J Korean Med Assoc.
2019 Jun;62(6):325-332. 10.5124/jkma.2019.62.6.325.
Diagnosis and treatment of childhood strabismus
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 2Department of Ophthalmology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. jaeho.jung@snu.ac.kr
- KMID: 2449580
- DOI: http://doi.org/10.5124/jkma.2019.62.6.325
Abstract
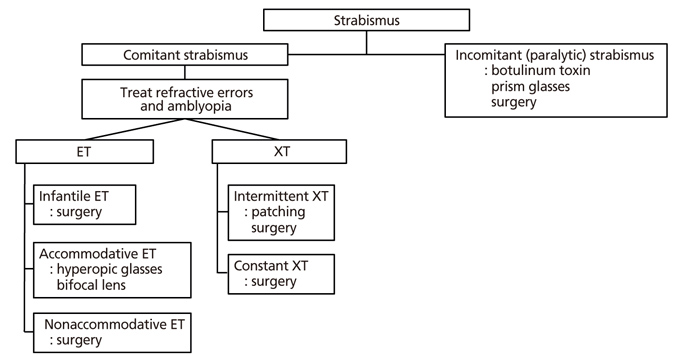
- Strabismus is a pathologic condition in which the eyes do not properly align with each other forming different images on the corresponding retinal points. Early diagnosis and appropriate management of strabismus in the sensitive period of visual maturation is critical for the development of normal binocular vision in children. Therefore, it is important to perform ophthalmologic examinations including cycloplegic refraction and ocular alignment as early as possible to detect risk factors for amblyopia and strabismus. Strabismus could also be a sign of intraocular pathology, brain diseases or myasthenia gravis which may require urgent treatment. Strabismus can be treated by surgical and non-surgical methods. The first step in the management of strabismus is to correct amblyogenic refractive errors and prescribe glasses if necessary. Bifocal lenses, prism glasses, occlusion therapy, and botulinum toxin injection could also be considered. Surgery is usually performed if non-surgical treatments are unsuccessful. Making an accurate diagnosis and setting practical goals and limitations of treatment is the key to success in the treatment of strabismus.
Keyword
MeSH Terms
Figure
Reference
-
1. Korean Strabismus and Pediatric Ophthalmological Society. Current concepts in strabismus. 4th ed. Seoul: Naewae Haksool;2018.2. Robaei D, Rose KA, Kifley A, Cosstick M, Ip JM, Mitchell P. Factors associated with childhood strabismus: findings from a population-based study. Ophthalmology. 2006; 113:1146–1153.3. Han KE, Baek SH, Kim SH, Lim KH. Epidemiologic Survey Committee of the Korean Ophthalmological Society. Prevalence and risk factors of strabismus in children and adolescents in South Korea: Korea National Health and Nutrition Examination Survey, 2008–2011. PLoS One. 2018; 13:e0191857.
Article4. Williams C, Northstone K, Howard M, Harvey I, Harrad RA, Sparrow JM. Prevalence and risk factors for common vision problems in children: data from the ALSPAC study. Br J Ophthalmol. 2008; 92:959–964.
Article5. Ehrlich JR, Anthopolos R, Tootoo J, Andrews CA, Miranda ML, Lee PP, Musch DC, Stein JD. Assessing geographic variation in strabismus diagnosis among children enrolled in Medicaid. Ophthalmology. 2016; 123:2013–2022.
Article6. Greenberg AE, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood esotropia: a population-based study. Ophthalmology. 2007; 114:170–174.7. Kim JH, Hwang JM. Presence of the abducens nerve according to the type of Duane's retraction syndrome. Ophthalmology. 2005; 112:109–113.
Article8. Kim JH, Hwang JM. Abducens nerve is present in patients with type 2 Duane's retraction syndrome. Ophthalmology. 2012; 119:403–406.
Article9. Yang HK, Kim JH, Hwang JM. Abducens nerve in patients with type 3 Duane's retraction syndrome. PLoS One. 2016; 11:e0150670.
Article10. Lee JE, Yang HK, Kim JH, Hwang JM. Diagnostic utility of the three-step test according to the presence of the trochlear nerve in superior oblique palsy. J Clin Neurol. 2018; 14:66–72.
Article11. Manchandia AM, Demer JL. Sensitivity of the three-step test in diagnosis of superior oblique palsy. J AAPOS. 2014; 18:567–571.
Article12. Wallace DK, Repka MX, Lee KA, Melia M, Christiansen SP, Morse CL, Sprunger DT. American Academy of Pediatric Ophthalmology/Strabismus Preferred Practice Pattern Pediatric Ophthalmology Panel. Amblyopia preferred practice pattern. Ophthalmology. 2018; 125:P105–P142.
Article13. Huang D, Chen X, Zhang X, Wang Y, Zhu H, Ding H, Bai J, Chen J, Fu Z, Wang Z, Liu H. Pediatric vision screening using the plusoptiX A12C photoscreener in Chinese preschool children aged 3 to 4 years. Sci Rep. 2017; 7:2041.
Article14. Dahlmann-Noor AH, Vrotsou K, Kostakis V, Brown J, Heath J, Iron A, McGill S, Vivian AJ. Vision screening in children by Plusoptix Vision Screener compared with gold-standard orthoptic assessment. Br J Ophthalmol. 2009; 93:342–345.
Article15. Dahlmann-Noor AH, Comyn O, Kostakis V, Misra A, Gupta N, Heath J, Brown J, Iron A, McGill S, Vrotsou K, Vivian AJ. Plusoptix Vision Screener: the accuracy and repeatability of refractive measurements using a new autorefractor. Br J Ophthalmol. 2009; 93:346–349.
Article16. Rowatt AJ, Donahue SP, Crosby C, Hudson AC, Simon S, Emmons K. Field evaluation of the Welch Allyn SureSight vision screener: incorporating the vision in preschoolers study recommendations. J AAPOS. 2007; 11:243–248.
Article17. Yang HK, Kim JH, Hwang JM. Congenital superior oblique palsy and trochlear nerve absence: a clinical and radiological study. Ophthalmology. 2012; 119:170–177.
Article18. Kim N, Yang HK, Kim JH, Hwang JM. Comparison of clinical and radiological findings between congenital orbital fibrosis and congenital fibrosis of the extraocular muscles. Curr Eye Res. 2018; 43:1471–1476.
Article19. von Noorden GK. Principles of nonsurgical treatment. In : von Noorden GK, Campos EC, editors. Binocular vision and ocular motility. St Louis: Mosby;2002. p. 537–553.20. Horwood AM, Riddell PM. Evidence that convergence rather than accommodation controls intermittent distance exotropia. Acta Ophthalmol. 2012; 90:e109–e117.
Article21. Thurtell MJ, Leigh RJ. Therapy for nystagmus. J Neuroophthalmol. 2010; 30:361–371.
Article22. Lavrich JB. Intermittent exotropia: continued controversies and current management. Curr Opin Ophthalmol. 2015; 26:375–381.23. Williams HP. Comparison of the accommodative effects of carbachol and pilocarpine with reference to accommodative esotropia. Br J Ophthalmol. 1974; 58:668–673.
Article24. Wright KW. Strabismus management. Curr Opin Ophthalmol. 1994; 5:25–29.
Article25. Scott AB. Botulinum toxin injection into extraocular muscles as an alternative to strabismus surgery. J Pediatr Ophthalmol Strabismus. 1980; 17:21–25.
Article26. Rowe FJ, Noonan CP. Botulinum toxin for the treatment of strabismus. Cochrane Database Syst Rev. 2009; (2):CD006499.
Article27. Rosenbaum AL, Metz HS. Diagnosis of lost or slipped muscle by saccadic velocity measurements. Am J Ophthalmol. 1974; 77:215–222.
Article28. Pineles SL, Chang MY, Oltra EL, Pihlblad MS, Davila-Gonzalez JP, Sauer TC, Velez FG. Anterior segment ischemia: etiology, assessment, and management. Eye (Lond). 2018; 32:173–178.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Analysis of Reoperation for Strabismus after Strabismus Surgery in Childhood
- Long-standing Adult Horizontal Strabismus with Early Childhood Onset
- Long-standing Adult Horizontal Strabismus with Early Childhood Onset
- Result of Initial Botulinum Toxin Injection in Childhood Horizontal Strabismus
- Statistical Obserbations of Comitant Horizontal Squint Surgery