Dement Neurocogn Disord.
2015 Jun;14(2):87-93. 10.12779/dnd.2015.14.2.87.
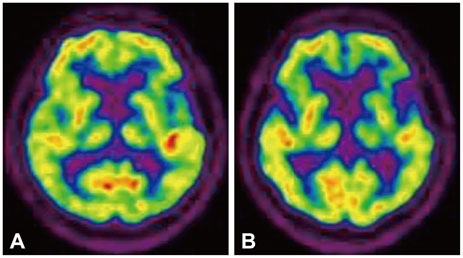
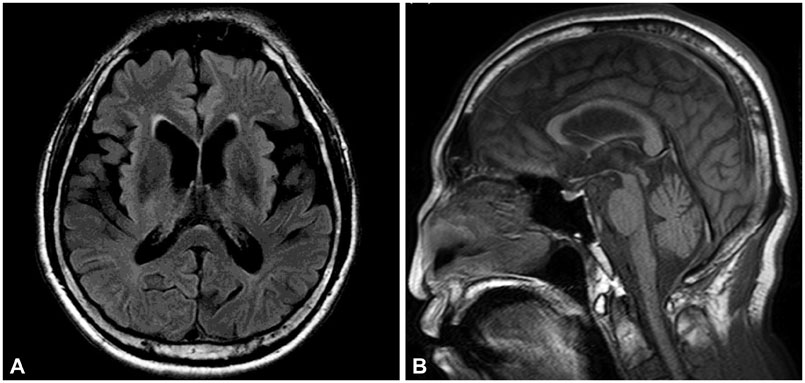
Longitudinal Clinical Changes of Non-Fluent/Agrammatic Primary Progressive Aphasia as Tau Spectrum Disorder: A Case Report
- Affiliations
-
- 1Department of Neurology, Kangwon National University Hospital, Chuncheon, Korea.
- 2Clinical Neuroscience Center, Seoul National University Bundang Hospital, Department of Neurology, Seoul National University College of Medicine, Seongnam, Korea. neuroksy@snu.ac.kr
- KMID: 2443007
- DOI: http://doi.org/10.12779/dnd.2015.14.2.87
Abstract
- BACKGROUND
Tauopathies are a group of diseases caused by the accumulation of hyperphosphorylated tau protein in the central nervous system. Previous studies have revealed that there is considerable overlap in clinical, pathological, and genetic features among different taupathies.
CASE REPORT
We report a patient with non-fluent/agrammatic primary progressive aphasia at the initial assessment. Over time, other symptoms belonging to corticobasal degeneration and progressive supranuclear palsy appeared in this patient.
CONCLUSIONS
Clinical overlapping features in these disorders may represent different phenotypes of a single disease process.
Keyword
MeSH Terms
Figure
Reference
-
1. Seelaar H, Rohrer JD, Pijnenburg YA, Fox NC, van Swieten JC. Clinical, genetic and pathological heterogeneity of frontotemporal dementia: a review. J Neurol Neurosurg Psychiatry. 2011; 82:476–486.
Article2. Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011; 76:1006–1014.
Article3. Grossman M. The non-fluent/agrammatic variant of primary progressive aphasia. Lancet Neurol. 2012; 11:545–555.
Article4. Gorno-Tempini ML, Murray RC, Rankin KP, Weiner MW, Miller BL. Clinical, cognitive and anatomical evolution from nonfluent progressive aphasia to corticobasal syndrome: a case report. Neurocase. 2004; 10:426–436.
Article5. Kim HJ, Baik YJ, Jeong JH. A case of progressive supranuclear palsy with progressive non-fluent aphasia. Dement Neurocognitive Disord. 2007; 6:77–80.6. Raggi A, Marcone A, Iannaccone S, Ginex V, Perani D, Cappa SF. The clinical overlap between the corticobasal degeneration syndrome and other diseases of the frontotemporal spectrum: three case reports. Behav Neurol. 2007; 18:159–164.
Article7. Kertesz A, McMonagle P, Jesso S. Extrapyramidal syndromes in frontotemporal degeneration. J Mol Neurosci. 2011; 45:336–342.
Article8. Kertesz A, Poole E. The aphasia quotient: the taxonomic approach to measurement of aphasic disability. 1974. Can J Neurol Sci. 2004; 31:175–184.
Article9. Robert M, Mathuranath PS. Tau and tauopathies. Neurol India. 2007; 55:11–16.
Article10. Bouchard M, Suchowersky O. Tauopathies: one disease or many? Can J Neurol Sci. 2011; 38:547–556.
Article11. Spillantini MG, Goedert M. Tau pathology and neurodegeneration. Lancet Neurol. 2013; 12:609–622.
Article12. Kertesz A, McMonagle P, Blair M, Davidson W, Munoz DG. The evolution and pathology of frontotemporal dementia. Brain. 2005; 128(Pt 9):1996–2005.
Article13. Josephs KA, Petersen RC, Knopman DS, Boeve BF, Whitwell JL, Duffy JR, et al. Clinicopathologic analysis of frontotemporal and corticobasal degenerations and PSP. Neurology. 2006; 66:41–48.
Article14. Mathew R, Bak TH, Hodges JR. Diagnostic criteria for corticobasal syndrome: a comparative study. J Neurol Neurosurg Psychiatry. 2012; 83:405–410.
Article15. Williams DR, Lees AJ. Progressive supranuclear palsy: clinicopathological concepts and diagnostic challenges. Lancet Neurol. 2009; 8:270–279.
Article16. Yoshida M. Astrocytic inclusions in progressive supranuclear palsy and corticobasal degeneration. Neuropathology. 2014; 34:555–570.
Article17. Armstrong MJ, Litvan I, Lang AE, Bak TH, Bhatia KP, Borroni B, et al. Criteria for the diagnosis of corticobasal degeneration. Neurology. 2013; 80:496–503.
Article18. Litvan I, Agid Y, Calne D, Campbell G, Dubois B, Duvoisin RC, et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDSSPSP international workshop. Neurology. 1996; 47:1–9.
Article19. Mimura M, Oda T, Tsuchiya K, Kato M, Ikeda K, Hori K, et al. Corticobasal degeneration presenting with nonfluent primary progressive aphasia: a clinicopathological study. J Neurol Sci. 2001; 183:19–26.
Article20. Mochizuki A, Ueda Y, Komatsuzaki Y, Tsuchiya K, Arai T, Shoji S. Progressive supranuclear palsy presenting with primary progressive aphasia--clinicopathological report of an autopsy case. Acta Neuropathol. 2003; 105:610–614.
Article21. Sánchez-Valle R, Forman MS, Miller BL, Gorno-Tempini ML. From progressive nonfluent aphasia to corticobasal syndrome: a case report of corticobasal degeneration. Neurocase. 2006; 12:355–359.
Article22. Karnik NS, D'Apuzzo M, Greicius M. Non-fluent progressive aphasia, depression, and OCD in a woman with progressive supranuclear palsy: neuroanatomical and neuropathological correlations. Neurocase. 2006; 12:332–338.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corticobasal Degeneration Presenting as Non-Fluent/Agrammatic Primary Progressive Aphasia: A Case Report
- A Case of the Fluent Form of Primary Progressive Aphasia Presenting as Conduction Aphasia
- ¹â¸F-THK5351 PET Imaging in Nonfluent-Agrammatic Variant Primary Progressive Aphasia
- Logopenic Progressive Aphasia Revealing Positive Cerebrospinal Fluid Biomarkers for Alzheimer's Disease
- Role of Positron Emission Tomography as a Biologic Marker in the Diagnosis of Primary Progressive Aphasia: Two Case Reports