J Korean Med Sci.
2021 Jun;36(24):e176. 10.3346/jkms.2021.36.e176.
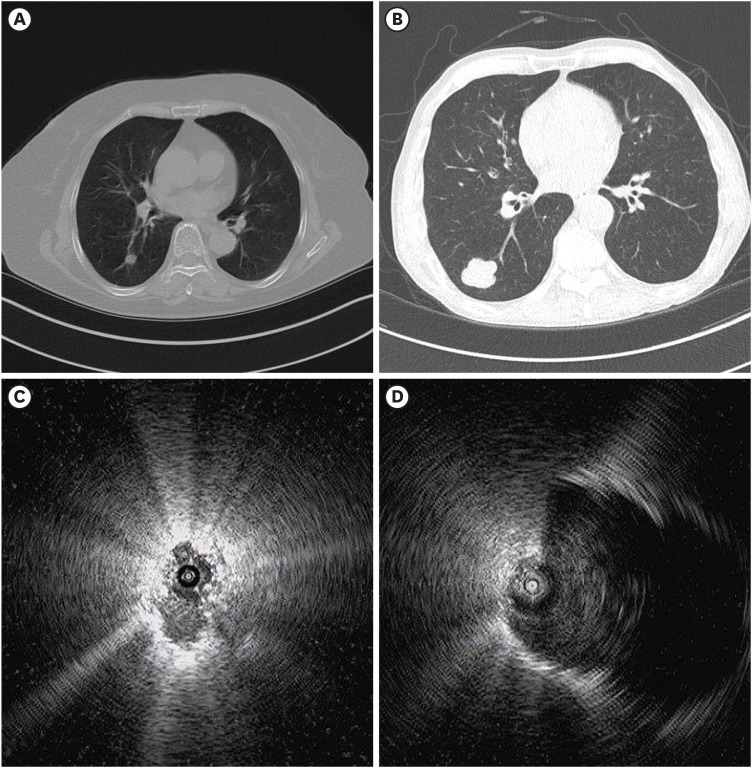
Utility of Radial Probe Endobronchial Ultrasound Guided Transbronchial Lung Biopsy in Bronchus Sign Negative Peripheral Pulmonary Lesions
- Affiliations
-
- 1Division of Pulmonology and Allergy, Department of Internal Medicine, College of Medicine, Yeungnam University and Respiratory Center, Yeungnam University Medical Center, Daegu, Korea
- KMID: 2516766
- DOI: http://doi.org/10.3346/jkms.2021.36.e176
Abstract
- Background
The presence of the bronchus sign on chest computed tomography is associated with an increased diagnostic yield of radial probe endobronchial ultrasound– guided transbronchial lung biopsy (RP-EBUS-TBLB). However, the utility of RP-EBUS-TBLB for bronchus sign negative peripheral pulmonary lesions (PPLs) remains unknown. We investigated the utility of RP-EBUS-TBLB in bronchus sign negative PPLs.
Methods
We retrospectively reviewed data from 109 patients who underwent RP-EBUS for bronchus sign negative PPLs from January 2019 to August 2020. TBLB was performed using RP-EBUS with a guide sheath and without fluoroscopy. The EBUS visualization and TBLB diagnostic yields were assessed. Multivariable logistic regression analyses were used to identify factors affecting the EBUS visualization and diagnostic yields.
Results
The EBUS visualization yield was 74.1% (68/109). Of the 109 lung lesions, 92 were definitively diagnosed. The overall diagnostic accuracy, sensitivity, specificity, positive predictive value, and negative predictive value were 50.5% (55/109), 34.9% (29/83), 100% (26/26), 100% (29/29), and 32.5% (26/80), respectively. In multivariable analyses, the size of the lesion (≥ 20 mm; odds ratio [OR], 2.62; 95% confidence interval [CI], 1.16–5.93; P = 0.021) and the distance from the pleura (> 10 mm; OR, 2.37; 95% CI, 1.02–5.52; P = 0.045) were associated with EBUS visualization. Regarding diagnostic yield, having the probe within the lesion (OR, 28.50; 95% CI, 6.26–129.85; P < 0.001) and a solid lesion (OR, 14.58; 95% CI, 2.64–80.38; P = 0.002) were associated with diagnostic success. Pneumothorax and hemoptysis occurred in 3.7% (4/109) and 0.9% (1/109), respectively, of the patients.
Conclusion
RP-EBUS-TBLB using a GS can be considered a diagnostic method in bronchus sign negative solid PPLs. Having the probe within the lesion and a solid lesion were important for diagnostic success. Complication rates were acceptable.
Keyword
Figure
Reference
-
1. Ahn JH. An update on the role of bronchoscopy in the diagnosis of pulmonary disease. Yeungnam Univ J Med. 2020; 37(4):253–261. PMID: 32891075.
Article2. Anantham D, Koh MS, Ernst A. Endobronchial ultrasound. Respir Med. 2009; 103(10):1406–1414. PMID: 19447014.
Article3. Kurimoto N, Miyazawa T, Okimasa S, Maeda A, Oiwa H, Miyazu Y, et al. Endobronchial ultrasonography using a guide sheath increases the ability to diagnose peripheral pulmonary lesions endoscopically. Chest. 2004; 126(3):959–965. PMID: 15364779.
Article4. Steinfort DP, Khor YH, Manser RL, Irving LB. Radial probe endobronchial ultrasound for the diagnosis of peripheral lung cancer: systematic review and meta-analysis. Eur Respir J. 2011; 37(4):902–910. PMID: 20693253.
Article5. Ali MS, Trick W, Mba BI, Mohananey D, Sethi J, Musani AI. Radial endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions: a systematic review and meta-analysis. Respirology. 2017; 22(3):443–453. PMID: 28177181.
Article6. Chen CH, Cheng WC, Wu BR, Chen CY, Chen WC, Hsia TC, et al. Improved diagnostic yield of bronchoscopy in peripheral pulmonary lesions: combination of radial probe endobronchial ultrasound and rapid on-site evaluation. J Thorac Dis. 2015; 7(Suppl 4):S418–S425. PMID: 26807290.7. Moon SM, Choe J, Jeong BH, Um SW, Kim H, Kwon OJ, et al. Diagnostic performance of radial probe endobronchial ultrasound without a guide-sheath and the feasibility of molecular analysis. Tuberc Respir Dis (Seoul). 2019; 82(4):319–327. PMID: 31172704.
Article8. Asano F, Eberhardt R, Herth FJ. Virtual bronchoscopic navigation for peripheral pulmonary lesions. Respiration. 2014; 88(5):430–440. PMID: 25402610.
Article9. Minezawa T, Okamura T, Yatsuya H, Yamamoto N, Morikawa S, Yamaguchi T, et al. Bronchus sign on thin-section computed tomography is a powerful predictive factor for successful transbronchial biopsy using endobronchial ultrasound with a guide sheath for small peripheral lung lesions: a retrospective observational study. BMC Med Imaging. 2015; 15(1):21. PMID: 26092497.
Article10. Tay JH, Irving L, Antippa P, Steinfort DP. Radial probe endobronchial ultrasound: factors influencing visualization yield of peripheral pulmonary lesions. Respirology. 2013; 18(1):185–190. PMID: 23035636.
Article11. Evison M, Crosbie PA, Morris J, Martin J, Barber PV, Booton R. Can computed tomography characteristics predict outcomes in patients undergoing radial endobronchial ultrasound-guided biopsy of peripheral lung lesions? J Thorac Oncol. 2014; 9(9):1393–1397. PMID: 25122434.
Article12. Park S, Yoon HY, Han Y, Wang KS, Park SY, Ryu YJ, et al. Diagnostic yield of additional conventional transbronchial lung biopsy following radial endobronchial ultrasound lung biopsy for peripheral pulmonary lesions. Thorac Cancer. 2020; 11(6):1639–1646. PMID: 32342673.
Article13. Ali MS, Sethi J, Taneja A, Musani A, Maldonado F. Computed tomography bronchus sign and the diagnostic yield of guided bronchoscopy for peripheral pulmonary lesions. A systematic review and meta-analysis. Ann Am Thorac Soc. 2018; 15(8):978–987. PMID: 29877715.
Article14. Chen AC, Loiselle A, Zhou L, Baty J, Misselhorn D. Localization of peripheral pulmonary lesions using a method of computed tomography-anatomic correlation and radial probe endobronchial ultrasound confirmation. Ann Am Thorac Soc. 2016; 13(9):1586–1592. PMID: 27388116.
Article15. Lee KM, Lee G, Kim A, Mok J, Lee JW, Jeong YJ, et al. Clinical outcomes of radial probe endobronchial ultrasound using a guide sheath for diagnosis of peripheral lung lesions in patients with pulmonary emphysema. Respir Res. 2019; 20(1):177. PMID: 31387600.
Article16. Good WR, Christensen PM, Herath S, Dawkins P, Yap E. Radial-probe endobronchial ultrasound outcomes in the investigation of peripheral pulmonary lesions: a New Zealand perspective. Intern Med J. 2018; 48(12):1481–1487. PMID: 30091278.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Utility of Radial Probe Endobronchial Ultrasound-Guided Transbronchial Lung Biopsy in Diffuse Lung Lesions
- Radial Probe Endobronchial Ultrasound Using Guide Sheath-Guided Transbronchial Lung Biopsy in Peripheral Pulmonary Lesions without Fluoroscopy
- The diagnosis of peripheral lung lesions: transbronchial biopsy using a radial probe endobronchial ultrasound
- Development of the Korean Association for Lung Cancer Clinical Practice Guidelines: Recommendations on Radial Probe Endobronchial Ultrasound for Diagnosing Lung Cancer - An Updated Meta-Analysis
- Technical Aspects of Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration