Infect Chemother.
2019 Sep;51(3):263-273. 10.3947/ic.2019.51.3.263.
Prognostic Value of Serum Procalcitonin level for the Diagnosis of Bacterial Infections in Critically-ill Patients
- Affiliations
-
- 1Faculty of Pharmacy, Siam University, Bangkok, Thailand.
- 2Department of Medicine, Phyathai 2 International Hospital, Bangkok, Thailand.
- 3Department of Pharmacy, Faculty of Pharmacy, Mahidol University, Bangkok, Thailand. preecha.mon@mahidol.ac.th
- 4Clinical Pharmacy Unit, Division of Pharmacy, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand.
- KMID: 2459042
- DOI: http://doi.org/10.3947/ic.2019.51.3.263
Abstract
- BACKGROUND
Procalcitonin (PCT) is a diagnostic biomarker for bacterial infections in critically-ill patients. However, the cut-off value of PCT for the diagnosis of bacterial infections is unclear and unreliable. This study aimed to determine the optimal cut-off value of PCT for the diagnosis of bacterial infections in critically-ill patients.
MATERIALS AND METHODS
We conducted a retrospective study involving 311 adult patients who had been admitted to the medical or surgical intensive care unit for more than 24 hours from 2013 to 2015. At least one blood test for PCT level was performed for all patients within the first 24 hours of suspecting an infection.
RESULTS
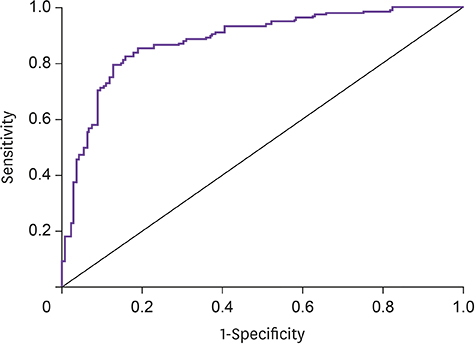
One hundred and fifty-seven patients had bacterial infections, while 154 did not. Patients with bacterial infections had a significantly higher median PCT level than those without bacterial infections (1.90 ng/mL vs. 0.16 ng/mL, P <0.001). The area under the receiver operating characteristic curve of PCT for discriminating between bacterial and non-bacterial infections was 0.874 (95% confidence interval: 0.834, 0.914; P <0.001). The optimal cut-off value of PCT for differentiating between fevers due to bacterial infections from those due to non-bacterial infections was 0.5 ng/mL, with a sensitivity of 84.7%, specificity of 79.9%, positive predictive value of 81.1%, and negative predictive value of 83.7%.
CONCLUSION
PCT was found to be an accurate biomarker for the diagnosis of bacterial infections among patients admitted to medical and surgical intensive care units. The optimal cut-off value of PCT for the diagnosis of bacterial infections was 0.5 ng/mL.
MeSH Terms
Figure
Cited by 1 articles
-
An Update on Sepsis Biomarkers
Mi-Hee Kim, Jung-Hyun Choi
Infect Chemother. 2020;52(1):1-18. doi: 10.3947/ic.2020.52.1.1.
Reference
-
1. Barati M, Alinejad F, Bahar MA, Tabrisi MS, Shamshiri AR, Bodouhi NO, Karimi H. Comparison of WBC, ESR, CRP and PCT serum levels in septic and non-septic burn cases. Burns. 2008; 34:770–774.
Article2. Laupland KB. Fever in the critically ill medical patient. Crit Care Med. 2009; 37:Suppl 7. S273–S278.
Article3. Levin PD, Idrees S, Sprung CL, Weissman C, Weiss Y, Moses AE, Benenson S. Antimicrobial use in the ICU: indications and accuracy--an observational trial. J Hosp Med. 2012; 7:672–678.
Article4. Huttner A, Harbarth S, Carlet J, Cosgrove S, Goossens H, Holmes A, Jarlier V, Voss A, Pittet D. Antimicrobial resistance: a global view from the 2013 World Healthcare-Associated Infections Forum. Antimicrob Resist Infect Control. 2013; 2:31.
Article5. Pittet D, Rangel-Frausto S, Li N, Tarara D, Costigan M, Rempe L, Jebson P, Wenzel RP. Systemic inflammatory response syndrome, sepsis, severe sepsis and septic shock: incidence, morbidities and outcomes in surgical ICU patients. Intensive Care Med. 1995; 21:302–309.
Article6. Schuetz P, Albrich W, Mueller B. Procalcitonin for diagnosis of infection and guide to antibiotic decisions: past, present and future. BMC Med. 2011; 9:107.
Article7. Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, Bohuon C. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994; 79:1605–1608.
Article8. Castelli GP, Pognani C, Meisner M, Stuani A, Bellomi D, Sgarbi L. Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. Crit Care. 2004; 8:R234–R242.9. Harbarth S, Holeckova K, Froidevaux C, Pittet D, Ricou B, Grau GE, Vadas L, Pugin J. Diagnostic value of procalcitonin, interleukin-6, and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med. 2001; 164:396–402.
Article10. BalcI C, Sungurtekin H, Gürses E, Sungurtekin U, Kaptanoglu B. Usefulness of procalcitonin for diagnosis of sepsis in the intensive care unit. Crit Care. 2003; 7:85–90.11. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, Osborn TM, Nunnally ME, Townsend SR, Reinhart K, Kleinpell RM, Angus DC, Deutschman CS, Machado FR, Rubenfeld GD, Webb SA, Beale RJ, Vincent JL, Moreno R. Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013; 41:580–637.
Article12. Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013; 13:426–435.
Article13. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:801–810.
Article14. Kalil AC, Metersky ML, Klompas M, Muscedere J, Sweeney DA, Palmer LB, Napolitano LM, O'Grady NP, Bartlett JG, Carratalà J, El Solh AA, Ewig S, Fey PD, File TM Jr, Restrepo MI, Roberts JA, Waterer GW, Cruse P, Knight SL, Brozek JL. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016; 63:e61–e111.15. Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, Srinivasan A, Dellit TH, Falck-Ytter YT, Fishman NO, Hamilton CW, Jenkins TC, Lipsett PA, Malani PN, May LS, Moran GJ, Neuhauser MM, Newland JG, Ohl CA, Samore MH, Seo SK, Trivedi KK. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016; 62:e51–e77.
Article16. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008; 36:309–332.
Article17. Brodská H, Malíčková K, Adámková V, Benáková H, Šťastná MM, Zima T. Significantly higher procalcitonin levels could differentiate Gram-negative sepsis from Gram-positive and fungal sepsis. Clin Exp Med. 2013; 13:165–170.
Article18. Becker KL, Snider R, Nylen ES. Procalcitonin assay in systemic inflammation, infection, and sepsis: clinical utility and limitations. Crit Care Med. 2008; 36:941–952.
Article19. Schneider HG, Lam QT. Procalcitonin for the clinical laboratory: a review. Pathology. 2007; 39:383–390.
Article20. Hunziker S, Hügle T, Schuchardt K, Groeschl I, Schuetz P, Mueller B, Dick W, Eriksson U, Trampuz A. The value of serum procalcitonin level for differentiation of infectious from noninfectious causes of fever after orthopaedic surgery. J Bone Joint Surg Am. 2010; 92:138–148.
Article21. Tamaki K, Kogata Y, Sugiyama D, Nakazawa T, Hatachi S, Kageyama G, Nishimura K, Morinobu A, Kumagai S. Diagnostic accuracy of serum procalcitonin concentrations for detecting systemic bacterial infection in patients with systemic autoimmune diseases. J Rheumatol. 2008; 35:114–119.22. Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. 2003; 348:138–150.
Article23. Clec'h C, Fosse JP, Karoubi P, Vincent F, Chouahi I, Hamza L, Cupa M, Cohen Y. Differential diagnostic value of procalcitonin in surgical and medical patients with septic shock. Crit Care Med. 2006; 34:102–107.24. Meisner M, Tschaikowsky K, Hutzler A, Schick C, Schüttler J. Postoperative plasma concentrations of procalcitonin after different types of surgery. Intensive Care Med. 1998; 24:680–684.
Article25. Picariello C, Lazzeri C, Chiostri M, Gensini GF, Valente S. Kinetic of procalcitonin in patients with cardiogenic shock following acute myocardial infarction: preliminary data. HSR Proc Intensive Care Cardiovasc Anesth. 2010; 2:201–207.26. Level C, Chauveau P, Delmas Y, Lasseur C, Pellé G, Peuchant E, Montaudon D, Combe C. Procalcitonin: a new marker of inflammation in haemodialysis patients? Nephrol Dial Transplant. 2001; 16:980–986.
Article27. Franke A, Lante W, Fackeldey V, Becker HP, Kurig E, Zöller LG, Weinhold C, Markewitz A. Pro-inflammatory cytokines after different kinds of cardio-thoracic surgical procedures: is what we see what we know? Eur J Cardiothorac Surg. 2005; 28:569–575.
Article28. Andersen LW, Landow L, Baek L, Jansen E, Baker S. Association between gastric intramucosal pH and splanchnic endotoxin, antibody to endotoxin, and tumor necrosis factor-alpha concentrations in patients undergoing cardiopulmonary bypass. Crit Care Med. 1993; 21:210–217.
Article29. Buttenschoen K, Buttenschoen DC, Berger D, Vasilescu C, Schafheutle S, Goeltenboth B, Seidelmann M, Beger HG. Endotoxemia and acute-phase proteins in major abdominal surgery. Am J Surg. 2001; 181:36–43.
Article30. Laifer G, Wasner M, Sendi P, Graber P, Gratzl O, Huber P, Fluckiger U, Zimmerli W. Dynamics of serum procalcitonin in patients after major neurosurgery. Clin Microbiol Infect. 2005; 11:679–681.
Article31. Osuka K, Suzuki Y, Saito K, Takayasu M, Shibuya M. Changes in serum cytokine concentrations after neurosurgical procedures. Acta Neurochir (Wien). 1996; 138:970–976.
Article32. Bouaicha S, Blatter S, Moor BK, Spanaus K, Dora C, Werner CM. Early serum procalcitonin level after primary total hip replacement. Mediators Inflamm. 2013; 2013:927636.
Article33. Eder J, Hlavin G, Haushofer A, Trubert-Exinger D, Trautinger F. Correlation of serum procalcitonin with the severity of skin and skin structure infections - a pilot study. J Dtsch Dermatol Ges. 2012; 10:564–571.
Article34. Daniels JM, Schoorl M, Snijders D, Knol DL, Lutter R, Jansen HM, Boersma WG. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010; 138:1108–1115.
Article35. Pecile P, Miorin E, Romanello C, Falleti E, Valent F, Giacomuzzi F, Tenore A. Procalcitonin: a marker of severity of acute pyelonephritis among children. Pediatrics. 2004; 114:e249–e254.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Usefulness of Semi-quantitative Procalcitonin Assay in Critically Ill Patients with Bacterial Pneumonia
- Semi-quantitative Procalcitonin Assay in Critically ill Patients with Respiratory infections
- Procalcitonin as a Diagnostic and Prognostic Factor for Tuberculosis Meningitis
- Serum Procalcitonin Level Reflects the Severity of Cellulitis
- Serum Procalcitonin for Differentiating Bacterial Infection from Disease Flares in Patients with Autoimmune Diseases