J Neurocrit Care.
2019 Jun;12(1):51-54. 10.18700/jnc.190075.
Status epilepticus due to cerebral air embolism after the Valsalva maneuver
- Affiliations
-
- 1Department of Neurology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea. kzoo@yuhs.ac
- KMID: 2452827
- DOI: http://doi.org/10.18700/jnc.190075
Abstract
- BACKGROUND
Cerebral air embolism is uncommon but potentially causes catastrophic events such as cardiac damage or even death. However, due to a low overall incidence, it may go undiagnosed.
CASE REPORT
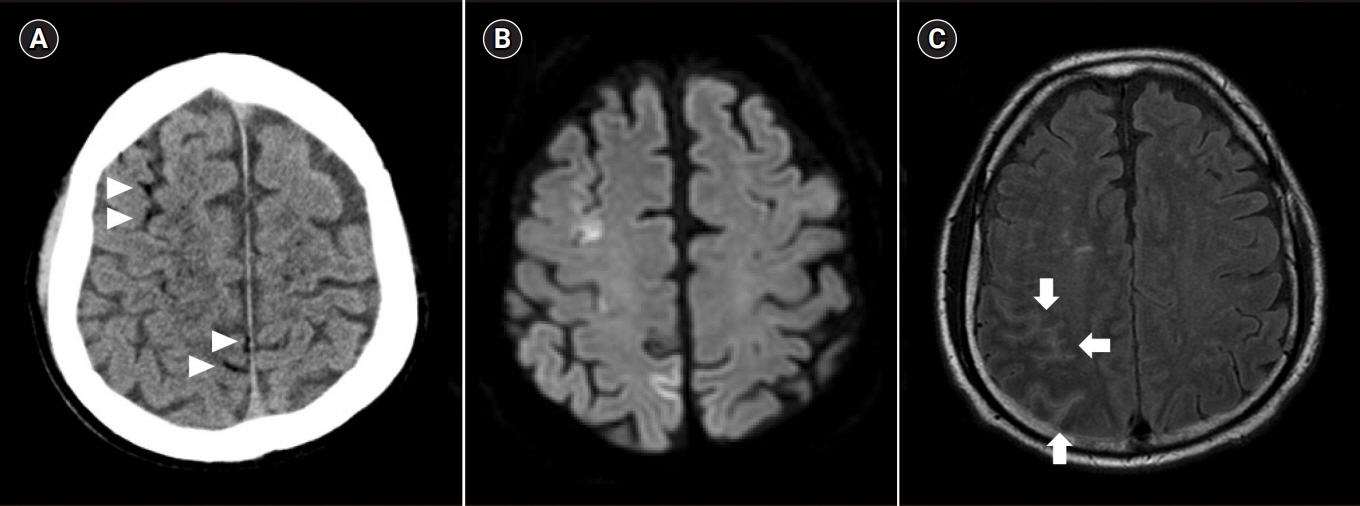
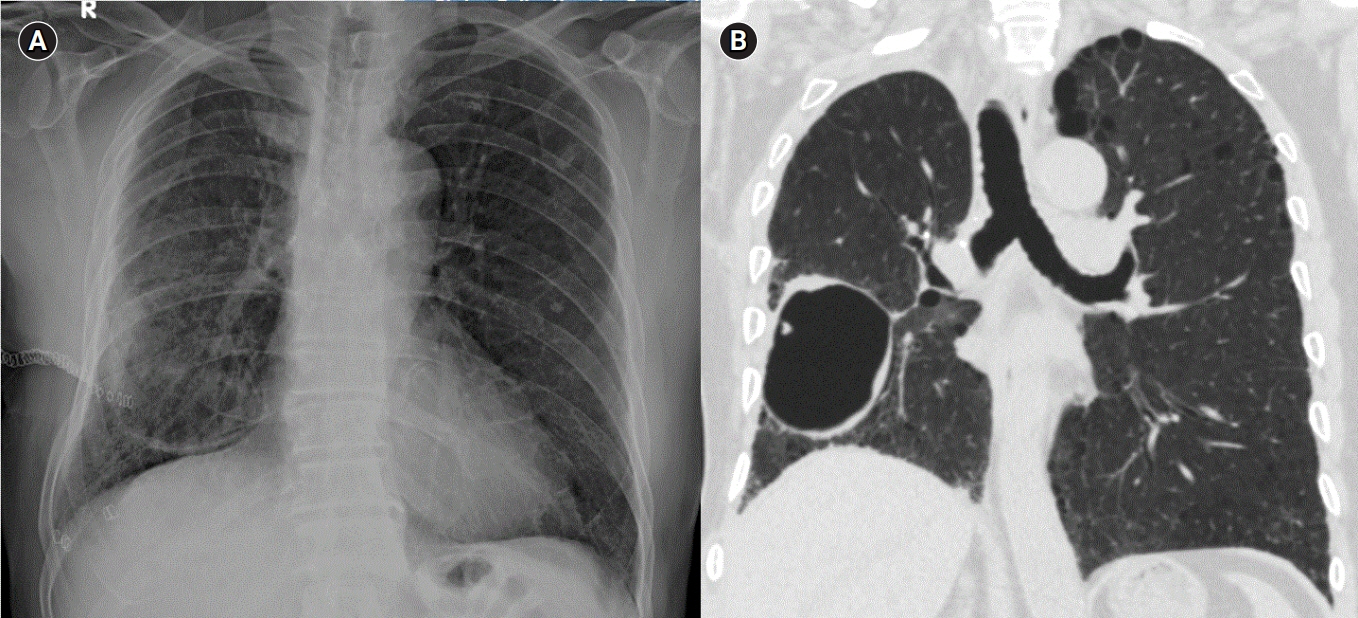
A 56-year-old man with a medical history of right upper lobectomy due to lung cancer showed changes in mental status after the Valsalva maneuver, followed by status epilepticus during admission. Brain and chest computed tomography showed cerebral air embolism and accidental pneumothorax in the right major fissure. After antiepileptic drug infusion and oxygen therapy, he recovered completely.
CONCLUSION
Since cerebral air embolism may result in fatal outcomes, it should be suspected in patients with sudden neurological deterioration after routine medical procedures.
MeSH Terms
Figure
Reference
-
1. Bou-Assaly W, Pernicano P, Hoeffner E. Systemic air embolism after transthoracic lung biopsy: a case report and review of literature. World J Radiol. 2010; 2:193–6.
Article2. Green BT, Tendler DA. Cerebral air embolism during upper endoscopy: case report and review. Gastrointest Endosc. 2005; 61:620–3.
Article3. Ho AM, Ling E. Systemic air embolism after lung trauma. Anesthesiology. 1999; 90:564–75.
Article4. Lin C, Barrio GA, Hurwitz LM, Kranz PG. Cerebral air embolism from angioinvasive cavitary aspergillosis. Case Rep Neurol Med. 2014; 2014:406106.
Article5. Akhtar N, Jafri W, Mozaffar T. Cerebral artery air embolism following an esophagogastroscopy: a case report. Neurology. 2001; 56:136–7.
Article6. Jain KK. Textbook of hyperbaric medicine. 5th ed. Cambridge: Hogrefe;2009. p. 578.7. Kim SK, Jun IG, Jang DM, Lim J, Hwang GS, Kim YK. Cerebral air embolism and subsequent transient neurologic abnormalities in a liver transplant recipient following the removal of the pulmonary artery catheter from the central venous access device: a case report. Korean J Anesthesiol. 2016; 69:80–3.
Article8. Schlimp CJ, Loimer T, Rieger M, Lederer W, Schmidts MB. The potential of venous air embolism ascending retrograde to the brain. J Forensic Sci. 2005; 50:906–9.
Article9. van Hulst RA, Klein J, Lachmann B. Gas embolism: pathophysiology and treatment. Clin Physiol Funct Imaging. 2003; 23:237–46.
Article10. Finsterer J, Stöllberger C, Bastovansky A. Cardiac and cerebral air embolism from endoscopic retrograde cholangio-pancreatography. Eur J Gastroenterol Hepatol. 2010; 22:1157–62.
Article11. Bessereau J, Genotelle N, Chabbaut C, Huon A, Tabah A, Aboab J, et al. Long-term outcome of iatrogenic gas embolism. Intensive Care Med. 2010; 36:1180–7.
Article12. Shi L, Zhang R, Wang Z, Zhou P. Delayed cerebral air embolism complicating percutaneous needle biopsy of the lung. Am J Med Sci. 2013; 345:501–3.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebral Air Embolism during Open Heart Surgery with Cardiopulmonary Bypass: A Case Report
- Cerebral Infarction During Sexual Intercourse
- Cerebral Air Embolism Following a Gastroscopy
- Cerebral air embolism after removal of internal jugular venous catheter: A case report
- An Effects of Repeated Valsalva Maneuver on Circulation of Normal Men