 109 patients (59%). The remaining 75 patients (41%) with non-malignant results underwent additional work-ups, and 34 were diagnosed with malignancy. Based on final diagnosis, diagnostic accuracy was 80% (136/170), and sensitivity and specificity for malignancy were 76% (109/143) and 100% (27/27), respectively. In multivariate analysis, peripheral location (adjusted odds ratio [aOR], 3.925; 95% confidence interval [CI], 1.203-12.811; p=0.023), and central position of the probe (aOR, 2.435; 95% CI, 1.424-7.013; p=0.035), were associated with accurate diagnosis of malignancy. Molecular and genetic analyses were successful, in all but one case, with inadequate specimens.
CONCLUSION
R-EBUS-guided biopsy without equipment, is effective for tissue diagnosis. Peripheral location and central position of the radial probe, were crucial for accurate diagnosis. Performance of molecular and genetic testing, using samples obtained by R-EBUS, was satisfactory.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Utility of Radial Probe Endobronchial Ultrasound Guided Transbronchial Lung Biopsy in Bronchus Sign Negative Peripheral Pulmonary Lesions
Kyung Soo Hong, Kwan Ho Lee, Jin Hong Chung, Kyeong-Cheol Shin, Hyun Jung Jin, Jong Geol Jang, June Hong Ahn
J Korean Med Sci. 2021;36(24):e176. doi: 10.3346/jkms.2021.36.e176.An update on the role of bronchoscopy in the diagnosis of pulmonary disease
June Hong Ahn
Yeungnam Univ J Med. 2020;37(4):253-261. doi: 10.12701/yujm.2020.00584.
Reference
-
1. Politi K, Herbst RS. Lung cancer in the era of precision medicine. Clin Cancer Res. 2015; 21:2213–2220. PMID: 25979927.
Article2. Folch E, Costa DB, Wright J, VanderLaan PA. Lung cancer diagnosis and staging in the minimally invasive age with increasing demands for tissue analysis. Transl Lung Cancer Res. 2015; 4:392–403. PMID: 26380180.3. Baaklini WA, Reinoso MA, Gorin AB, Sharafkaneh A, Manian P. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest. 2000; 117:1049–1054. PMID: 10767238.
Article4. Gildea TR, Mazzone PJ, Karnak D, Meziane M, Mehta AC. Electromagnetic navigation diagnostic bronchoscopy: a prospective study. Am J Respir Crit Care Med. 2006; 174:982–989. PMID: 16873767.5. Ishida T, Asano F, Yamazaki K, Shinagawa N, Oizumi S, Moriya H, et al. Virtual bronchoscopic navigation combined with endobronchial ultrasound to diagnose small peripheral pulmonary lesions: a randomised trial. Thorax. 2011; 66:1072–1077. PMID: 21749984.
Article6. Chen A, Chenna P, Loiselle A, Massoni J, Mayse M, Misselhorn D. Radial probe endobronchial ultrasound for peripheral pulmonary lesions: a 5-year institutional experience. Ann Am Thorac Soc. 2014; 11:578–582. PMID: 24635641.
Article7. Chenna P, Chen AC. Radial probe endobronchial ultrasound and novel navigation biopsy techniques. Semin Respir Crit Care Med. 2014; 35:645–654. PMID: 25463156.
Article8. Anantham D, Koh MS, Ernst A. Endobronchial ultrasound. Respir Med. 2009; 103:1406–1414. PMID: 19447014.
Article9. Ali MS, Trick W, Mba BI, Mohananey D, Sethi J, Musani AI. Radial endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions: a systematic review and metaanalysis. Respirology. 2017; 22:443–453. PMID: 28177181.
Article10. Steinfort DP, Khor YH, Manser RL, Irving LB. Radial probe endobronchial ultrasound for the diagnosis of peripheral lung cancer: systematic review and meta-analysis. Eur Respir J. 2011; 37:902–910. PMID: 20693253.
Article11. Fuso L, Varone F, Magnini D, Baldi F, Rindi G, Pagliari G, et al. Role of ultrasound-guided transbronchial biopsy in the diagnosis of peripheral pulmonary lesions. Lung Cancer. 2013; 81:60–64. PMID: 23639784.
Article12. Evison M, Crosbie PA, Morris J, Martin J, Barber PV, Booton R. Can computed tomography characteristics predict outcomes in patients undergoing radial endobronchial ultrasound-guided biopsy of peripheral lung lesions. J Thorac Oncol. 2014; 9:1393–1397. PMID: 25122434.
Article13. Wang Y, Mei Q, Ai YQ, Li RQ, Chang L, Li YF, et al. Identification of lung cancer oncogenes based on the mRNA expression and single nucleotide polymorphism profile data. Neoplasma. 2015; 62:966–973. PMID: 26458310.
Article14. Yamada N, Yamazaki K, Kurimoto N, Asahina H, Kikuchi E, Shinagawa N, et al. Factors related to diagnostic yield of transbronchial biopsy using endobronchial ultrasonography with a guide sheath in small peripheral pulmonary lesions. Chest. 2007; 132:603–608. PMID: 17573504.
Article15. Minezawa T, Okamura T, Yatsuya H, Yamamoto N, Morikawa S, Yamaguchi T, et al. Bronchus sign on thin-section computed tomography is a powerful predictive factor for successful transbronchial biopsy using endobronchial ultrasound with a guide sheath for small peripheral lung lesions: a retrospective observational study. BMC Med Imaging. 2015; 15:21. PMID: 26092497.
Article16. Eberhardt R, Ernst A, Herth FJ. Ultrasound-guided transbronchial biopsy of solitary pulmonary nodules less than 20 mm. Eur Respir J. 2009; 34:1284–1287. PMID: 19460785.
Article17. Izumo T, Sasada S, Chavez C, Matsumoto Y, Hayama M, Tsuchida T. The diagnostic value of histology and cytology samples during endobronchial ultrasound with a guide sheath. Jpn J Clin Oncol. 2015; 45:362–366. PMID: 25628350.
Article18. Yoshikawa M, Sukoh N, Yamazaki K, Kanazawa K, Fukumoto S, Harada M, et al. Diagnostic value of endobronchial ultrasonography with a guide sheath for peripheral pulmonary lesions without X-ray fluoroscopy. Chest. 2007; 131:1788–1793. PMID: 17565021.
Article19. Chan A, Devanand A, Low SY, Koh MS. Radial endobronchial ultrasound in diagnosing peripheral lung lesions in a high tuberculosis setting. BMC Pulm Med. 2015; 15:90. PMID: 26285821.
Article20. Casutt A, Prella M, Beigelman-Aubry C, Fitting JW, Nicod L, Koutsokera A, et al. Fluoroscopic-guided radial endobronchial ultrasound without guide sheath for peripheral pulmonary lesions: a safe and efficient combination. Arch Bronconeumol. 2015; 51:338–343. PMID: 25769444.
Article21. Haidong H, Yunye N, Wei Z, Zarogoulidis P, Hohenforst-Schmidt W, Man YG, et al. Multiple guided technologies based on radial probe endobronchial ultrasound for the diagnosis of solitary peripheral pulmonary lesions: a single-center study. J Cancer. 2017; 8:3514–3521. PMID: 29151936.
Article22. Zhang SJ, Zhang M, Zhou J, Zhang QD, Xu QQ, Xu X. Comparison of radial endobronchial ultrasound with a guide sheath and with distance by thin bronchoscopy for the diagnosis of peripheral pulmonary lesions: a prospective randomized crossover trial. J Thorac Dis. 2016; 8:3112–3118. PMID: 28066590.23. Zhang SJ, Zhang M, Zhou J, Zhang QD, Xu QQ, Xu X. Radial endobronchial ultrasonography with distance measurement through a thin bronchoscope for the diagnosis of malignant peripheral pulmonary lesions. Transl Lung Cancer Res. 2018; 7:80–87. PMID: 29535914.
Article24. Steinfort DP, Vincent J, Heinze S, Antippa P, Irving LB. Comparative effectiveness of radial probe endobronchial ultrasound versus CT-guided needle biopsy for evaluation of peripheral pulmonary lesions: a randomized pragmatic trial. Respir Med. 2011; 105:1704–1711. PMID: 21875783.
Article25. Xu CH, Yuan Q, Yu LK, Wang W, Lin Y. Endobronchial ultrasound transbronchial biopsy with guide-sheath for the diagnosis of solitary pulmonary nodules. Oncotarget. 2017; 8:58272–58277. PMID: 28938554.
Article26. Kuo CH, Lin SM, Lee KY, Chung FT, Lo YL, Hsiung TC, et al. Endobronchial ultrasound-guided transbronchial biopsy and brushing: a comparative evaluation for the diagnosis of peripheral pulmonary lesions. Eur J Cardiothorac Surg. 2014; 45:894–898. PMID: 24078100.
Article27. Gex G, Pralong JA, Combescure C, Seijo L, Rochat T, Soccal PM. Diagnostic yield and safety of electromagnetic navigation bronchoscopy for lung nodules: a systematic review and meta-analysis. Respiration. 2014; 87:165–176. PMID: 24401166.
Article28. Asano F, Eberhardt R, Herth FJ. Virtual bronchoscopic navigation for peripheral pulmonary lesions. Respiration. 2014; 88:430–440. PMID: 25402610.
Article29. Tachihara M, Ishida T, Kanazawa K, Sugawara A, Watanabe K, Uekita K, et al. A virtual bronchoscopic navigation system under X-ray fluoroscopy for transbronchial diagnosis of small peripheral pulmonary lesions. Lung Cancer. 2007; 57:322–327. PMID: 17532538.
Article30. Iwano S, Imaizumi K, Okada T, Hasegawa Y, Naganawa S. Virtual bronchoscopy-guided transbronchial biopsy for aiding the diagnosis of peripheral lung cancer. Eur J Radiol. 2011; 79:155–159. PMID: 20022191.
Article31. Asano F, Shinagawa N, Ishida T, Shindoh J, Anzai M, Tsuzuku A, et al. Virtual bronchoscopic navigation combined with ultrathin bronchoscopy. A randomized clinical trial. Am J Respir Crit Care Med. 2013; 188:327–333. PMID: 23600452.
Article32. Ozgul G, Cetinkaya E, Ozgul MA, Abul Y, Gencoglu A, Kamiloglu E, et al. Efficacy and safety of electromagnetic navigation bronchoscopy with or without radial endobronchial ultrasound for peripheral lung lesions. Endosc Ultrasound. 2016; 5:189–195. PMID: 27386477.
Article33. Georgiou HD, Taverner J, Irving LB, Steinfort DP. Safety and efficacy of radial EBUS for the investigation of peripheral pulmonary lesions in patients with advanced COPD. J Bronchology Interv Pulmonol. 2016; 23:192–198. PMID: 27454473.
Article34. Jurado J, Saqi A, Maxfield R, Newmark A, Lavelle M, Bacchetta M, et al. The efficacy of EBUS-guided transbronchial needle aspiration for molecular testing in lung adenocarcinoma. Ann Thorac Surg. 2013; 96:1196–1202. PMID: 23972930.
Article35. Khandhar SJ, Bowling MR, Flandes J, Gildea TR, Hood KL, Krimsky WS, et al. Electromagnetic navigation bronchoscopy to access lung lesions in 1,000 subjects: first results of the prospective, multicenter NAVIGATE study. BMC Pulm Med. 2017; 17:59. PMID: 28399830.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The diagnosis of peripheral lung lesions: transbronchial biopsy using a radial probe endobronchial ultrasound
- Radial Probe Endobronchial Ultrasound Using Guide Sheath-Guided Transbronchial Lung Biopsy in Peripheral Pulmonary Lesions without Fluoroscopy
- Utility of Radial Probe Endobronchial Ultrasound Guided Transbronchial Lung Biopsy in Bronchus Sign Negative Peripheral Pulmonary Lesions
- Utility of Radial Probe Endobronchial Ultrasound-Guided Transbronchial Lung Biopsy in Diffuse Lung Lesions
- Development of the Korean Association for Lung Cancer Clinical Practice Guidelines: Recommendations on Radial Probe Endobronchial Ultrasound for Diagnosing Lung Cancer - An Updated Meta-Analysis