Clin Exp Otorhinolaryngol.
2020 May;13(2):194-202. 10.21053/ceo.2019.01634.
The Effect of Prophylactic Central Neck Dissection During Hemithyroidectomy on Locoregional Recurrence in Patients With Papillary Thyroid Carcinoma: A Meta-Analysis
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2500293
- DOI: http://doi.org/10.21053/ceo.2019.01634
Abstract
Objectives
. Hemithyroidectomy is commonly performed in patients with low- to intermediate-risk papillary thyroid carcinoma. The purpose of this meta-analysis was to evaluate the effect of prophylactic central neck dissection on locoregional recurrence in patients undergoing hemithyroidectomy.
Methods
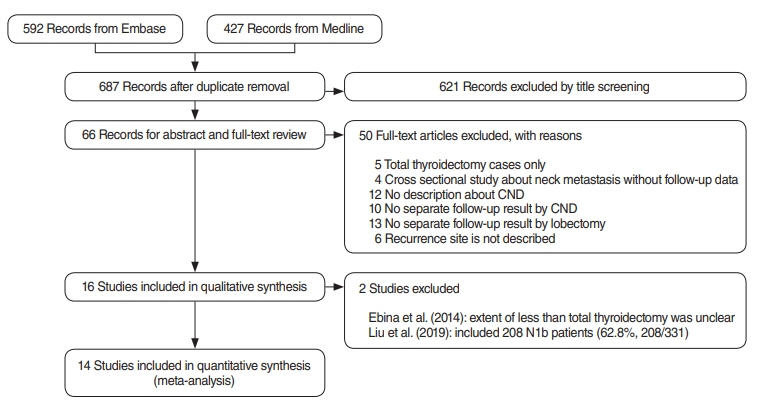
. A meta-analysis was performed of full-text publications published in English retrieved from the Embase database.
Results
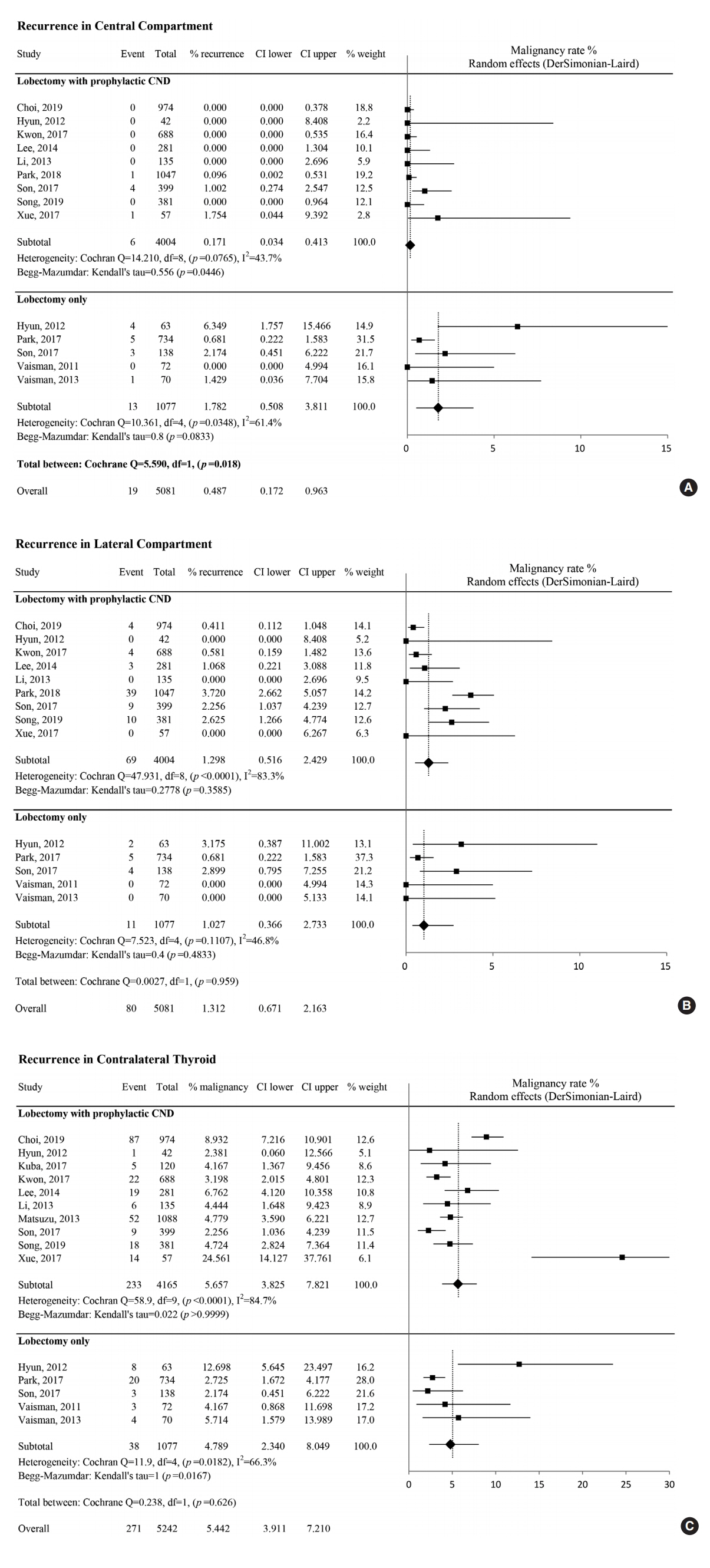
. The rate of regional recurrence in the central compartment after hemithyroidectomy, with or without prophylactic central neck dissection, was 0.17% and 1.78%, respectively. This difference was statistically significant. Recurrence in the lateral compartment or contralateral thyroid was not affected by prophylactic central neck dissection; the overall rate of recurrence was 1.3% and 5.4%, respectively.
Conclusion
. Prophylactic central neck dissection significantly reduced the risk of recurrence in the central compartment in patients undergoing hemithyroidectomy.
Keyword
Figure
Cited by 1 articles
-
Transcriptomic Analysis of Papillary Thyroid Cancer: A Focus on Immune-Subtyping, Oncogenic Fusion, and Recurrence
Seung-Jin Park, Yea Eun Kang, Jeong-Hwan Kim, Jong-Lyul Park, Seon-Kyu Kim, Seung-Woo Baek, In Sun Chu, Shinae Yi, Seong Eun Lee, Young Joo Park, Eun-Jae Chung, Jin Man Kim, Hye Mi Ko, Je-Ryong Kim, Seung-Nam Jung, Ho-Ryun Won, Jae Won Chang, Bon Seok Koo, Seon-Young Kim
Clin Exp Otorhinolaryngol. 2022;15(2):183-193. doi: 10.21053/ceo.2021.02215.
Reference
-
1. Mendelsohn AH, Elashoff DA, Abemayor E, St John MA. Surgery for papillary thyroid carcinoma: is lobectomy enough? Arch Otolaryngol Head Neck Surg. 2010; Nov. 136(11):1055–61.2. Barney BM, Hitchcock YJ, Sharma P, Shrieve DC, Tward JD. Overall and cause-specific survival for patients undergoing lobectomy, near-total, or total thyroidectomy for differentiated thyroid cancer. Head Neck. 2011; May. 33(5):645–9.
Article3. Koo BS, Choi EC, Yoon YH, Kim DH, Kim EH, Lim YC. Predictive factors for ipsilateral or contralateral central lymph node metastasis in unilateral papillary thyroid carcinoma. Ann Surg. 2009; May. 249(5):840–4.
Article4. Roh JL, Kim JM, Park CI. Central lymph node metastasis of unilateral papillary thyroid carcinoma: patterns and factors predictive of nodal metastasis, morbidity, and recurrence. Ann Surg Oncol. 2011; Aug. 18(8):2245–50.
Article5. Hughes DT, Rosen JE, Evans DB, Grubbs E, Wang TS, Solorzano CC. Prophylactic central compartment neck dissection in papillary thyroid cancer and effect on locoregional recurrence. Ann Surg Oncol. 2018; Sep. 25(9):2526–34.
Article6. Chen L, Wu YH, Lee CH, Chen HA, Loh EW, Tam KW. Prophylactic central neck dissection for papillary thyroid carcinoma with clinically uninvolved central neck lymph nodes: a systematic review and meta-analysis. World J Surg. 2018; Sep. 42(9):2846–57.
Article7. Zhao WJ, Luo H, Zhou YM, Dai WY, Zhu JQ. Evaluating the effectiveness of prophylactic central neck dissection with total thyroidectomy for cN0 papillary thyroid carcinoma: an updated meta-analysis. Eur J Surg Oncol. 2017; Nov. 43(11):1989–2000.
Article8. Ebina A, Sugitani I, Fujimoto Y, Yamada K. Risk-adapted management of papillary thyroid carcinoma according to our own risk group classification system: is thyroid lobectomy the treatment of choice for low-risk patients. Surgery. 2014; Dec. 156(6):1579–88.9. Liu J, Zhang Z, Huang H, Xu S, Liu Y, Liu S, et al. Total thyroidectomy versus lobectomy for intermediate-risk papillary thyroid carcinoma: a single-institution matched-pair analysis. Oral Oncol. 2019; Mar. 90:17–22.
Article10. Choi JB, Lee SG, Kim MJ, Kim TH, Ban EJ, Lee CR, et al. Oncologic outcomes in patients with 1-cm to 4-cm differentiated thyroid carcinoma according to extent of thyroidectomy. Head Neck. 2019; Jan. 41(1):56–63.
Article11. Hyun SM, Song HY, Kim SY, Nam SY, Roh JL, Han MW, et al. Impact of combined prophylactic unilateral central neck dissection and hemithyroidectomy in patients with papillary thyroid microcarcinoma. Ann Surg Oncol. 2012; Feb. 19(2):591–6.
Article12. Kuba S, Yamanouchi K, Hayashida N, Maeda S, Adachi T, Sakimura C, et al. Total thyroidectomy versus thyroid lobectomy for papillary thyroid cancer: comparative analysis after propensity score matching: a multicenter study. Int J Surg. 2017; Feb. 38:143–8.
Article13. Kwon H, Jeon MJ, Kim WG, Park S, Kim M, Song DE, et al. A comparison of lobectomy and total thyroidectomy in patients with papillary thyroid microcarcinoma: a retrospective individual risk factor-matched cohort study. Eur J Endocrinol. 2017; Apr. 176(4):371–8.
Article14. Lee CR, Son H, Lee S, Kang SW, Jeong JJ, Nam KH, et al. Lobectomy and prophylactic central neck dissection for papillary thyroid microcarcinoma: do involved lymph nodes mandate completion thyroidectomy. World J Surg. 2014; Apr. 38(4):872–7.
Article15. Li X, Zhao C, Hu D, Yu Y, Gao J, Zhao W, et al. Hemithyroidectomy increases the risk of disease recurrence in patients with ipsilateral multifocal papillary thyroid carcinoma. Oncol Lett. 2013; Apr. 5(4):1412–6.
Article16. Matsuzu K, Sugino K, Masudo K, Nagahama M, Kitagawa W, Shibuya H, et al. Thyroid lobectomy for papillary thyroid cancer: long-term follow-up study of 1,088 cases. World J Surg. 2014; Jan. 38(1):68–79.
Article17. Park YM, Lee DY, Oh KH, Cho JG, Baek SK, Kwon SY, et al. Clinical implications of pathologic factors after thyroid lobectomy in patients with papillary thyroid carcinoma. Oral Oncol. 2017; Dec. 75:1–5.
Article18. Park JH, Lee YM, Lee YH, Hong SJ, Yoon JH. The prognostic value of serum thyroid-stimulating hormone level post-lobectomy in low- and intermediate-risk papillary thyroid carcinoma. J Surg Oncol. 2018; Sep. 118(3):390–6.
Article19. Son HJ, Kim JK, Jung YD, Jang GH, Seo YT, Kim DS, et al. Comparison of outcomes between hemithyroidectomy alone and hemithyroidectomy with elective unilateral central neck dissection in patients with papillary thyroid microcarcinoma. Head Neck. 2018; Nov. 40(11):2449–54.
Article20. Song E, Han M, Oh HS, Kim WW, Jeon MJ, Lee YM, et al. Lobectomy is feasible for 1-4 cm papillary thyroid carcinomas: a 10-year propensity score matched-pair analysis on recurrence. Thyroid. 2019; Jan. 29(1):64–70.21. Vaisman F, Shaha A, Fish S, Michael Tuttle R. Initial therapy with either thyroid lobectomy or total thyroidectomy without radioactive iodine remnant ablation is associated with very low rates of structural disease recurrence in properly selected patients with differentiated thyroid cancer. Clin Endocrinol (Oxf). 2011; Jul. 75(1):112–9.
Article22. Vaisman F, Momesso D, Bulzico DA, Pessoa CH, da Cruz MD, Dias F, et al. Thyroid lobectomy is associated with excellent clinical outcomes in properly selected differentiated thyroid cancer patients with primary tumors greater than 1 cm. J Thyroid Res. 2013; 2013:398194.23. Xue S, Wang P, Liu J, Chen G. Total thyroidectomy may be more reasonable as initial surgery in unilateral multifocal papillary thyroid microcarcinoma: a single-center experience. World J Surg Oncol. 2017; Mar. 15(1):62.
Article24. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; Jan. 26(1):1–133.
Article25. Lang BH, Ng SH, Lau LL, Cowling BJ, Wong KP, Wan KY. A systematic review and meta-analysis of prophylactic central neck dissection on short-term locoregional recurrence in papillary thyroid carcinoma after total thyroidectomy. Thyroid. 2013; Sep. 23(9):1087–98.
Article26. Ito Y, Miyauchi A, Kihara M, Higashiyama T, Kobayashi K, Miya A. Patient age is significantly related to the progression of papillary microcarcinoma of the thyroid under observation. Thyroid. 2014; Jan. 24(1):27–34.
Article27. Sugitani I, Fujimoto Y, Yamada K. Association between serum thyrotropin concentration and growth of asymptomatic papillary thyroid microcarcinoma. World J Surg. 2014; Mar. 38(3):673–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Central Neck Dissection for Papillary Thyroid Carcinoma
- Surgical Treatment for Papillary Thyroid Carcinoma in Japan: Differences from Other Countries
- Locoregional Recurrence in Papillary Thyroid Carcinoma
- Regional Lymph Node Metastasis in Papillary Thyroid Cancer
- Concurrent Papillary and Medullary Carcinoma of the Thyroid Gland