Cancer Res Treat.
2024 Apr;56(2):464-483. 10.4143/crt.2023.749.
Development of the Korean Association for Lung Cancer Clinical Practice Guidelines: Recommendations on Radial Probe Endobronchial Ultrasound for Diagnosing Lung Cancer - An Updated Meta-Analysis
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea
- 2Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 3Division of Pulmonology, National Cancer Center, Goyang, Korea
- 4Department of Biostatistics, Pusan National University Hospital, Busan, Korea
- 5Department of Internal Medicine, Dong-A University Hospital, Busan, Korea
- KMID: 2554337
- DOI: http://doi.org/10.4143/crt.2023.749
Abstract
- Purpose
Radial probe endobronchial ultrasound (RP-EBUS) accurately locates peripheral lung lesions (PLLs) during transbronchial biopsy (TBB). We performed an updated meta-analysis of the diagnostic yield of TBB for PLLs using RP-EBUS to generate recommendations for the development of the Korean Association of Lung Cancer guidelines.
Materials and Methods
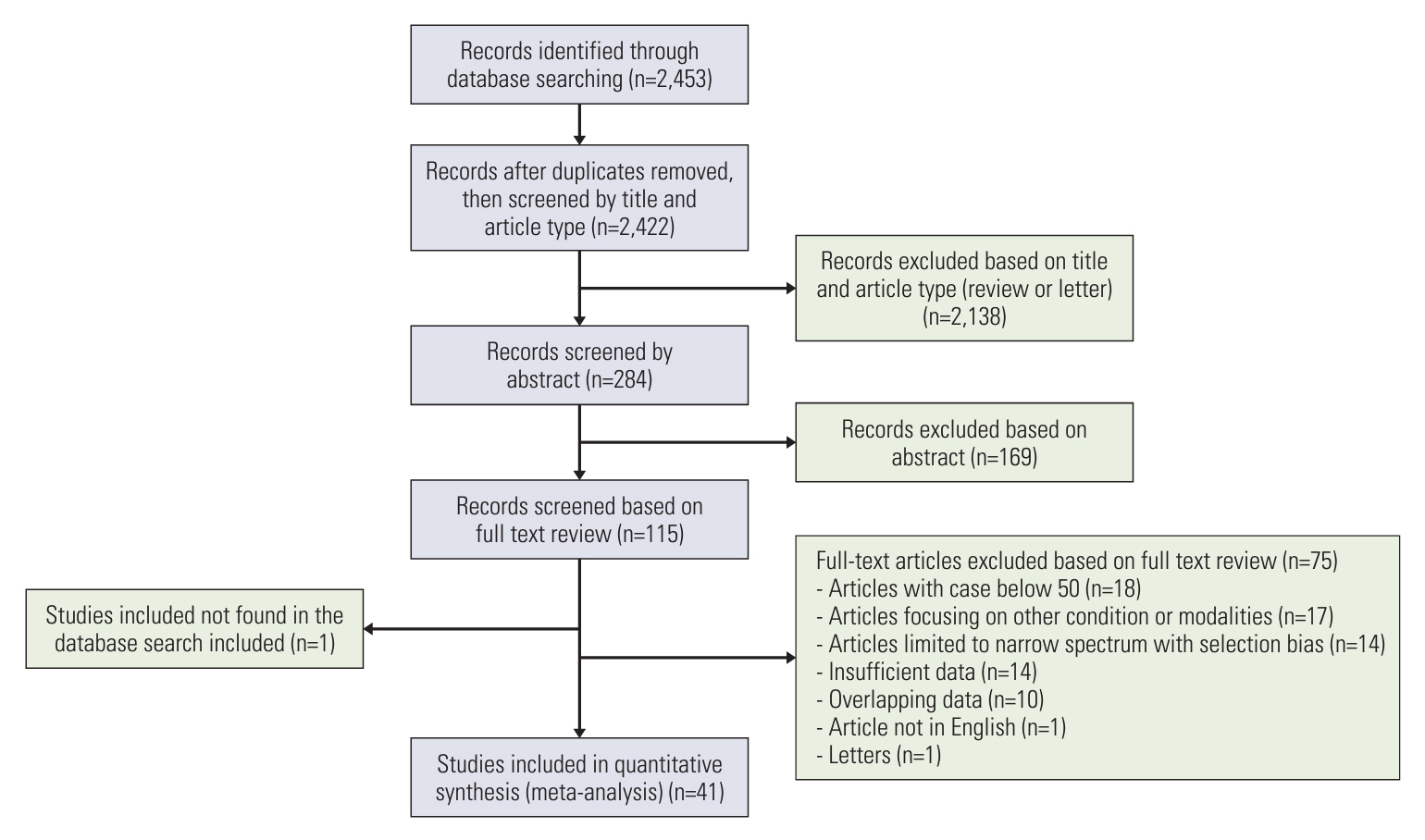
We systematically searched MEDLINE and EMBASE (from January 2013 to December 2022), and performed a meta-analysis using R software. The diagnostic yield was evaluated by dividing the number of successful diagnoses by the total lesion number. Subgroup analysis was performed to identify related factors.
Results
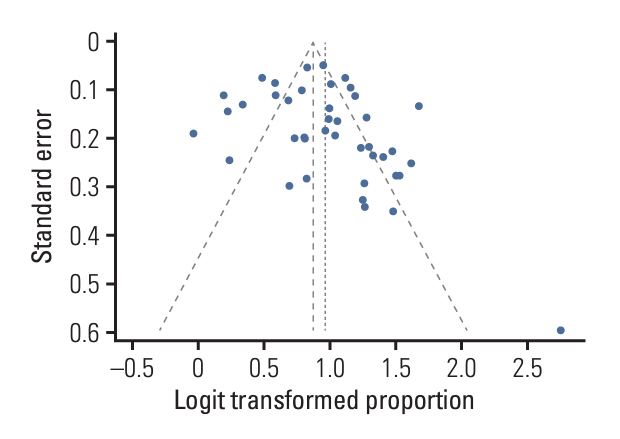
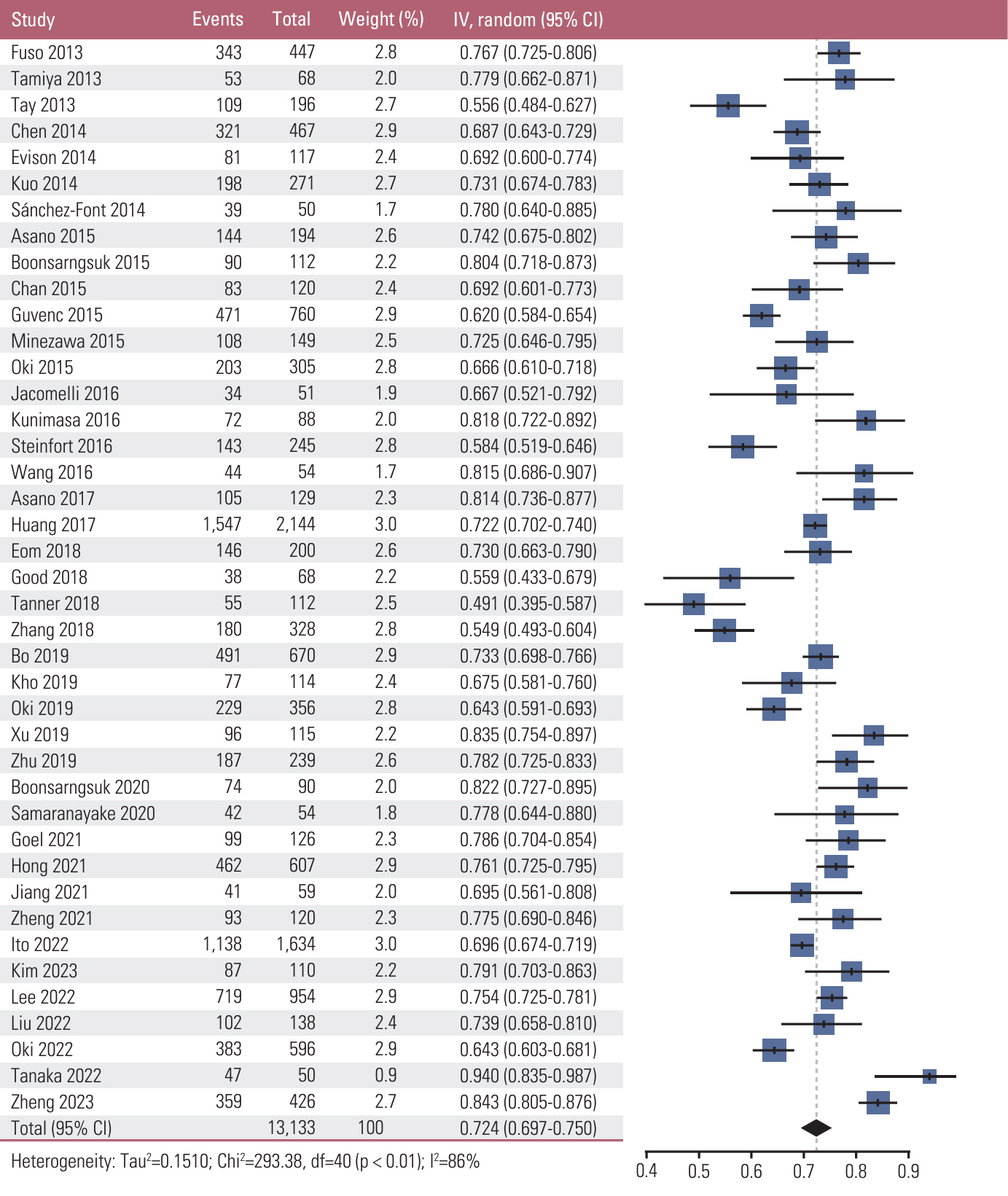
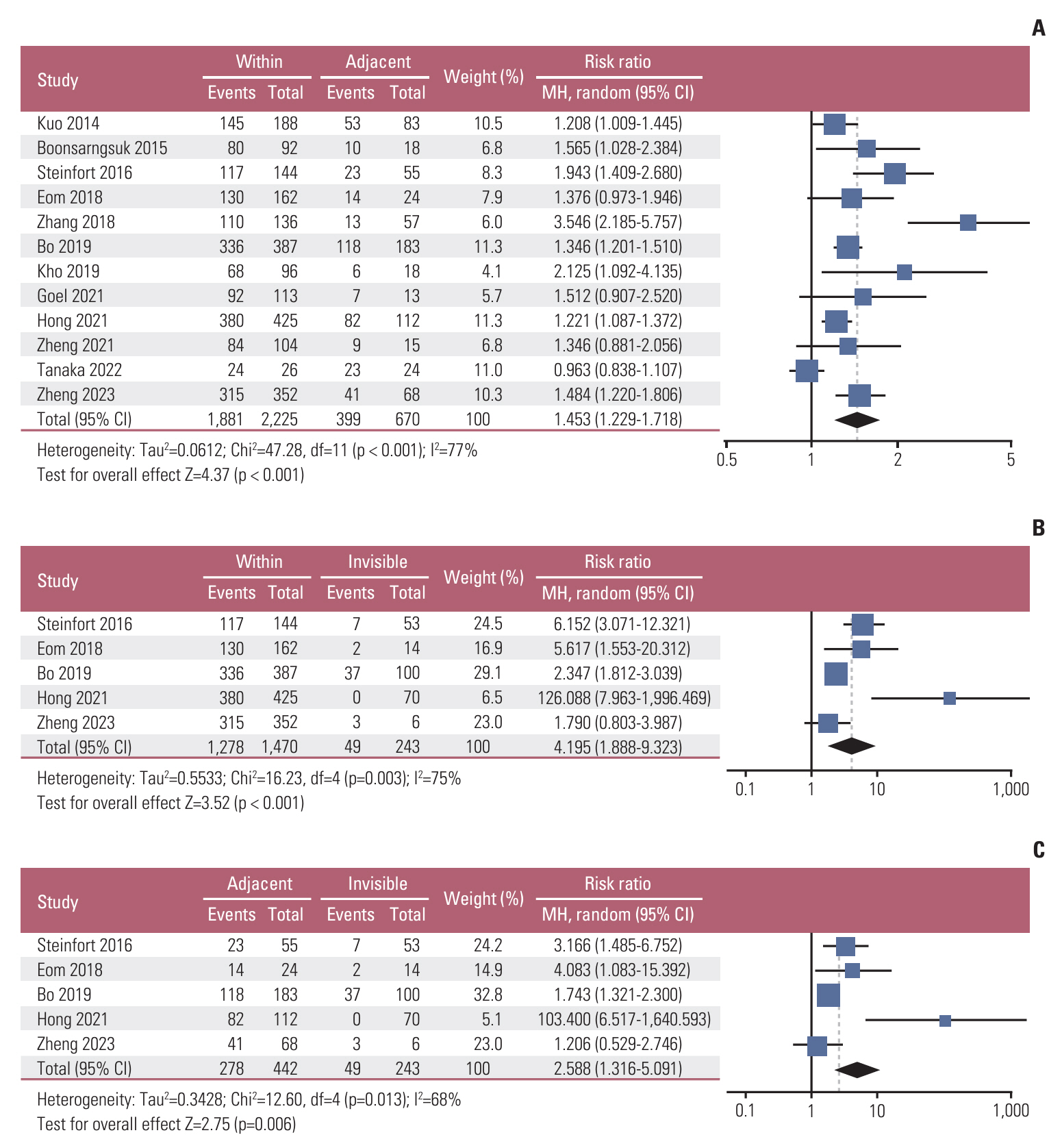
Forty-one studies with a total of 13,133 PLLs were included. The pooled diagnostic yield of RP-EBUS was 0.72 (95% confidence interval [CI], 0.70 to 0.75). Significant heterogeneity was observed among studies (χ2=292.38, p < 0.01, I2=86.4%). In a subgroup analysis, there was a significant difference in diagnostic yield based on RP-EBUS findings (within, adjacent to, invisible), with a risk ratio of 1.45 (95% CI, 1.23 to 1.72) between within and adjacent to, 4.20 (95% CI, 1.89 to 9.32) between within and invisible, and 2.59 (95% CI, 1.32 to 5.01) between adjacent to and invisible. There was a significant difference in diagnostic yield based on lesion size, histologic diagnosis, computed tomography (CT) bronchus sign, lesion character, and location from the hilum. The overall complication rate of TBB with RP-EBUS was 6.8% (bleeding, 4.5%; pneumothorax, 1.4%).
Conclusion
Our study showed that TBB with RP-EBUS is an accurate diagnostic tool for PLLs with good safety profiles, especially for PLLs with within orientation on RP-EBUS or positive CT bronchus sign.
Keyword
Figure
Reference
-
References
1. Gould MK, Tang T, Liu IL, Lee J, Zheng C, Danforth KN, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015; 192:1208–14.
Article2. National Lung Screening Trial Research Team, Church TR, Black WC, Aberle DR, Berg CD, Clingan KL, et al. Results of initial low-dose computed tomographic screening for lung cancer. N Engl J Med. 2013; 368:1980–91.
Article3. Gould MK, Donington J, Lynch WR, Mazzone PJ, Midthun DE, Naidich DP, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143:e93S–120S.4. Kim SH, Kim MH, Lee MK, Eom JS. Problems in the pathologic diagnosis of suspected lung cancer. Tuberc Respir Dis (Seoul). 2023; 86:176–82.
Article5. Herth FJ, Ernst A, Becker HD. Endobronchial ultrasound-guided transbronchial lung biopsy in solitary pulmonary nodules and peripheral lesions. Eur Respir J. 2002; 20:972–4.
Article6. Kurimoto N, Miyazawa T, Okimasa S, Maeda A, Oiwa H, Miyazu Y, et al. Endobronchial ultrasonography using a guide sheath increases the ability to diagnose peripheral pulmonary lesions endoscopically. Chest. 2004; 126:959–65.
Article7. Wang Memoli JS, Nietert PJ, Silvestri GA. Meta-analysis of guided bronchoscopy for the evaluation of the pulmonary nodule. Chest. 2012; 142:385–93.
Article8. Asano F, Matsuno Y, Shinagawa N, Yamazaki K, Suzuki T, Ishida T, et al. A virtual bronchoscopic navigation system for pulmonary peripheral lesions. Chest. 2006; 130:559–66.
Article9. Eberhardt R, Anantham D, Herth F, Feller-Kopman D, Ernst A. Electromagnetic navigation diagnostic bronchoscopy in peripheral lung lesions. Chest. 2007; 131:1800–5.
Article10. Oki M, Saka H. Diagnostic value of ultrathin bronchoscopy in peripheral pulmonary lesions: a narrative review. J Thorac Dis. 2020; 12:7675–82.
Article11. McInnes MD, Moher D, Thombs BD, McGrath TA, Bossuyt PM; PRISMA-DTA Group, et al. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA. 2018; 319:388–96.
Article12. Baaklini WA, Reinoso MA, Gorin AB, Sharafkaneh A, Manian P. Diagnostic yield of fiberoptic bronchoscopy in evaluating solitary pulmonary nodules. Chest. 2000; 117:1049–54.
Article13. Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011; 155:529–36.
Article14. Ali MS, Sethi J, Taneja A, Musani A, Maldonado F. Computed tomography bronchus sign and the diagnostic yield of guided bronchoscopy for peripheral pulmonary lesions: a systematic review and meta-analysis. Ann Am Thorac Soc. 2018; 15:978–87.
Article15. Kim SH, Kim J, Pak K, Eom JS. Ultrathin bronchoscopy for the diagnosis of peripheral pulmonary lesions: a meta-analysis. Respiration. 2023; 102:34–45.
Article16. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–60.
Article17. Dinnes J, Deeks J, Kirby J, Roderick P. A methodological review of how heterogeneity has been examined in systematic reviews of diagnostic test accuracy. Health Technol Assess. 2005; 9:1–113.
Article18. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010; 1:97–111.
Article19. Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol. 2014; 67:897–903.
Article20. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–34.
Article21. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994; 50:1088–101.
Article22. Oki M, Saka H, Asano F, Kitagawa C, Kogure Y, Tsuzuku A, et al. Use of an ultrathin vs thin bronchoscope for peripheral pulmonary lesions: a randomized trial. Chest. 2019; 156:954–64.
Article23. Fuso L, Varone F, Magnini D, Baldi F, Rindi G, Pagliari G, et al. Role of ultrasound-guided transbronchial biopsy in the diagnosis of peripheral pulmonary lesions. Lung Cancer. 2013; 81:60–4.
Article24. Tamiya M, Okamoto N, Sasada S, Shiroyama T, Morishita N, Suzuki H, et al. Diagnostic yield of combined bronchoscopy and endobronchial ultrasonography, under LungPoint guidance for small peripheral pulmonary lesions. Respirology. 2013; 18:834–9.
Article25. Tay JH, Irving L, Antippa P, Steinfort DP. Radial probe endobronchial ultrasound: factors influencing visualization yield of peripheral pulmonary lesions. Respirology. 2013; 18:185–90.
Article26. Chen A, Chenna P, Loiselle A, Massoni J, Mayse M, Misselhorn D. Radial probe endobronchial ultrasound for peripheral pulmonary lesions: a 5-year institutional experience. Ann Am Thorac Soc. 2014; 11:578–82.
Article27. Evison M, Crosbie PA, Morris J, Martin J, Barber PV, Booton R. Can computed tomography characteristics predict outcomes in patients undergoing radial endobronchial ultrasound-guided biopsy of peripheral lung lesions? J Thorac Oncol. 2014; 9:1393–7.
Article28. Kuo CH, Lin SM, Lee KY, Chung FT, Lo YL, Hsiung TC, et al. Endobronchial ultrasound-guided transbronchial biopsy and brushing: a comparative evaluation for the diagnosis of peripheral pulmonary lesions. Eur J Cardiothorac Surg. 2014; 45:894–8.
Article29. Sanchez-Font A, Giralt L, Vollmer I, Pijuan L, Gea J, Curull V. Endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions: a controlled study with fluoroscopy. Arch Bronconeumol. 2014; 50:166–71.
Article30. Asano F, Shinagawa N, Ishida T, Tsuzuku A, Tachihara M, Kanazawa K, et al. Virtual bronchoscopic navigation improves the diagnostic yield of radial-endobronchial ultrasound for peripheral pulmonary lesions with involved bronchi on CT. Intern Med. 2015; 54:1021–5.
Article31. Boonsarngsuk V, Kanoksil W, Laungdamerongchai S. Comparison of diagnostic performances among bronchoscopic sampling techniques in the diagnosis of peripheral pulmonary lesions. J Thorac Dis. 2015; 7:697–703.32. Chan A, Devanand A, Low SY, Koh MS. Radial endobronchial ultrasound in diagnosing peripheral lung lesions in a high tuberculosis setting. BMC Pulm Med. 2015; 15:90.
Article33. Guvenc C, Yserbyt J, Testelmans D, Zanca F, Carbonez A, Ninane V, et al. Computed tomography characteristics predictive for radial EBUS-miniprobe-guided diagnosis of pulmonary lesions. J Thorac Oncol. 2015; 10:472–8.
Article34. Minezawa T, Okamura T, Yatsuya H, Yamamoto N, Morikawa S, Yamaguchi T, et al. Bronchus sign on thin-section computed tomography is a powerful predictive factor for successful transbronchial biopsy using endobronchial ultrasound with a guide sheath for small peripheral lung lesions: a retrospective observational study. BMC Med Imaging. 2015; 15:21.
Article35. Oki M, Saka H, Ando M, Asano F, Kurimoto N, Morita K, et al. Ultrathin bronchoscopy with multimodal devices for peripheral pulmonary lesions: a randomized trial. Am J Respir Crit Care Med. 2015; 192:468–76.
Article36. Jacomelli M, Demarzo SE, Cardoso PF, Palomino AL, Figueiredo VR. Radial-probe EBUS for the diagnosis of peripheral pulmonary lesions. J Bras Pneumol. 2016; 42:248–53.
Article37. Kunimasa K, Tachihara M, Tamura D, Tokunaga S, Nakata K, Hazeki N, et al. Diagnostic utility of additional conventional techniques after endobronchial ultrasonography guidance during transbronchial biopsy. Respirology. 2016; 21:1100–5.
Article38. Steinfort DP, Bonney A, See K, Irving LB. Sequential multimodality bronchoscopic investigation of peripheral pulmonary lesions. Eur Respir J. 2016; 47:607–14.
Article39. Wang C, Li X, Zhou Z, Zhao H, Li Z, Jiang G, et al. Endobronchial ultrasonography with guide sheath versus computed tomography guided transthoracic needle biopsy for peripheral pulmonary lesions: a propensity score matched analysis. J Thorac Dis. 2016; 8:2758–64.
Article40. Asano F, Ishida T, Shinagawa N, Sukoh N, Anzai M, Kanazawa K, et al. Virtual bronchoscopic navigation without X-ray fluoroscopy to diagnose peripheral pulmonary lesions: a randomized trial. BMC Pulm Med. 2017; 17:184.
Article41. Huang CT, Ruan SY, Tsai YJ, Ho CC, Yu CJ. Experience improves the performance of endobronchial ultrasound-guided transbronchial biopsy for peripheral pulmonary lesions: a learning curve at a medical centre. PLoS One. 2017; 12:e0179719.
Article42. Eom JS, Mok JH, Kim I, Lee MK, Lee G, Park H, et al. Radial probe endobronchial ultrasound using a guide sheath for peripheral lung lesions in beginners. BMC Pulm Med. 2018; 18:137.
Article43. Good WR, Christensen PM, Herath S, Dawkins P, Yap E. Radial-probe endobronchial ultrasound outcomes in the investigation of peripheral pulmonary lesions: a New Zealand perspective. Intern Med J. 2018; 48:1481–7.
Article44. Tanner NT, Yarmus L, Chen A, Wang Memoli J, Mehta HJ, Pastis NJ, et al. Standard bronchoscopy with fluoroscopy vs thin bronchoscopy and radial endobronchial ultrasound for biopsy of pulmonary lesions: a multicenter, prospective, randomized trial. Chest. 2018; 154:1035–43.
Article45. Zhang SJ, Zhang M, Zhou J, Zhang QD, Xu QQ, Xu X. Radial endobronchial ultrasonography with distance measurement through a thin bronchoscope for the diagnosis of malignant peripheral pulmonary lesions. Transl Lung Cancer Res. 2018; 7:80–7.
Article46. Bo L, Li C, Pan L, Wang H, Li S, Li Q, et al. Diagnosing a solitary pulmonary nodule using multiple bronchoscopic guided technologies: a prospective randomized study. Lung Cancer. 2019; 129:48–54.
Article47. Kho SS, Chan SK, Yong MC, Tie ST. Performance of transbronchial cryobiopsy in eccentrically and adjacently orientated radial endobronchial ultrasound lesions. ERJ Open Res. 2019; 5:00135–2019.
Article48. Xu C, Yuan Q, Wang Y, Wang W, Chi C, Zhang Q, et al. Usefulness of virtual bronchoscopic navigation combined with endobronchial ultrasound guided transbronchial lung biopsy for solitary pulmonary nodules. Medicine (Baltimore). 2019; 98:e14248.
Article49. Zhu J, Gu Y. Diagnosis of peripheral pulmonary lesions using endobronchial ultrasonography with a guide sheath and computed tomography guided transthoracic needle aspiration. Clin Respir J. 2019; 13:765–72.
Article50. Boonsarngsuk V, Petnak T, So-Ngern A, Saksitthichok B, Kanoksil W. Comparison of different transbronchial biopsy sampling techniques for the diagnosis of peripheral pulmonary lesions with radial endobronchial ultrasound-guided bronchoscopy: a prospective study. Respir Investig. 2020; 58:381–6.
Article51. Samaranayake CB, Wright C, Erigadoo S, Azzopardi M, Putt M, Bint M. A randomized controlled trial on optimal sampling sequence in radial guide sheath endobronchial ultrasound lung biopsy. J Bronchology Interv Pulmonol. 2020; 27:205–11.
Article52. Goel MK, Kumar A, Maitra G, Singh B, Ahlawat S, Jain P, et al. Radial EBUS-guided cryobiopsy of peripheral lung lesions with flexible bronchoscopy without using guide-sheath. J Bronchology Interv Pulmonol. 2021; 28:184–91.
Article53. Hong KS, Ahn H, Lee KH, Chung JH, Shin KC, Jin HJ, et al. Radial probe endobronchial ultrasound using guide sheath-guided transbronchial lung biopsy in peripheral pulmonary lesions without fluoroscopy. Tuberc Respir Dis (Seoul). 2021; 84:282–90.
Article54. Jiang L, Xu J, Liu C, Gao N, Zhao J, Han X, et al. Diagnosis of peripheral pulmonary lesions with transbronchial lung cryobiopsy by guide sheath and radial endobronchial ultrasonography: a prospective control study. Can Respir J. 2021; 2021:6947037.
Article55. Zheng X, Xie F, Li Y, Chen J, Jiang Y, Sun J. Ultrathin bronchoscope combined with virtual bronchoscopic navigation and endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions with or without fluoroscopy: a randomized trial. Thorac Cancer. 2021; 12:1864–72.
Article56. Ito T, Matsumoto Y, Okachi S, Nishida K, Tanaka M, Imabayashi T, et al. A diagnostic predictive model of bronchoscopy with radial endobronchial ultrasound for peripheral pulmonary lesions. Respiration. 2022; 101:1148–56.
Article57. Kim SH, Mok J, Jo EJ, Kim MH, Lee K, Kim KU, et al. The additive impact of transbronchial cryobiopsy using a 1.1-mm diameter cryoprobe on conventional biopsy for peripheral lung nodules. Cancer Res Treat. 2023; 55:506–12.
Article58. Lee J, Kim C, Seol HY, Chung HS, Mok J, Lee G, et al. Safety and diagnostic yield of radial probe endobronchial ultrasound-guided biopsy for peripheral lung lesions in patients with idiopathic pulmonary fibrosis: a multicenter cross-sectional study. Respiration. 2022; 101:401–7.
Article59. Liu Y, Wang F, Zhang Q, Tong Z. Diagnostic yield of virtual bronchoscope navigation combined with radial endobronchial ultrasound guided transbronchial cryo-biopsy for peripheral pulmonary nodules: a prospective, randomized, controlled trial. Ann Transl Med. 2022; 10:443.
Article60. Oki M, Saka H, Imabayashi T, Himeji D, Nishii Y, Nakashima H, et al. Guide sheath versus non-guide sheath method for endobronchial ultrasound-guided biopsy of peripheral pulmonary lesions: a multicentre randomised trial. Eur Respir J. 2022; 59:2101678.61. Tanaka M, Matsumoto Y, Imabayashi T, Kawahara T, Tsuchida T. Diagnostic value of a new cryoprobe for peripheral pulmonary lesions: a prospective study. BMC Pulm Med. 2022; 22:226.
Article62. Zheng X, Zhong C, Xie F, Li S, Wang G, Zhang L, et al. Virtual bronchoscopic navigation and endobronchial ultrasound with a guide sheath without fluoroscopy for diagnosing peripheral pulmonary lesions with a bronchus leading to or adjacent to the lesion: a randomized non-inferiority trial. Respirology. 2023; 28:389–98.
Article63. Ali MS, Trick W, Mba BI, Mohananey D, Sethi J, Musani AI. Radial endobronchial ultrasound for the diagnosis of peripheral pulmonary lesions: a systematic review and meta-analysis. Respirology. 2017; 22:443–53.
Article64. Huang CT, Ho CC, Tsai YJ, Yu CJ, Yang PC. Factors influencing visibility and diagnostic yield of transbronchial biopsy using endobronchial ultrasound in peripheral pulmonary lesions. Respirology. 2009; 14:859–64.
Article65. Folch EE, Labarca G, Ospina-Delgado D, Kheir F, Majid A, Khandhar SJ, et al. Sensitivity and safety of electromagnetic navigation bronchoscopy for lung cancer diagnosis: systematic review and meta-analysis. Chest. 2020; 158:1753–69.
Article66. Torky M, Elshimy WS, Ragab MA, Attia GA, Lopez R, Mate JL, et al. Endobronchial ultrasound guided transbronchial cryobiopsy versus forceps biopsy in peripheral lung lesions. Clin Respir J. 2021; 15:320–8.
Article67. Ankudavicius V, Miliauskas S, Poskiene L, Vajauskas D, Zemaitis M. Diagnostic yield of transbronchial cryobiopsy guided by radial endobronchial ultrasound and fluoroscopy in the radiologically suspected lung cancer: a single institution prospective study. Cancers (Basel). 2022; 14:1563.
Article68. Nadig TR, Thomas N, Nietert PJ, Lozier J, Tanner NT, Wang Memoli JS, et al. Guided bronchoscopy for the evaluation of pulmonary lesions: an updated meta-analysis. Chest. 2023; 163:1589–98.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Updates in diagnostic bronchoscopy for lung cancer
- An update on the role of bronchoscopy in the diagnosis of pulmonary disease
- Photodynamic Therapy for Endobronchial Obstruction due to Recurrent Lung Cancer : 2 Cases Report
- Utility of Radial Probe Endobronchial Ultrasound-Guided Transbronchial Lung Biopsy in Diffuse Lung Lesions
- Technical Aspects of Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration