Intest Res.
2019 Apr;17(2):273-277. 10.5217/ir.2018.00122.
Remission of diffuse ulcerative duodenitis in a patient with ulcerative colitis after infliximab therapy: a case study and review of the literature
- Affiliations
-
- 1Department of Gastroenterology, Daehang Hospital, Seoul, Korea. yschoi427@naver.com
- 2Department of Pathology, Daehang Hospital, Seoul, Korea.
- KMID: 2449969
- DOI: http://doi.org/10.5217/ir.2018.00122
Abstract
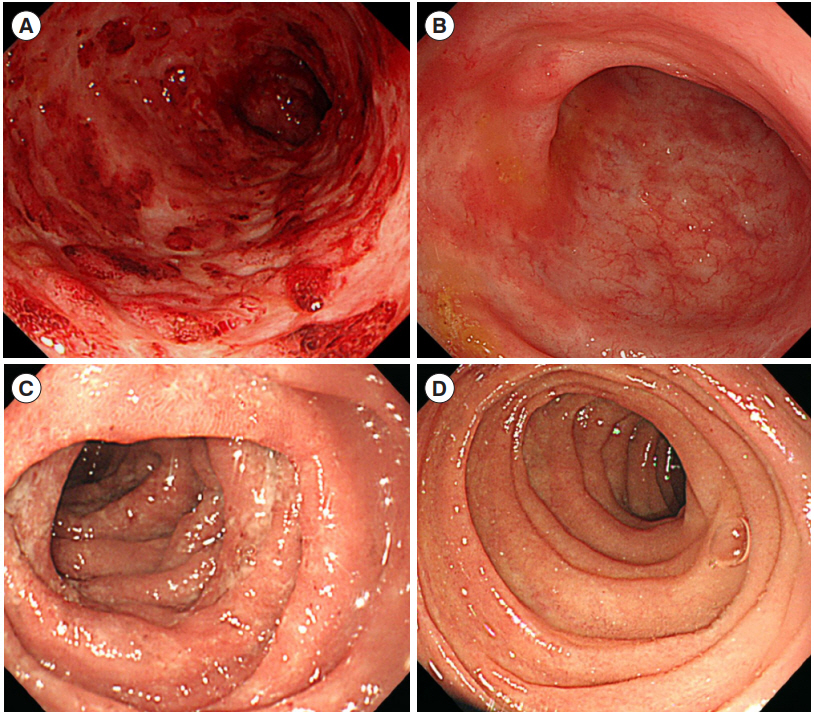
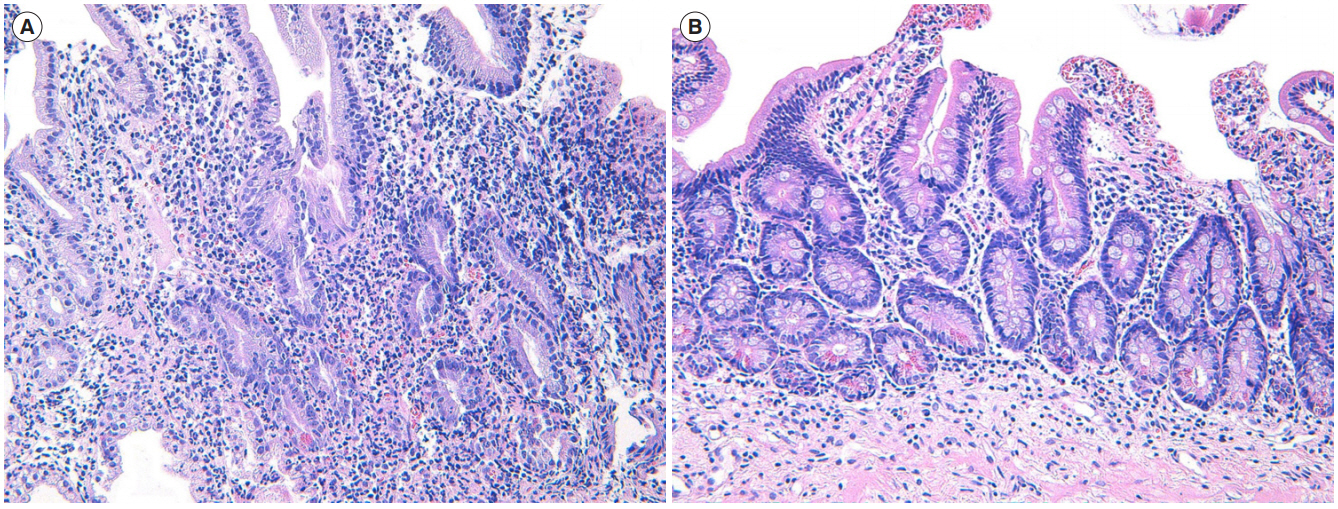
- Although ulcerative colitis (UC) is confined to colonic and rectal mucosa in a continuous fashion, recent studies have also demonstrated the involvement of upper gastrointestinal tract as diagnostic endoscopy becomes more available and technically advanced. The pathogenesis of UC is not well established yet. It might be associated with an inappropriate response of host mucosal immune system to gut microflora. Although continuous and symmetric distribution of mucosal inflammation from rectum to colon is a typical pattern of UC, clinical feature and course of atypically distributed lesions in UC might also help us understand the pathogenesis of UC. Herein, we report a case of duodenal involvement of UC which successfully remitted after infliximab therapy. Endoscopic and pathologic findings before and after administration of anti-tumor necrosis factor suggest that the pathogenesis of upper gastrointestinal involvement of UC may be similar to that of colon involvement.
Keyword
MeSH Terms
Figure
Reference
-
1. Mutinga ML, Odze RD, Wang HH, Hornick JL, Farraye FA. The clinical significance of right-sided colonic inflammation in patients with left-sided chronic ulcerative colitis. Inflamm Bowel Dis. 2004; 10:215–219.
Article2. Choi YS, Kim WJ, Kim JK, Kim DS, Lee DH. Efficacy of topical 5-aminosalicylate monotherapy in patients with ulcerative proctitis with skip inflammation. J Gastroenterol Hepatol. 2018; 33:1200–1206.
Article3. Ruuska T, Vaajalahti P, Arajärvi P, Mäki M. Prospective evaluation of upper gastrointestinal mucosal lesions in children with ulcerative colitis and Crohn’s disease. J Pediatr Gastroenterol Nutr. 1994; 19:181–186.
Article4. Kaufman SS, Vanderhoof JA, Young R, Perry D, Raynor SC, Mack DR. Gastroenteric inflammation in children with ulcerative colitis. Am J Gastroenterol. 1997; 92:1209–1212.5. Mitomi H, Atari E, Uesugi H, et al. Distinctive diffuse duodenitis associated with ulcerative colitis. Dig Dis Sci. 1997; 42:684–693.6. Thompson JW 3rd, Bargen JA. Ulcerative duodenitis and chronic ulcerative colitis: report of two cases. Gastroenterology. 1960; 38:452–455.
Article7. Valdez R, Appelman HD, Bronner MP, Greenson JK. Diffuse duodenitis associated with ulcerative colitis. Am J Surg Pathol. 2000; 24:1407–1413.
Article8. Terashima S, Hoshino Y, Kanzaki N, Kogure M, Gotoh M. Ulcerative duodenitis accompanying ulcerative colitis. J Clin Gastroenterol. 2001; 32:172–175.
Article9. Rubenstein J, Sherif A, Appelman H, Chey WD. Ulcerative colitis associated enteritis: is ulcerative colitis always confined to the colon? J Clin Gastroenterol. 2004; 38:46–51.10. Kawai K, Watanabe T, Nakayama H, Roberts-Thomson I, Nagawa H. Images of interest. Gastrointestinal: small bowel inflammation and ulcerative colitis. J Gastroenterol Hepatol. 2005; 20:1791.
Article11. Hori K, Ikeuchi H, Nakano H, et al. Gastroduodenitis associated with ulcerative colitis. J Gastroenterol. 2008; 43:193–201.
Article12. Akitake R, Nakase H, Tamaoki M, Ueno S, Mikami S, Chiba T. Modulation of Th1/Th2 balance by infliximab rescues postoperative occurrence of small-intestinal inflammation associated with ulcerative colitis. Dig Dis Sci. 2010; 55:1781–1784.
Article13. Hisabe T, Matsui T, Miyaoka M, et al. Diagnosis and clinical course of ulcerative gastroduodenal lesion associated with ulcerative colitis: possible relationship with pouchitis. Dig Endosc. 2010; 22:268–274.
Article14. Lin J, McKenna BJ, Appelman HD. Morphologic findings in upper gastrointestinal biopsies of patients with ulcerative colitis: a controlled study. Am J Surg Pathol. 2010; 34:1672–1677.
Article15. Chiba M, Ono I, Wakamatsu H, Wada I, Suzuki K. Diffuse gastroduodenitis associated with ulcerative colitis: treatment by infliximab. Dig Endosc. 2013; 25:622–625.
Article16. Willington AJ, Taylor G, White J, Gearry RB. Gastrointestinal: ulcerative colitis-associated duodenitis. J Gastroenterol Hepatol. 2018; 33:973.
Article17. Byeon JS, Yang SK, Myung SJ, et al. Clinical course of distal ulcerative colitis in relation to appendiceal orifice inflammation status. Inflamm Bowel Dis. 2005; 11:366–371.
Article18. Naves JE, Lorenzo-Zúñiga V, Marín L, et al. Long-term outcome of patients with distal ulcerative colitis and inflammation of the appendiceal orifice. J Gastrointestin Liver Dis. 2011; 20:355–358.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Golimumab Therapy in Ulcerative Colitis
- A case of ulcerative duodenitis accompanying ulcerative colitis
- Advances in ulcerative colitis therapy
- What to do when traditional rescue therapies fail in acute severe ulcerative colitis
- Optic Neuritis after Infliximab Treatment in a Patient with Ulcerative Colitis