Int J Thyroidol.
2019 May;12(1):19-27. 10.11106/ijt.2019.12.1.19.
The Prognostic Value of Central Lymph Node Yield and Ratio in Papillary Thyroid Carcinoma Patients Who Underwent Thyroidectomy with Prophylactic Central Compartment Neck Dissection
- Affiliations
-
- 1Division of Thyroid & Endocrine Surgery, Department of Surgery, Eunpyeong St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Division of Thyroid & Endocrine Surgery, Department of Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. drbae@catholic.ac.kr
- KMID: 2449062
- DOI: http://doi.org/10.11106/ijt.2019.12.1.19
Abstract
- BACKGROUND AND OBJECTIVES
The impacts of prophylactic central compartment neck dissection (pCCND) on the prognosis of papillary thyroid cancer (PTC) are controversial. The aim of this study is to evaluate the relationship between nodal factors of pCCND and the prognosis of PTC patients.
MATERIALS AND METHODS
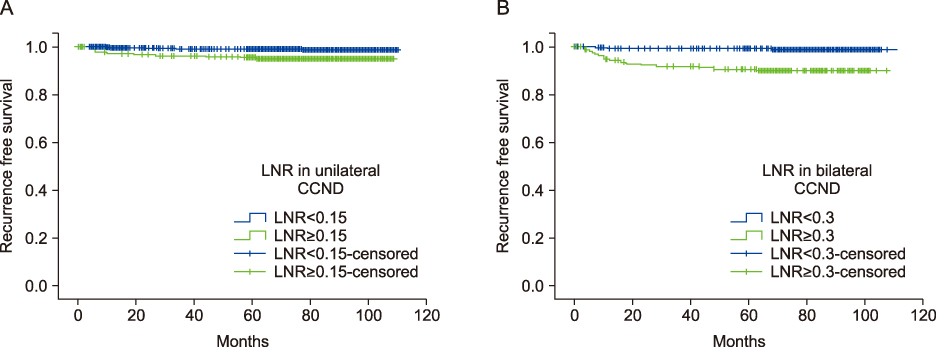
A total of 1754 patients who underwent thyroidectomy with pCCND were retrospectively reviewed. Nodal factor was defined as the number of metastatic lymph node (MLN), lymph node yield (LNY) and lymph node ratio (LNR). In regarding the cutoff of nodal factors, patients were categorized as low/high MLN, LNR and LNY group. The correlation of clinicopathologic characteristics including nodal factors and recurrence free survival (RFS) were anlalyzed.
RESULTS
Of these, 1195 patients underwent thyroidectomy with unilateral pCCND and 559 patients underwent total thyroidectomy with bilateral pCCND. During follow-up, 45 (2.57%) patients showed recurrent disease. Of these, 19 patients underwent bilateral pCCND and 26 cases were unilateral pCCND. Gross extrathyroidal extension (ETE), high MLN and LNR showed statistically significant on RFS in univariate analysis in unilateral pCCND. In multivariate analysis, gross ETE and high LNR were independent risk factor of recurrence in unilateral pCCND. In bilateral pCCND, larger tumor size, minimal ETE, high MLN and LNR were significant correlation with RFS in univariate analysis. However, in multivariate analysis, multiple larger tumor and high LNR showed significant correlation with RFS. LNY was not statistically significant in both unilateral and bilateral pCCND.
CONCLUSION
In regarding nodal factors, high LNR was only independent risk factor to worse RFS in both unilateral and bilateral pCCND in cN0 PTC patients.
MeSH Terms
Figure
Reference
-
1. Smith PW, Hanks LR, Salomone LJ, Hanks JB. Thyroid. In : Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Sabiston textbook of surgery: The biological basis of modern surgical practice. 20th ed. Philadelphia, PA: Elsevier;2017. p. 881–992.2. Shigematsu N, Takami H, Ito N, Kubo A. Nationwide survey on the treatment policy for well-differentiated thyroid cancer -- results of a questionnaire distributed at the 37th meeting of the Japanese Society of Thyroid Surgery. Endocr J. 2005; 52(4):479–491.
Article3. American Thyroid Association Surgery Working Group. American Association of Endocrine Surgeons. American Academy of Otolaryngology-Head and Neck Surgery. American Head and Neck Society. Carty SE, Cooper DS, et al. Consensus statement on the terminology and classification of central neck dissection for thyroid cancer. Thyroid. 2009; 19(11):1153–1158.
Article4. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26(1):1–133.
Article5. Barczynski M, Konturek A, Stopa M, Nowak W. Prophylactic central neck dissection for papillary thyroid cancer. Br J Surg. 2013; 100(3):410–418.
Article6. Amit M, Tam S, Boonsripitayanon M, Cabanillas ME, Busaidy NL, Grubbs EG, et al. Association of lymph node density with survival of patients with papillary thyroid cancer. JAMA Otolaryngol Head Neck Surg. 2018; 144(2):108–114.
Article7. Kim Y, Roh JL, Gong G, Cho KJ, Choi SH, Nam SY, et al. Risk factors for lateral neck recurrence of N0/N1a papillary thyroid cancer. Ann Surg Oncol. 2017; 24(12):3609–3616.
Article8. Nam SH, Roh JL, Gong G, Cho KJ, Choi SH, Nam SY, et al. Nodal factors predictive of recurrence after thyroidectomy and neck dissection for papillary thyroid carcinoma. Thyroid. 2018; 28(1):88–95.
Article9. Heaton CM, Chang JL, Orloff LA. Prognostic implications of lymph node yield in central and lateral neck dissections for well-differentiated papillary thyroid carcinoma. Thyroid. 2016; 26(3):434–440.
Article10. Popadich A, Levin O, Lee JC, Smooke-Praw S, Ro K, Fazel M, et al. A multicenter cohort study of total thyroidectomy and routine central lymph node dissection for cN0 papillary thyroid cancer. Surgery. 2011; 150(6):1048–1057.
Article11. Hartl DM, Mamelle E, Borget I, Leboulleux S, Mirghani H, Schlumberger M. Influence of prophylactic neck dissection on rate of retreatment for papillary thyroid carcinoma. World J Surg. 2013; 37(8):1951–1958.
Article12. Leboulleux S, Rubino C, Baudin E, Caillou B, Hartl DM, Bidart JM, et al. Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab. 2005; 90(10):5723–5729.
Article13. Podnos YD, Smith D, Wagman LD, Ellenhorn JD. The implication of lymph node metastasis on survival in patients with well-differentiated thyroid cancer. Am Surg. 2005; 71(9):731–734.
Article14. American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee LS, et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009; 19(11):1167–1214.
Article15. Enyioha C, Roman SA, Sosa JA. Central lymph node dissection in patients with papillary thyroid cancer: A population level analysis of 14,257 cases. Am J Surg. 2013; 205(6):655–661.
Article16. Grodski S, Cornford L, Sywak M, Sidhu S, Delbridge L. Routine level VI lymph node dissection for papillary thyroid cancer: surgical technique. ANZ J Surg. 2007; 77(4):203–208.
Article17. Moo TA, McGill J, Allendorf J, Lee J, Fahey T 3rd, Zarnegar R. Impact of prophylactic central neck lymph node dissection on early recurrence in papillary thyroid carcinoma. World J Surg. 2010; 34(6):1187–1191.
Article18. Kouvaraki MA, Shapiro SE, Fornage BD, Edeiken-Monro BS, Sherman SI, Vassilopoulou-Sellin R, et al. Role of preoperative ultrasonography in the surgical management of patients with thyroid cancer. Surgery. 2003; 134(6):946–954. discussion 54–5.
Article19. Roh JL, Kim JM, Park CI. Central lymph node metastasis of unilateral papillary thyroid carcinoma: patterns and factors predictive of nodal metastasis, morbidity, and recurrence. Ann Surg Oncol. 2011; 18(8):2245–2250.
Article20. Roh JL, Park JY, Park CI. Total thyroidectomy plus neck dissection in differentiated papillary thyroid carcinoma patients: Pattern of nodal metastasis, morbidity, recurrence, and postoperative levels of serum parathyroid hormone. Ann Surg. 2007; 245(4):604–610.
Article21. Sywak M, Cornford L, Roach P, Stalberg P, Sidhu S, Delbridge L. Routine ipsilateral level VI lymphadenectomy reduces postoperative thyroglobulin levels in papillary thyroid cancer. Surgery. 2006; 140(6):1000–1005. discussion 5–7.
Article22. Ito Y, Miyauchi A, Masuoka H, Fukushima M, Kihara M, Miya A. Excellent prognosis of central lymph node recurrence-free survival for cN0M0 papillary thyroid carcinoma patients who underwent routine prophylactic central node dissection. World J Surg. 2018; 42(8):2462–2468.
Article23. Zheng CM, Ji YB, Song CM, Ge MH, Tae K. Number of metastatic lymph nodes and ratio of metastatic lymph nodes to total number of retrieved lymph nodes are risk factors for recurrence in patients with clinically node negative papillary thyroid carcinoma. Clin Exp Otorhinolaryngol. 2018; 11(1):58–64.
Article24. Park YM, Wang SG, Lee JC, Shin DH, Kim IJ, Son SM, et al. Metastatic lymph node status in the central compartment of papillary thyroid carcinoma: A prognostic factor of locoregional recurrence. Head Neck. 2016; 38:Suppl 1. E1172–E1176.
Article25. Vas Nunes JH, Clark JR, Gao K, Chua E, Campbell P, Niles N, et al. Prognostic implications of lymph node yield and lymph node ratio in papillary thyroid carcinoma. Thyroid. 2013; 23(7):811–816.
Article26. Schneider DF, Mazeh H, Chen H, Sippel RS. Lymph node ratio predicts recurrence in papillary thyroid cancer. Oncologist. 2013; 18(2):157–162.
Article27. Schneider DF, Chen H, Sippel RS. Impact of lymph node ratio on survival in papillary thyroid cancer. Ann Surg Oncol. 2013; 20(6):1906–1911.
Article28. Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL, et al. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 2012; 22(11):1144–1152.
Article29. Beal SH, Chen SL, Schneider PD, Martinez SR. An evaluation of lymph node yield and lymph node ratio in well-differentiated thyroid carcinoma. Am Surg. 2010; 76(1):28–32.
Article30. Lai V, Yen TW, Rose BT, Fareau GG, Misustin SM, Evans DB, et al. The effect of thyroiditis on the yield of central compartment lymph nodes in patients with papillary thyroid cancer. Ann Surg Oncol. 2015; 22(13):4181–4186.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Prophylactic Central Neck Dissection During Hemithyroidectomy on Locoregional Recurrence in Patients With Papillary Thyroid Carcinoma: A Meta-Analysis
- Incidence and Predictive Factors of Central Neck Node Metastasis in Patients with T1, T2 Papillary Thyroid Cancer
- Feasibility of Sentinel Lymph Node Biopsy in Papillary Thyroid Carcinoma
- Surgical Treatment for Papillary Thyroid Carcinoma in Japan: Differences from Other Countries
- Regional Lymph Node Metastasis in Papillary Thyroid Cancer