Clin Endosc.
2019 Mar;52(2):107-113. 10.5946/ce.2018.189.
Advanced Treatment and Imaging in Colonoscopy: The Pocket-Creation Method for Complete Resection and Linked Color Imaging for Better Detection of Early Neoplastic Lesions by Colonoscopy
- Affiliations
-
- 1Division of Gastroenterology, Department of Medicine, Jichi Medical University, Shimotsuke, Japan. ireef@jichi.ac.jp
- 2Shinozaki Medical Clinic, Utsunomiya, Japan.
- 3Department of Surgery, Jichi Medical University, Shimotsuke, Japan.
- KMID: 2447666
- DOI: http://doi.org/10.5946/ce.2018.189
Abstract
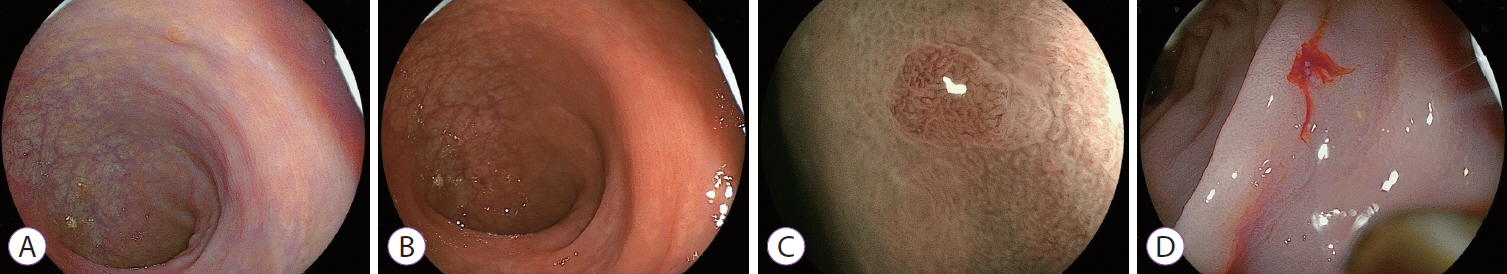
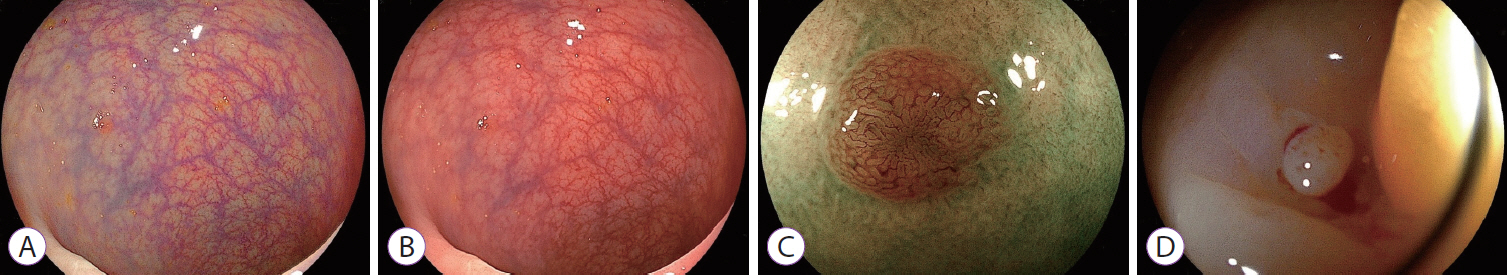
- Early detection and resection of neoplastic lesions are key objectives to diminish colorectal cancer mortality. Resection of superficial colorectal neoplasms, cold snare polypectomy, endoscopic mucosal resection, and endoscopic submucosal dissection have all been developed and used worldwide. The pocket-creation method facilitates the resection of tumors in difficult and routine locations. Early detection is the most important first step to maximize the benefits of recent advancements in endoscopic techniques. However, the detection of small, flat-shaped, or faded color lesions remains difficult. Linked color imaging, a novel multi-light technology, facilitates the recognition of minor differences in tissue by enhancing the color contrast between early colorectal neoplasms and surrounding normal mucosa in a bright field of view. The most striking feature of linked color imaging is its ability to display the color of early neoplastic lesions as distinct from inflammatory changes, both of which have similar "redness" when viewed using white light imaging. To increase the detection rate of neoplasms, linked color imaging should be used from the outset for endoscopic observation. Early detection of superficial colorectal tumors can result in decreased mortality from colorectal cancer and maintain a good quality of life for patients.
MeSH Terms
Figure
Reference
-
1. Tanaka S, Kashida H, Saito Y, et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015; 27:417–434.
Article2. Zauber AG, Winawer SJ, O’Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012; 366:687–696.
Article3. Watanabe T, Muro K, Ajioka Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol. 2018; 23:1–34.
Article4. Sakamoto H, Hayashi Y, Miura Y, et al. Pocket-creation method facilitates endoscopic submucosal dissection of colorectal laterally spreading tumors, non-granular type. Endosc Int Open. 2017; 5:E123–E129.
Article5. Miura Y, Shinozaki S, Hayashi Y, Sakamoto H, Lefor AK, Yamamoto H. Duodenal endoscopic submucosal dissection is feasible using the pocket-creation method. Endoscopy. 2017; 49:8–14.
Article6. Miura Y, Hayashi Y, Lefor AK, Osawa H, Yamamoto H. The pocket-creation method of ESD for gastric neoplasms. Gastrointest Endosc. 2016; 83:457–458.
Article7. Imaeda H, Hosoe N, Ida Y, et al. Novel technique of endoscopic submucosal dissection by using external forceps for early rectal cancer (with videos). Gastrointest Endosc. 2012; 75:1253–1257.
Article8. Suzuki S, Gotoda T, Kobayashi Y, et al. Usefulness of a traction method using dental floss and a hemoclip for gastric endoscopic submucosal dissection: a propensity score matching analysis (with videos). Gastrointest Endosc. 2016; 83:337–346.
Article9. Ritsuno H, Sakamoto N, Osada T, et al. Prospective clinical trial of traction device-assisted endoscopic submucosal dissection of large superficial colorectal tumors using the S-O clip. Surg Endosc. 2014; 28:3143–3149.
Article10. Yamamoto H, Kawata H, Sunada K, et al. Successful en-bloc resection of large superficial tumors in the stomach and colon using sodium hyaluronate and small-caliber-tip transparent hood. Endoscopy. 2003; 35:690–694.
Article11. Shinozaki S, Kobayashi Y, Hayashi Y, Sakamoto H, Lefor AK, Yamamoto H. Efficacy and safety of cold versus hot snare polypectomy for resecting small colorectal polyps: systematic review and meta-analysis. Dig Endosc. 2018; 30:592–599.
Article12. Shinozaki S, Hayashi Y, Lefor AK, Yamamoto H. What is the best therapeutic strategy for colonoscopy of colorectal neoplasia? Future perspectives from the East. Dig Endosc. 2016; 28:289–295.
Article13. Horiuchi A, Nakayama Y, Kajiyama M, Tanaka N, Sano K, Graham DY. Removal of small colorectal polyps in anticoagulated patients: a prospective randomized comparison of cold snare and conventional polypectomy. Gastrointest Endosc. 2014; 79:417–423.14. Okada M, Sakamoto H, Takezawa T, et al. Laterally spreading tumor of the rectum delineated with linked color imaging technology. Clin Endosc. 2016; 49:207–208.
Article15. Fukuda H, Miura Y, Osawa H, et al. Linked color imaging can enhance recognition of early gastric cancer by high color contrast to surrounding gastric intestinal metaplasia. J Gastroenterol. 2018; Oct. 5. [Epub]. https://doi.org/10.1007/s00535-018-1515-6.
Article16. Heresbach D, Barrioz T, Lapalus MG, et al. Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy. 2008; 40:284–290.
Article17. Leufkens AM, van Oijen MG, Vleggaar FP, Siersema PD. Factors influencing the miss rate of polyps in a back-to-back colonoscopy study. Endoscopy. 2012; 44:470–475.
Article18. Singh H, Nugent Z, Demers AA, Kliewer EV, Mahmud SM, Bernstein CN. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology. 2010; 139:1128–1137.
Article19. Matsushita M, Hajiro K, Okazaki K, Takakuwa H, Tominaga M. Efficacy of total colonoscopy with a transparent cap in comparison with colonoscopy without the cap. Endoscopy. 1998; 30:444–447.
Article20. Halpern Z, Gross SA, Gralnek IM, et al. Comparison of adenoma detection and miss rates between a novel balloon colonoscope and standard colonoscopy: a randomized tandem study. Endoscopy. 2015; 47:238–244.
Article21. Gralnek IM, Siersema PD, Halpern Z, et al. Standard forward-viewing colonoscopy versus full-spectrum endoscopy: an international, multicentre, randomised, tandem colonoscopy trial. Lancet Oncol. 2014; 15:353–360.
Article22. Leufkens AM, DeMarco DC, Rastogi A, et al. Effect of a retrograde-viewing device on adenoma detection rate during colonoscopy: the TERRACE study. Gastrointest Endosc. 2011; 73:480–489.
Article23. Kaminski MF, Hassan C, Bisschops R, et al. Advanced imaging for detection and differentiation of colorectal neoplasia: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2014; 46:435–449.
Article24. Fujimoto D, Muguruma N, Okamoto K, et al. Linked color imaging enhances endoscopic detection of sessile serrated adenoma/polyps. Endosc Int Open. 2018; 6:E322–E334.
Article25. Goda Y, Mori H, Kobara H, et al. Therapeutic application of linked color imaging for colorectal endoscopic mucosal resection. Endoscopy. 2018; 50:E8–E9.
Article26. Min M, Deng P, Zhang W, Sun X, Liu Y, Nong B. Comparison of linked color imaging and white-light colonoscopy for detection of colorectal polyps: a multicenter, randomized, crossover trial. Gastrointest Endosc. 2017; 86:724–730.
Article27. Suzuki T, Hara T, Kitagawa Y, et al. Linked-color imaging improves endoscopic visibility of colorectal nongranular flat lesions. Gastrointest Endosc. 2017; 86:692–697.
Article28. Yoshida N, Naito Y, Murakami T, et al. Linked color imaging improves the visibility of colorectal polyps: a video study. Endosc Int Open. 2017; 5:E518–E525.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Applications of Linked Color Imaging and Blue Laser/Light Imaging in the Screening, Diagnosis, and Treatment of Superficial Colorectal Tumors
- The impact of linked color imaging on adenoma detection rate in colonoscopy: a systematic review and meta-analysis
- Detecting colorectal lesions with image-enhanced endoscopy: an updated review from clinical trials
- Endoscopic Diagnosis of Colorectal Neoplasms Using Autofluorescence Imaging
- Colorectal Cancer after Colonoscopy: Causes and Prevention Strategies