Nutr Res Pract.
2019 Jun;13(3):222-229. 10.4162/nrp.2019.13.3.222.
Impact of socio-demographic factors, lifestyle and health status on nutritional status among the elderly in Taiwan
- Affiliations
-
- 1School of Nutrition and Health Sciences, College of Nutrition, Taipei Medical University, 250 Wu-Hsing Street, Taipei 110, Taiwan. chenjui@tmu.edu.tw
- 2Ministry of Health, Avenue of Burkina, Ouagadougou 7035, Burkina Faso.
- 3Department of Information Management, National Taipei University of Nursing and Health Sciences, 365 Ming-Te Road, Peitou District, Taipei 112, Taiwan.
- 4Master Program in Global Health and Development, Taipei Medical University, 250 Wu-Hsing Street, Taipei 110, Taiwan.
- 5Joint Commission of Taiwan, 5F, No. 31, Sec. 2, Sanmin Rd., Banqiao Dist., New Taipei City 220, Taiwan.
- 6Nutrition Research Center, Taipei Medical University Hospital, 252 Wu-Hsing Street, Taipei 110, Taiwan.
- KMID: 2453286
- DOI: http://doi.org/10.4162/nrp.2019.13.3.222
Abstract
- BACKGROUND/OBJECTIVES
Aging is an imperative problem for many countries in this century, and presents several challenges for the maintenance of good nutritional status. This study aims to assess the impact of socio-demographic factors, lifestyle and health status on the nutritional status among the elderly in Taiwan.
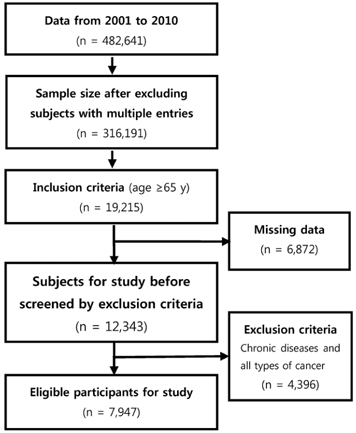
SUBJECTS/METHODS
A cross-sectional study was carried out in Taiwan. Data were obtained from the Mei Jau Health Management Institution, which is a private health evaluation provider with multiple health screening centers in Taiwan and Asia. This study included 7947 adults aged 65 years or above. The data were extracted between 2001 to 2010. Nutritional status was assessed using anthropometric data, biochemical data and dietary intake information.
RESULTS
Among the 7947 participants with mean age of 70.1 (SD = 4.5) years, 20.2%, 6.6%, 10.5% and 52.5% experienced underweight, protein malnutrition, anemia and inadequate dietary intake in the past month, respectively. Age was negatively correlated with body weight (r = −0.19, P = 0.02), body mass index (r = −0.41, P < 0.001), albumin level (r = −0.93, P < 0.001) and hemoglobin level (r = −0.30, P = 0.008). Age above 70 years, gender, unmarried status, retirement, lack of education, low family income, smoking, alcohol drinking, sleep duration of 6-8 hours, vegetarian diet, multiple medications, comorbidity and dysphagia were positively associated with malnutrition in older adults.
CONCLUSIONS
Underweight and inadequate dietary intake are prevalent among the elderly in Taiwan. Vegetarian diet, multiple medications, comorbidity, dysphagia and lifestyle factors such as smoking, alcohol drinking and sleep duration of 6-8 hours are risk factors for undernutrition in older adults.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization. Health statistics and information systems [Internet]. Geneva: World Health Organization;2016. cited 2016 August 19. Available from: http://www.who.int/healthinfo/survey/ageingdefnolder/en/.2. World Health Organization. National Institutes of Health (US). National Institute on Aging (US). Global health and aging [Internet]. Geneva: World Health Organization;2011. cited 2016 August 19. Available from: http://www.who.int/ageing/publications/global_health.pdf.3. Chen LK, Inoue H, Won CW, Lin CH, Lin KF, Tsay SF, Lin PF, Li SH. Challenges of urban aging in Taiwan: summary of urban aging forum. J Clin Gerontol Geriatr. 2013; 4:97–101.
Article4. Lu L. Aging and quality of life in Taiwan. J Altern Med Res. 2012; 4:233–243.5. National Statistics (TW). Yearly statistics: population and housing [Internet]. Taipei: National Statistics;2016. cited 2016 August 19. Available from: http://eng.stat.gov.tw/lp.asp?ctNode=2265&CtUnit=1072&BaseDSD=36&mp=5.6. Lin YY, Huang CS. Aging in Taiwan: building a society for active aging and aging in place. Gerontologist. 2016; 56:176–183.
Article7. Ahmed T, Haboubi N. Assessment and management of nutrition in older people and its importance to health. Clin Interv Aging. 2010; 5:207–216.8. Chang CC, Roberts BL. Malnutrition and feeding difficulty in Taiwanese older with dementia. J Clin Nurs. 2011; 20:2153–2161.
Article9. Madeira T, Peixoto-Plácido C, Goulão B, Mendonça N, Alarcão V, Santos N, de Oliveira RM, Yngve A, Bye A, Bergland A, Lopes C, Nicola P, Santos O, Clara JG. National survey of the Portuguese elderly nutritional status: study protocol. BMC Geriatr. 2016; 16:139.
Article10. Mathew AC, Das D, Sampath S, Vijayakumar M, Ramakrishnan N, Ravishankar SL. Prevalence and correlates of malnutrition among elderly in an urban area in Coimbatore. Indian J Public Health. 2016; 60:112–117.
Article11. Okabe Y, Furuta M, Akifusa S, Takeuchi K, Adachi M, Kinoshita T, Kikutani T, Nakamura S, Yamashita Y. Swallowing function and nutritional status in Japanese elderly people receiving home-care services: a 1-year longitudinal study. J Nutr Health Aging. 2016; 20:697–704.
Article12. Agarwalla R, Saikia AM, Baruah R. Assessment of the nutritional status of the elderly and its correlates. J Family Community Med. 2015; 22:39–43.
Article13. Porter Starr KN, McDonald SR, Bales CW. Nutritional vulnerability in older adults: a continuum of concerns. Curr Nutr Rep. 2015; 4:176–184.
Article14. Da Silva Coqueiro R, Rodrigues Barbosa A, Ferreti Borgatto A. Nutritional status, health conditions and socio-demographic factors in the elderly of Havana, Cuba: data from SABE survey. J Nutr Health Aging. 2010; 14:803–808.
Article15. Fares D, Barbosa AR, Borgatto AF, Coqueiro RS, Fernandes MH. Factors associated with nutritional status of the elderly in two regions of Brazil. Rev Assoc Med Bras (1992). 2012; 58:434–441.
Article16. Boscatto EC, da Silva Duarte MF, da Silva Coqueiro R, Barbosa AR. Nutritional status in the oldest elderly and associated factors. . Rev Assoc Med Bras (1992). 2013; 59:40–47.
Article17. United Nations Development Programme. World leaders adopt sustainable development goals [Internet]. New York, NY: United Nations Development Programme;2016. cited 2016 August 22. Available from: http://www.undp.org/content/undp/en/home/presscenter/pressreleases/2015/09/24/undp-welcomes-adoption-of-sustainable-development-goals-by-world-leaders.html.18. Lou MF, Dai YT, Huang GS, Yu PJ. Nutritional status and health outcomes for older people with dementia living in institutions. J Adv Nurs. 2007; 60:470–477.
Article19. Chen SH, Acton G, Shao JH. Relationships among nutritional self-efficacy, health locus of control and nutritional status in older Taiwanese adults. J Clin Nurs. 2010; 19:2117–2127.
Article20. Liu HY, Tseng MY, Li HJ, Wu CC, Cheng HS, Yang CT, Chou SW, Chen CY, Shyu YI. Comprehensive care improves physical recovery of hip-fractured elderly Taiwanese patients with poor nutritional status. J Am Med Dir Assoc. 2014; 15:416–422.
Article21. Chen SH, Cheng HY, Chuang YH, Shao JH. Nutritional status and its health-related factors among older adults in rural and urban areas. J Adv Nurs. 2015; 71:42–53.
Article22. Tsai MT, Liu HC, Huang TP. The impact of malnutritional status on survival in elderly hemodialysis patients. J Chin Med Assoc. 2016; 79:309–313.
Article23. Chien MH, Guo HR. Nutritional status and falls in community-dwelling older people: a longitudinal study of a population-based random sample. PLoS One. 2014; 9:e91044.
Article24. Lin CL, Lin CP, Chen SW, Wu HC, Tsai YH. The association between sleep duration and overweight or obesity in Taiwanese adults: a cross-sectional study. Obes Res Clin Pract. 2018; 12:384–388.
Article25. Chang CC. Prevalence and factors associated with feeding difficulty in institutionalized elderly with dementia in Taiwan. J Nutr Health Aging. 2012; 16:258–261.
Article26. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.27. World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity [Internet]. Geneva: World Health Organization;2011. cited 2016 August 19. Available from: http://www.who.int/vmnis/indicators/haemoglobin.pdf.28. Hengeveld LM, Wijnhoven HA, Olthof MR, Brouwer IA, Harris TB, Kritchevsky SB, Newman AB, Visser M. Health ABC Study. Prospective associations of poor diet quality with long-term incidence of protein-energy malnutrition in community-dwelling older adults: the Health, Aging, and Body Composition (Health ABC) Study. Am J Clin Nutr. 2018; 107:155–164.
Article29. Procter-Gray E, Olendzki B, Kane K, Churchill L, Hayes RB, Aguirre A, Kang HJ, Li W. Comparison of dietary quality assessment using food frequency questionnaire and 24-hour-recalls in older men and women. AIMS Public Health. 2017; 4:326–346.
Article30. Tomey KM, Chen DM, Wang X, Braunschweig CL. Dietary intake and nutritional status of urban community-dwelling men with paraplegia. Arch Phys Med Rehabil. 2005; 86:664–671.
Article31. Tessfamichael D, Gete AA, Wassie MM. High prevalence of undernutrition among elderly people in Northwest Ethiopia: a cross sectional study. J Nutr Health Food Sci. 2014; 2:1–5.
Article32. Röhrig G, Becker I, Polidori MC, Schulz RJ, Noreik M. Association of anemia and hypoalbuminemia in German geriatric inpatients: relationship to nutritional status and comprehensive geriatric assessment. Z Gerontol Geriatr. 2015; 48:619–624.
Article33. Singh DK, Manaf ZA, Yusoff NA, Muhammad NA, Phan MF, Shahar S. Correlation between nutritional status and comprehensive physical performance measures among older adults with undernourishment in residential institutions. Clin Interv Aging. 2014; 9:1415–1423.
Article34. de van der Schueren MA, Lonterman-Monasch S, van der Flier WM, Kramer MH, Maier AB, Muller M. Malnutrition and risk of structural brain changes seen on magnetic resonance imaging in older adults. J Am Geriatr Soc. 2016; 64:2457–2463.
Article35. Donini LM, Poggiogalle E, Molfino A, Rosano A, Lenzi A, Rossi Fanelli F, Muscaritoli M. Mini-nutritional assessment, malnutrition universal screening tool, and nutrition risk screening tool for the nutritional evaluation of older nursing home residents. J Am Med Dir Assoc. 2016; 17:959.e11–959.e18.
Article36. Chang SF. Frailty is a major related factor for at risk of malnutrition in community-dwelling older adults. J Nurs Scholarsh. 2017; 49:63–72.
Article37. Ghimire S, Baral BK, Callahan K. Nutritional assessment of communitydwelling older adults in rural Nepal. PLoS One. 2017; 12:e0172052.
Article38. Verlaan S, Ligthart-Melis GC, Wijers SL, Cederholm T, Maier AB, de van der Schueren MA. High prevalence of physical frailty among community-dwelling malnourished older adults-a systematic review and meta-analysis. J Am Med Dir Assoc. 2017; 18:374–382.
Article39. Amarya S, Singh K, Sabharwal M. Changes during aging and their association with malnutrition. J Clin Gerontol Geriatr. 2015; 6:78–84.
Article40. Camina-Martín MA, de Mateo-Silleras B, Malafarina V, Lopez-Mongil R, Niño-Martín V, López-Trigo JA, Redondo-del-Río MP. Nutritional status assessment in geriatrics: consensus declaration by the Spanish Society of Geriatrics and Gerontology Nutrition Work Group. Maturitas. 2015; 81:414–419.
Article41. Papparotto C, Bidoli E, Palese A. Risk factors associated with malnutrition in older adults living in Italian nursing homes: a cross-sectional study. Res Gerontol Nurs. 2013; 6:187–197.
Article42. O'Shea E, Trawley S, Manning E, Barrett A, Browne V, Timmons S. Malnutrition in hospitalized older adults: a multicentre observational study of prevalence, associations and outcomes. J Nutr Health Aging. 2017; 21:830–836.43. Naidoo I, Charlton KE, Esterhuizen TM, Cassim B. High risk of malnutrition associated with depressive symptoms in older South Africans living in KwaZulu-Natal, South Africa: a cross-sectional survey. J Health Popul Nutr. 2015; 33:19.
Article44. Das SK, Vasudevan DM. Biochemical diagnosis of alcoholism. Indian J Clin Biochem. 2005; 20:35–42.
Article45. Ebuehi OAT, Asonye CL. Gender and alcohol consumption affect human serum enzymes, protein and bilirubin. Asian J Biochem. 2007; 2:330–336.
Article46. Gildner TE, Liebert MA, Kowal P, Chatterji S, Josh Snodgrass J. Sleep duration, sleep quality, and obesity risk among older adults from six middle-income countries: findings from the study on global AGEing and adult health (SAGE). Am J Hum Biol. 2014; 26:803–812.
Article47. Chiang JK. Short duration of sleep is associated with elevated high-sensitivity C-reactive protein level in Taiwanese adults: a cross-sectional study. J Clin Sleep Med. 2014; 10:743–749.
Article48. Chien MY, Wang LY, Chen HC. The relationship of sleep duration with obesity and sarcopenia in community-dwelling older adults. Gerontology. 2015; 61:399–406.
Article49. Chang WC, Hsiao CF, Chang HY, Lan TY, Hsiung CA, Shih YT, Tai TY. Betel nut chewing and other risk factors associated with obesity among Taiwanese male adults. Int J Obes (Lond). 2006; 30:359–363.
Article50. Lin WY, Pi-Sunyer FX, Liu CS, Li TC, Li CI, Huang CY, Lin CC. Betel nut chewing is strongly associated with general and central obesity in Chinese male middle-aged adults. Obesity (Silver Spring). 2009; 17:1247–1254.
Article51. Chavarro-Carvajal D, Reyes-Ortiz C, Samper-Ternent R, Arciniegas AJ, Gutierrez CC. Nutritional assessment and factors associated to malnutrition in older adults: a cross-sectional study in Bogotá, Colombia. J Aging Health. 2015; 27:304–319.
Article52. Peng LN, Cheng Y, Chen LK, Tung HH, Chu KH, Liang SY. Cognition and social-physiological factors associated with malnutrition in hospitalized older adults in Taiwan. J Nurs Res. 2015; 23:1–5.
Article53. Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012; 7:287–298.54. Takeuchi K, Aida J, Ito K, Furuta M, Yamashita Y, Osaka K. Nutritional status and dysphagia risk among community-dwelling frail older adults. J Nutr Health Aging. 2014; 18:352–357.
Article55. Andre MB, Dumavibhat N, Ngatu NR, Eitoku M, Hirota R, Suganuma N. Mini Nutritional Assessment and functional capacity in community-dwelling elderly in rural Luozi, Democratic Republic of Congo. Geriatr Gerontol Int. 2013; 13:35–42.
Article56. Esmayel EM, Eldarawy MM, Hassan MM, Hassanin HM, Reda Ashour WM, Mahmoud W. Nutritional and functional assessment of hospitalized elderly: impact of sociodemographic variables. J Aging Res. 2013; 2013:101725.
Article57. Tanimoto Y, Watanabe M, Sun W, Tanimoto K, Shishikura K, Sugiura Y, Kusabiraki T, Kono K. Association of sarcopenia with functional decline in community-dwelling elderly subjects in Japan. Geriatr Gerontol Int. 2013; 13:958–963.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Risk and Its Contributing Factors in the Low-income Elderly in Urban Areas
- Characteristics of health lifestyle patterns by the quantification method
- A Study of the Health Promoting Lifestyle of the Elderly
- Socio-economic status is associated with the risk of inadequate energy intake among Korean elderly
- Psycho-Social, Nutritional Status and Meal Service Utility Patterns by Living Arrangements of the Elderly Participated in Meal Service