J Clin Neurol.
2019 Jul;15(3):369-375. 10.3988/jcn.2019.15.3.369.
Factors Affecting the Response to First-Line Treatments in Patients with Anti-N-Methyl-D-Aspartate Receptor Encephalitis
- Affiliations
-
- 1Department of Neurology, Shandong Provincial Hospital Affiliated to Shandong University, Jinan, China. guoshougang1124@163.com
- 2School of Clinical Medicine, Qilu Medical College, Shandong University, Jinan, China.
- 3Department of Radiation Oncology, Yantai Yuhuangding Hospital, Yantai, China.
- 4Department of Neurology, ENT Hospital Affiliated to Shandong University, Jinan, China.
- KMID: 2451122
- DOI: http://doi.org/10.3988/jcn.2019.15.3.369
Abstract
- BACKGROUND AND PURPOSE
Anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis is the most common type of autoimmune encephalitis. This study aimed to explore the possible factors affecting the response to first-line treatments in patients with anti-NMDAR encephalitis.
METHODS
We enrolled 29 patients who were diagnosed as anti-NMDAR encephalitis between January 1, 2015, and June 30, 2018. They were divided into the remission and nonremission groups according to their response to first-line treatments. The demographics, clinical manifestations, main ancillary examinations, follow-up treatments, and prognosis of patients were recorded. The symptoms reported on in this study occurred before treatments or during the course of first-line treatments.
RESULTS
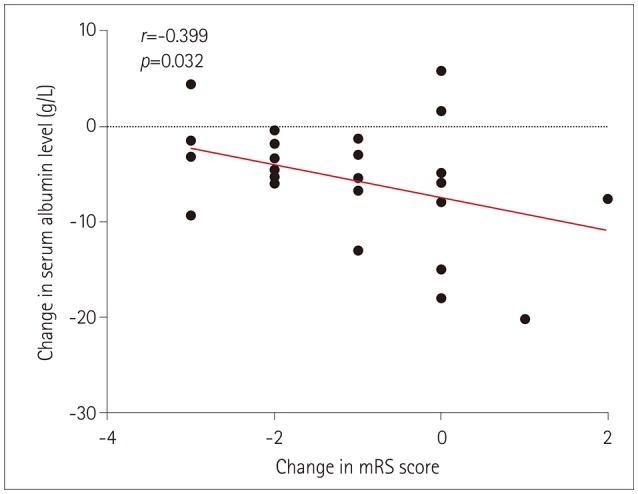
There were 18 patients (62.07%) in the remission group and 11 patients (37.93%) in the nonremission group. Compared to the remission group, a higher proportion of the patients in the nonremission group exhibited involuntary movements, decreased consciousness, central hypoventilation, lung infection, and hypoalbuminemia. The nonremission group had a high incidence of increased intracranial pressure and significant elevations of the neutrophil-to-lymphocyte ratio in peripheral blood (NLR), aspartate aminotransferase, and fibrinogen. Six patients (54.55%) in the nonremission group received second-line immunotherapy. Only one patient (3.45%) died, which was due to multiple-organ failure.
CONCLUSIONS
Anti-NMDAR-encephalitis patients with more symptoms"”especially involuntary movements, disturbance of consciousness, central hypoventilation, and accompanying hypoalbuminemia and pulmonary infection"”may respond poorly to first-line treatments. Positive second-line immunotherapy therefore needs to be considered. Admission to an intensive-care unit, increased cerebrospinal fluid pressure, and increased NLR might be the significant factors affecting the response to first-line treatments.
MeSH Terms
-
Anti-N-Methyl-D-Aspartate Receptor Encephalitis*
Aspartate Aminotransferases
Cerebrospinal Fluid Pressure
Consciousness
Demography
Dyskinesias
Encephalitis
Fibrinogen
Follow-Up Studies
Humans
Hypoalbuminemia
Hypoventilation
Immunotherapy
Incidence
Intracranial Pressure
Lung
Prognosis
Aspartate Aminotransferases
Fibrinogen
Figure
Reference
-
1. Dalmau J, Tüzün E, Wu HY, Masjuan J, Rossi JE, Voloschin A, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007; 61:25–36. PMID: 17262855.
Article2. Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 2011; 10:63–74. PMID: 21163445.
Article3. Moscato EH, Peng X, Jain A, Parsons TD, Dalmau J, Balice-Gordon RJ. Acute mechanisms underlying antibody effects in anti-N-methyl-D-aspartate receptor encephalitis. Ann Neurol. 2014; 76:108–119. PMID: 24916964.
Article4. Shin YW, Lee ST, Park KI, Jung KH, Jung KY, Lee SK, et al. Treatment strategies for autoimmune encephalitis. Ther Adv Neurol Disord. 2017; 11:1756285617722347. PMID: 29399043.
Article5. Titulaer MJ, McCracken L, Gabilondo I, Armangué T, Glaser C, Iizuka T, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013; 12:157–165. PMID: 23290630.
Article6. Balu R, McCracken L, Lancaster E, Graus F, Dalmau J, Titulaer MJ. A score that predicts 1-year functional status in patients with anti-NMDA receptor encephalitis. Neurology. 2019; 92:e244–e252. PMID: 30578370.
Article7. Broadley J, Seneviratne U, Beech P, Buzzard K, Butzkueven H, O'Brien T, et al. Prognosticating autoimmune encephalitis: a systematic review. J Autoimmun. 2019; 96:24–34. PMID: 30595145.
Article8. Jang Y, Lee ST, Kim TJ, Jun JS, Moon J, Jung KH, et al. High albumin level is a predictor of favorable response to immunotherapy in autoimmune encephalitis. Sci Rep. 2018; 8:1012. PMID: 29343812.
Article9. Zeng Z, Wang C, Wang B, Wang N, Yang Y, Guo S, et al. Prediction of neutrophil-to-lymphocyte ratio in the diagnosis and progression of autoimmune encephalitis. Neurosci Lett. 2019; 694:129–135. PMID: 30521947.
Article10. Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016; 15:391–404. PMID: 26906964.
Article11. Wang Y, Zhang W, Yin J, Lu Q, Yin F, He F, et al. Anti-N-methyl-d-aspartate receptor encephalitis in children of Central South China: clinical features, treatment, influencing factors, and outcomes. J Neuroimmunol. 2017; 312:59–65. PMID: 28935354.12. Zhang Y, Liu G, Jiang M, Chen W, He Y, Su Y. Clinical characteristics and prognosis of severe anti-N-methyl-D-aspartate receptor encephalitis patients. Neurocrit Care. 2018; 29:264–272. PMID: 29651625.
Article13. Duan BC, Weng WC, Lin KL, Wong LC, Li ST, Hsu MH, et al. Variations of movement disorders in anti-N-methyl-D-aspartate receptor encephalitis: a nationwide study in Taiwan. Medicine (Baltimore). 2016; 95:e4365. PMID: 27631202.14. Vural A, Arsava EM, Dericioglu N, Topcuoglu MA. Central neurogenic hyperventilation in anti-NMDA receptor encephalitis. Intern Med. 2012; 51:2789–2792. PMID: 23037476.
Article15. Waters KA, Machaalani R. Role of NMDA receptors in development of respiratory control. Respir Physiol Neurobiol. 2005; 149:123–130. PMID: 15908286.
Article16. Fokkink WR, Walgaard C, Kuitwaard K, Tio-Gillen AP, Van Doorn PA, Jacobs BC. Association of albumin levels with outcome in intravenous immunoglobulin-treated Guillain-Barré syndrome. JAMA Neurol. 2017; 74:189–196. PMID: 28027337.
Article17. Chi X, Wang W, Huang C, Wu M, Zhang L, Li J, et al. Risk factors for mortality in patients with anti-NMDA receptor encephalitis. Acta Neurol Scand. 2017; 136:298–304. PMID: 28028820.
Article18. Dalmau J, Tüzün E, Wu HY, Masjuan J, Rossi JE, Voloschin A, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007; 61:25–36. PMID: 17262855.
Article19. Sonderen AV, Arends S, Tavy DLJ, Bastiaansen AEM, Bruijn MAAM, Schreurs MWJ, et al. Predictive value of electroencephalography in anti-NMDA receptor encephalitis. J Neurol Neurosurg Psychiatry. 2018; 89:1101–1106. PMID: 30135187.
Article20. Wang R, Guan HZ, Ren HT, Wang W, Hong Z, Zhou D. CSF findings in patients with anti-N-methyl-D-aspartate receptor-encephalitis. Seizure. 2015; 29:137–142. PMID: 26076857.
Article21. Gresa-Arribas N, Titulaer MJ, Torrents A, Aguilar E, McCracken L, Leypoldt F, et al. Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol. 2014; 13:167–177. PMID: 24360484.
Article22. Lin J, Xue B, Li J, Xu H, Huang X, Yao Z, et al. Neutrophil to lymphocyte ratio may be a helpful marker to evaluate disease activity in NMOSD. Neurol Sci. 2017; 38:1859–1863. PMID: 28779361.
Article23. Wu Y, Chen Y, Yang X, Chen L, Yang Y. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were associated with disease activity in patients with systemic lupus erythematosus. Int Immunopharmacol. 2016; 36:94–99. PMID: 27111516.
Article24. Bisgaard AK, Pihl-Jensen G, Frederiksen JL. The neutrophil-to-lymphocyte ratio as disease actvity marker in multiple sclerosis and optic neuritis. Mult Scler Relat Disord. 2017; 18:213–217. PMID: 29141813.
Article25. Shu Y, Wang Y, Lu T, Li R, Sun X, Li J, et al. Serum uric acid and anti-N-methyl-D-aspartate receptor encephalitis. Neurochem Int. 2017; 108:34–39. PMID: 28192149.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anti-N-Methyl-D-Aspartate Receptor Encephalitis Presenting Progressive Dyslexia: A Case Report
- Anti-N-methyl-D-aspartate Receptor Encephalitis in Illicit Substance Use
- Case of anti-N-methyl D-aspartate receptor encephalitis associated with ovarian teratoma presenting as suicidal ideation
- Childhood Onset of Anti-N-Methyl-D-Aspartate Receptor Encephalitis Without Teratoma Masquerading as a Psychotic Disorder
- Anti-NMDA Receptor Encephalitis Which Has Shown Clinical Symptoms of Schizophrenia