J Clin Neurol.
2016 Jul;12(3):332-339. 10.3988/jcn.2016.12.3.332.
Procalcitonin as a Diagnostic and Prognostic Factor for Tuberculosis Meningitis
- Affiliations
-
- 1Department of Family Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 2Department of Neurology, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. smilepkm@hanmail.net
- 3Department of Internal Medicine, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2354121
- DOI: http://doi.org/10.3988/jcn.2016.12.3.332
Abstract
- BACKGROUND AND PURPOSE
We investigated the potential role of serum procalcitonin in differentiating tuberculosis meningitis from bacterial and viral meningitis, and in predicting the prognosis of tuberculosis meningitis.
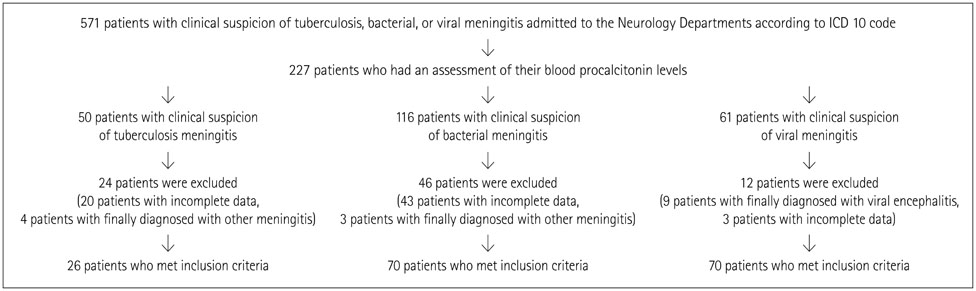
METHODS
This was a retrospective study of 26 patients with tuberculosis meningitis. In addition, 70 patients with bacterial meningitis and 49 patients with viral meningitis were included as the disease control groups for comparison. The serum procalcitonin level was measured in all patients at admission. Differences in demographic and laboratory data, including the procalcitonin level, were analyzed among the three groups. In addition, we analyzed the predictive factors for a prognosis of tuberculosis meningitis using the Glasgow Coma Scale (GCS) at discharge, and the correlation between the level of procalcitonin and the GCS score at discharge.
RESULTS
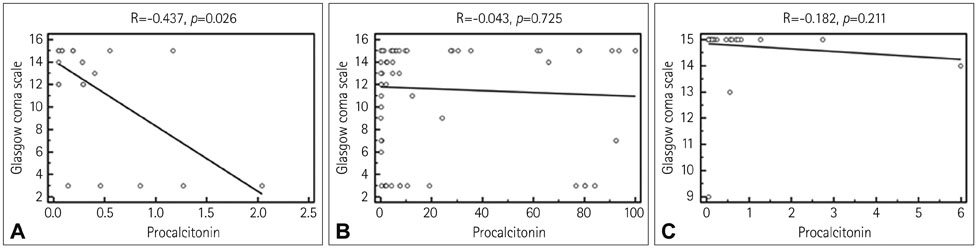
Multiple logistic regression analysis showed that a low level of procalcitonin (≤1.27 ng/mL) independently distinguished tuberculosis meningitis from bacterial meningitis. The sensitivity and specificity for distinguishing tuberculosis meningitis from bacterial meningitis were 96.2% and 62.9%, respectively. However, the level of procalcitonin in patients with tuberculosis meningitis did not differ significantly from that in patients with viral meningitis. In patients with tuberculosis meningitis, a high level of procalcitonin (>0.4 ng/mL) was a predictor of a poor prognosis, and the level of procalcitonin was negatively correlated with the GCS score at discharge (r=-0.437, p=0.026).
CONCLUSIONS
We found that serum procalcitonin is a useful marker for differentiating tuberculosis meningitis from bacterial meningitis and is also valuable for predicting the prognosis of tuberculosis meningitis.
Keyword
MeSH Terms
Figure
Reference
-
1. Garg RK. Tuberculous meningitis. Acta Neurol Scand. 2010; 122:75–90.
Article2. Yoon YK, Jo YM, Kwon HH, Yoon HJ, Lee EJ, Park SY, et al. Differential diagnosis between tuberculous spondylodiscitis and pyogenic spontaneous spondylodiscitis: a multicenter descriptive and comparative study. Spine J. 2015; 15:1764–1771.
Article3. Erdem H, Ozturk-Engin D, Tireli H, Kilicoglu G, Defres S, Gulsun S, et al. Hamsi scoring in the prediction of unfavorable outcomes from tuberculous meningitis: results of Haydarpasa-II study. J Neurol. 2015; 262:890–898.
Article4. Joosten AA, van der Valk PD, Geelen JA, Severin WP, Jansen Steur EN. Tuberculous meningitis: pitfalls in diagnosis. Acta Neurol Scand. 2000; 102:388–394.
Article5. Prat C, Domínguez J, Andreo F, Blanco S, Pallarés A, Cuchillo F, et al. Procalcitonin and neopterin correlation with aetiology and severity of pneumonia. J Infect. 2006; 52:169–177.
Article6. Huang CT, Lee LN, Ho CC, Shu CC, Ruan SY, Tsai YJ, et al. High serum levels of procalcitonin and soluble TREM-1 correlated with poor prognosis in pulmonary tuberculosis. J Infect. 2014; 68:440–447.
Article7. Huang SL, Lee HC, Yu CW, Chen HC, Wang CC, Wu JY, et al. Value of procalcitonin in differentiating pulmonary tuberculosis from other pulmonary infections: a meta-analysis. Int J Tuberc Lung Dis. 2014; 18:470–477.
Article8. Viallon A, Zeni F, Lambert C, Pozzetto B, Tardy B, Venet C, et al. High sensitivity and specificity of serum procalcitonin levels in adults with bacterial meningitis. Clin Infect Dis. 1999; 28:1313–1316.
Article9. Dubos F, Moulin F, Gajdos V, De Suremain N, Biscardi S, Lebon P, et al. Serum procalcitonin and other biologic markers to distinguish between bacterial and aseptic meningitis. J Pediatr. 2006; 149:72–76.
Article10. Kang YA, Kwon SY, Yoon HI, Lee JH, Lee CT. Role of C-reactive protein and procalcitonin in differentiation of tuberculosis from bacterial community acquired pneumonia. Korean J Intern Med. 2009; 24:337–342.
Article11. Niu WY, Wan YG, Li MY, Wu ZX, Zhang LG, Wang JX. The diagnostic value of serum procalcitonin, IL-10 and C-reactive protein in community acquired pneumonia and tuberculosis. Eur Rev Med Pharmacol Sci. 2013; 17:3329–3333.12. Nyamande K, Lalloo UG. Serum procalcitonin distinguishes CAP due to bacteria, Mycobacterium tuberculosis and PJP. Int J Tuberc Lung Dis. 2006; 10:510–515.13. Cakir E, Deniz O, Ozcan O, Tozkoparan E, Yaman H, Akgul EO, et al. Pleural fluid and serum procalcitonin as diagnostic tools in tuberculous pleurisy. Clin Biochem. 2005; 38:234–238.
Article14. Marais S, Thwaites G, Schoeman JF, Török ME, Misra UK, Prasad K, et al. Tuberculous meningitis: a uniform case definition for use in clinical research. Lancet Infect Dis. 2010; 10:803–812.
Article15. Ropper AH, Samuels MA, Klein J. Adams and Victor's Principles of Neurology. 10th ed. Columbus: McGraw-Hill Education;2014. p. 697–777.16. Thwaites GE, Chau TT, Stepniewska K, Phu NH, Chuong LV, Sinh DX, et al. Diagnosis of adult tuberculous meningitis by use of clinical and laboratory features. Lancet. 2002; 360:1287–1292.
Article17. Assicot M, Gendrel D, Carsin H, Raymond J, Guilbaud J, Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993; 341:515–518.
Article18. Linscheid P, Seboek D, Schaer DJ, Zulewski H, Keller U, Müller B. Expression and secretion of procalcitonin and calcitonin gene-related peptide by adherent monocytes and by macrophage-activated adipocytes. Crit Care Med. 2004; 32:1715–1721.
Article19. Maruna P, Nedelníková K, Gürlich R. Physiology and genetics of procalcitonin. Physiol Res. 2000; 49:Suppl 1. S57–S61.20. van Rossum AM, Wulkan RW, Oudesluys-Murphy AM. Procalcitonin as an early marker of infection in neonates and children. Lancet Infect Dis. 2004; 4:620–630.
Article21. Dandona P, Nix D, Wilson MF, Aljada A, Love J, Assicot M, et al. Procalcitonin increase after endotoxin injection in normal subjects. J Clin Endocrinol Metab. 1994; 79:1605–1608.
Article22. Alarcón F, Moreira J, Rivera J, Salinas R, Dueñas G, Van den Ende J. Tuberculous meningitis: do modern diagnostic tools offer better prognosis prediction? Indian J Tuberc. 2013; 60:5–14.23. Hosoglu S, Geyik MF, Balik I, Aygen B, Erol S, Aygencel TG, et al. Predictors of outcome in patients with tuberculous meningitis. Int J Tuberc Lung Dis. 2002; 6:64–70.24. Hosoğlu S, Ayaz C, Geyik MF, Kökoğlu OF, Ceviz A. Tuberculous meningitis in adults: an eleven-year review. Int J Tuberc Lung Dis. 1998; 2:553–557.25. Ruokonen E, Ilkka L, Niskanen M, Takala J. Procalcitonin and neopterin as indicators of infection in critically ill patients. Acta Anaesthesiol Scand. 2002; 46:398–404.
Article26. Rasmussen TA, Søgaard OS, Camara C, Andersen PL, Wejse C. Serum procalcitonin in pulmonary tuberculosis. Int J Tuberc Lung Dis. 2011; 15:251–256.27. Hu R, Gong Y, Wang Y. Relationship of serum procalcitonin levels to severity and prognosis in pediatric bacterial meningitis. Clin Pediatr (Phila). 2015; 54:1141–1144.
Article28. Chiang SS, Khan FA, Milstein MB, Tolman AW, Benedetti A, Starke JR, et al. Treatment outcomes of childhood tuberculous meningitis: a systematic review and meta-analysis. Lancet Infect Dis. 2014; 14:947–957.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the Amplicor(TM) M. tuberculosis PCR test for the Diagnosis of M. tuberculosis meningitis
- Study on the Demonstration of Enteroviruses from Cerebrospinal Fluid of Adult Patients with Aseptic Meningitis
- Applying the Bacterial Meningitis Score in Neonates Diagnosed Meningitis: A Single Center Experience
- Studies on LDH activity in cerebrospinal fluid of tuberculosis, purulent and aseptic meningitis in children
- Brain CT and clinical finding in tuberlous meningitis