Acute Crit Care.
2019 Feb;34(1):30-37. 10.4266/acc.2018.00318.
Application of Sepsis-3 Criteria to Korean Patients with Critical Illnesses
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Hallym University Medical Center, Anyang, Korea.
- 3Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Anesthesiology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 5Department of Internal Medicine, St. Paul's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 6Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea.
- 7Department of Anesthesia and Pain Medicine, Pusan National University School of Medicine, Busan, Korea.
- 8Department of Anesthesia and Pain Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 9Department of Anesthesiology and Pain Medicine, Seoul National University College of Medicine, Seoul, Korea.
- 10Department of Software Convergence, Seoul Women's University, Seoul, Korea.
- 11Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. yskoh@amc.seoul.kr
- KMID: 2449377
- DOI: http://doi.org/10.4266/acc.2018.00318
Abstract
- BACKGROUND
The 2016 Society of Critical Care Medicine (SCCM)/European Society of Intensive Care Medicine (ESICM) task force for Sepsis-3 devised new definitions for sepsis, sepsis with organ dysfunction and septic shock. Although Sepsis-3 was data-driven, evidence-based approach, East Asian descents comprised minor portions of the project population.
METHODS
We selected Korean participants from the fever and antipyretics in critically ill patients evaluation (FACE) study, a joint study between Korea and Japan. We calculated the concordance rates for sepsis diagnosis between Sepsis-2 and Sepsis-3 criteria and evaluated mortality rates of sepsis, sepsis with organ dysfunction, and septic shock by Sepsis-3 criteria using the selected data.
RESULTS
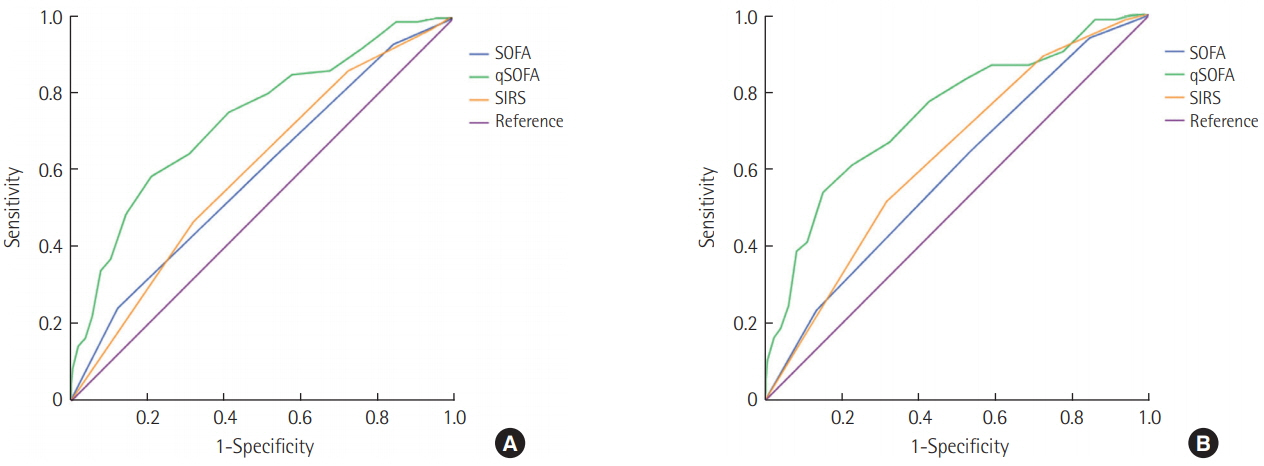
Korean participants of the FACE study were 913 (383 with sepsis and 530 without sepsis by Sepsis-2 criteria). The concordance rate for sepsis diagnosis between Sepsis-2 and Sepsis-3 criteria was 55.4%. The intensive care unit (ICU) and 28-day mortality rates of sepsis, sepsis with organ dysfunction, and septic shock patients according to Sepsis-3 criteria were 26.2% and 31.0%, 27.5% and 32.5%, and 40.8% and 43.4%, respectively. The quick Sequential Organ Failure Assessment (qSOFA) was inferior not only to SOFA but also to systemic inflammatory response syndrome (SIRS) for predicting ICU and 28-day mortality.
CONCLUSIONS
The concordance rates for sepsis diagnosis between Sepsis-2 and Sepsis-3 criteria were low. Mortality rate for septic shock in Koreans was consistent with estimates made by the 2016 SCCM/ESICM task force. SOFA and SIRS were better than qSOFA for predicting ICU and 28-day mortality in Korean ICU patients.
Keyword
MeSH Terms
Figure
Reference
-
1. American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992; 20:864–74.2. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003; 31:1250–6.
Article3. Shankar-Hari M, Phillips GS, Levy ML, Seymour CW, Liu VX, Deutschman CS, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016; 315:775–87.4. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016; 315:801–10.
Article5. Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of Clinical Criteria for Sepsis: for the third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016; 315:762–74.6. Lee BH, Inui D, Suh GY, Kim JY, Kwon JY, Park J, et al. Association of body temperature and antipyretic treatments with mortality of critically ill patients with and without sepsis: multi-centered prospective observational study. Crit Care. 2012; 16:R33.
Article7. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992; 101:1644–55.8. Fernando SM, Tran A, Taljaard M, Cheng W, Rochwerg B, Seely AJ, et al. Prognostic accuracy of the quick sequential organ failure assessment for mortality in patients with suspected infection: a systematic review and meta-analysis. Ann Intern Med. 2018; 168:266–75.9. Raith EP, Udy AA, Bailey M, McGloughlin S, MacIsaac C, Bellomo R, et al. Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017; 317:290–300.
Article10. Casserly B, Phillips GS, Schorr C, Dellinger RP, Townsend SR, Osborn TM, et al. Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database. Crit Care Med. 2015; 43:567–73.11. Cecconi M, De Backer D, Antonelli M, Beale R, Bakker J, Hofer C, et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 2014; 40:1795–815.
Article12. Park DW, Chun BC, Kim JM, Sohn JW, Peck KR, Kim YS, et al. Epidemiological and clinical characteristics of communityacquired severe sepsis and septic shock: a prospective observational study in 12 university hospitals in Korea. J Korean Med Sci. 2012; 27:1308–14.
Article13. Ryoo SM, Kang GH, Shin TG, Hwang SY, Kim K, Jo YH, et al. Clinical outcome comparison of patients with septic shock defined by the new sepsis-3 criteria and by previous criteria. J Thorac Dis. 2018; 10:845–53.
Article