J Pathol Transl Med.
2019 Jul;53(4):236-243. 10.4132/jptm.2019.03.21.
Serous Adenocarcinoma of Fallopian Tubes: Histological and Immunohistochemical Aspects
- Affiliations
-
- 1Department of Pathology, Sumy State University, Sumy, Ukraine. n.gyryavenko@med.sumdu.edu.ua
- 2Sumy Regional Clinical Perinatal Center, Sumy, Ukraine.
- 3Sumy State University, Sumy, Ukraine.
- KMID: 2454603
- DOI: http://doi.org/10.4132/jptm.2019.03.21
Abstract
- BACKGROUND
Although primary cancer of the fallopian tubes is a relatively rare type of tumor in female reproductive organs, its mortality is quite high. It is important to identify molecular and biological markers of this malignancy that determine its specific phenotype.
METHODS
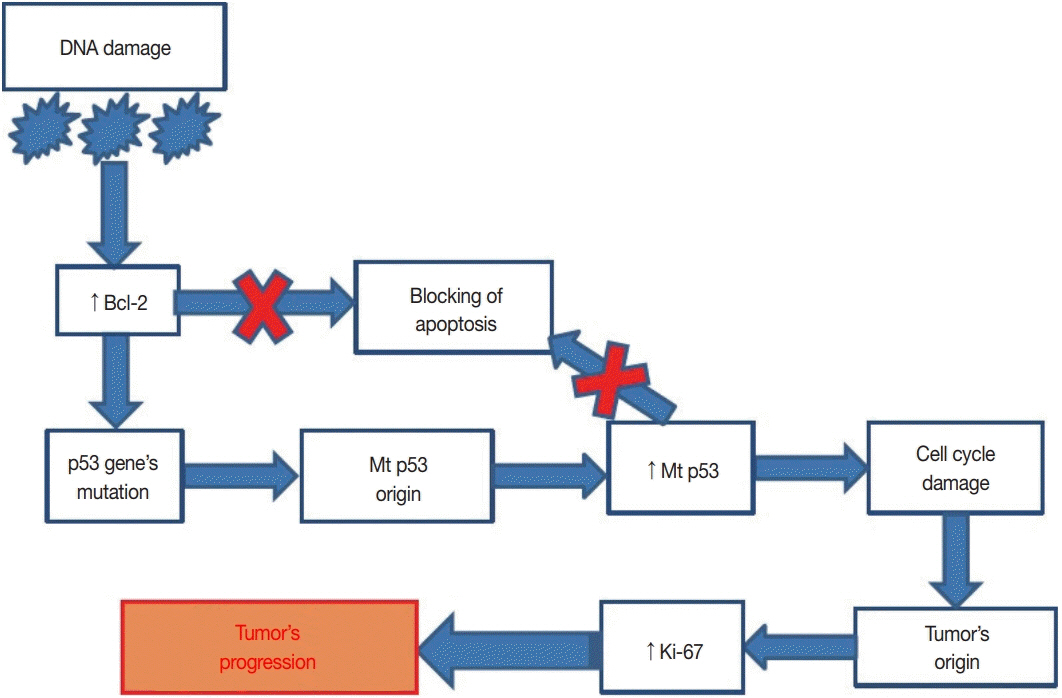
The study was carried out on samples received from 71 female patients with primary cancer of the fallopian tubes. The main molecular and biological properties, including hormone status (estrogen receptor [ER], progesterone receptor [PR]), human epidermal growth factor receptor (HER2)/neu expression, proliferative potential (Ki-67), apoptosis (p53, Bcl-2), and pro-angiogenic (vascular endothelial growth factor) quality of serous tumors were studied in comparison with clinical and morphological characteristics.
RESULTS
ER and PR expression is accompanied by low grade neoplasia, early clinical disease stage, and absence of lymphogenic metastasis (p < .001). HER2/neu expression is not typical for primary cancer of the fallopian tubes. Ki-67 expression is characterized by an inverse correlation with ER and PR (p < .05) and is associated with lymphogenic metastasis (p < .01). p53+ status correlates with high grade malignancy, tumor progression, metastasis, negative ER/PR (p < .001), and negative Bcl-2 status (p < .05). Positive Bcl-2 status is positively correlated with ER and PR expression and low grade malignancy.
CONCLUSIONS
Complex morphologic (histological and immunohistochemical) study of postoperative material allows estimation of the degree of malignancy and tumor spread to enable appropriate treatment for each case.
Keyword
MeSH Terms
Figure
Reference
-
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90.
Article2. Azodi M, Langer A, Jenison EL. Primary fallopian tube carcinoma with isolated torsion of involved tube. Eur J Gynaecol Oncol. 2000; 21:364–7.3. Singhal P, Odunsi K, Rodabaugh K, Driscoll D, Lele S. Primary fallopian tube carcinoma: a retrospective clinicopathologic study. Eur J Gynaecol Oncol. 2006; 27:16–8.4. Kalampokas E, Sofoudis C, Boutas I, Kalampokas T, Tourountous I. Primary fallopian tube carcinoma: a case report and mini-review of the literature. Eur J Gynaecol Oncol. 2014; 35:595–6.5. Riska A, Leminen A. Updating on primary fallopian tube carcinoma. Acta Obstet Gynecol Scand. 2007; 86:1419–26.
Article6. Callahan MJ, Crum CP, Medeiros F, et al. Primary fallopian tube malignancies in BRCA-positive women undergoing surgery for ovarian cancer risk reduction. J Clin Oncol. 2007; 25:3985–90.
Article7. Kalampokas E, Kalampokas T, Tourountous I. Primary fallopian tube carcinoma. Eur J Obstet Gynecol Reprod Biol. 2013; 169:155–61.
Article8. Kessler M, Fotopoulou C, Meyer T. The molecular fingerprint of high grade serous ovarian cancer reflects its fallopian tube origin. Int J Mol Sci. 2013; 14:6571–96.
Article9. Reade CJ, McVey RM, Tone AA, et al. The fallopian tube as the origin of high grade serous ovarian cancer: review of a paradigm shift. J Obstet Gynaecol Can. 2014; 36:133–40.
Article10. Kim J, Coffey DM, Creighton CJ, Yu Z, Hawkins SM, Matzuk MM. High-grade serous ovarian cancer arises from fallopian tube in a mouse model. Proc Natl Acad Sci U S A. 2012; 109:3921–6.
Article11. Przybycin CG, Kurman RJ, Ronnett BM, Shih IM, Vang R. Are all pelvic (nonuterine) serous carcinomas of tubal origin? Am J Surg Pathol. 2010; 34:1407–16.
Article12. Riska A, Leminen A, Pukkala E. Sociodemographic determinants of incidence of primary fallopian tube carcinoma, Finland 1953-97. Int J Cancer. 2003; 104:643–5.
Article13. Potapov S, Sidorenko R, Galata D, Stratiy N, Gargin V. Peculiarities of catenin activity in the embryonal testicular carcinoma. Georgian Med News. 2016; (261):68–73.14. Romaniuk A, Lyndin M, Smiyanov V, Sikora V, Rieznik A, Kuzenko Y, et al. Primary multiple tumor with affection of the thyroid gland, uterus, urinary bladder, mammary gland and other organs. Pathol Res Pract. 2017; 213:574–9.
Article15. Oliveira C, Duarte H, Bartosch C, Fernandes D. Small fallopian tube carcinoma with extensive upper abdominal dissemination: a case report. J Med Case Rep. 2013; 7:252.
Article16. Pectasides D, Pectasides E, Papaxoinis G, et al. Primary fallopian tube carcinoma: results of a retrospective analysis of 64 patients. Gynecol Oncol. 2009; 115:97–101.
Article17. Wang Y, Li L, Wang Y, Tang SN, Zheng W. Fallopian tube secretory cell expansion: a sensitive biomarker for ovarian serous carcinogenesis. Am J Transl Res. 2015; 7:2082–90.18. Wang Y, Wang Y, Li D, et al. IMP3 signatures of fallopian tube: a risk for pelvic serous cancers. J Hematol Oncol. 2014; 7:49.
Article19. Farooq S, Tasleem R, Nazir N, Reshi R, Hassan Z. Histopathological pattern of ovarian neoplasms and estrogen and progesterone receptor expression in primary epithelial tumours and their histopathological correlation. Int J Curr Res Rev. 2013; 5:70–7.20. Rose PG, Piver MS, Tsukada Y. Fallopian tube cancer. The Roswell Park experience. Cancer. 1990; 66:2661–7.
Article21. Rosen AC, Reiner A, Klein M, et al. Prognostic factors in primary fallopian tube carcinoma. Austrian Cooperative Study Group for Fallopian Tube Carcinoma. Gynecol Oncol. 1994; 53:307–13.22. Thomas C, Gustafsson JÅ. The different roles of ER subtypes in cancer biology and therapy. Nat Rev Cancer. 2011; 11:597–608.
Article23. Lacy MQ, Hartmann LC, Keeney GL, et al. c-erbB-2 and p53 expression in fallopian tube carcinoma. Cancer. 1995; 75:2891–6.
Article24. Alvarado-Cabrero I, Kiyokawa T, Piña P, Valencia-Cedillo R, Santiago-Payán H, Stolnicu S. HER2/neu, p53, MIB1 and PAX8 immunoexpression in primary serous fallopian tube carcinomas. Rev Esp Patol. 2016; 49:219–25.
Article25. Chung TK, Cheung TH, To KF, Wong YF. Overexpression of p53 and HER-2/neu and c-myc in primary fallopian tube carcinoma. Gynecol Obstet Invest. 2000; 49:47–51.26. Dawson SJ, Makretsov N, Blows FM, et al. BCL2 in breast cancer: a favourable prognostic marker across molecular subtypes and independent of adjuvant therapy received. Br J Cancer. 2010; 103:668–75.
Article27. Romaniuk A, Lyndin M. Immune microenvironment as a factor of breast cancer progression. Diagn Pathol. 2015; 10:79.
Article28. Carmeliet P. VEGF as a key mediator of angiogenesis in cancer. Oncology. 2005; 69 Suppl 3:4–10.
Article29. Lichtenberger BM, Tan PK, Niederleithner H, Ferrara N, Petzelbauer P, Sibilia M. Autocrine VEGF signaling synergizes with EGFR in tumor cells to promote epithelial cancer development. Cell. 2010; 140:268–79.
Article30. Lytvynenko M, Bocharova T, Zhelezniakova N, Narbutova T, Gargin V. Cervical transformation in alcohol abuse patients. Georgian Med News. 2017; (271):12–7.31. Lytvynenko M, Shkolnikov V, Bocharova T, Sychova L, Gargin V. Peculiarities of proliferative activity of cervical squamous cancer in HIV infection. Georgian Med News. 2017; (270):10–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Malignant Tumor of the Fallopian Tube: 2 cases Reports Papillary Carcinoma and Choriocarcionma
- Serous borderline tumor of the fallopian tube
- A Case of Adenocarcinoma in Situ of the Fallopian Tube
- Synchronous Papillary Tumor of the Fallopian Tube and Endometrium: A Case Report
- Synchronous Adenocarcinoma of Vermiform Appendix and Fallopian Tube: A case report