Dement Neurocogn Disord.
2016 Jun;15(2):55-58. 10.12779/dnd.2016.15.2.55.
Corticobasal Degeneration Presenting as Non-Fluent/Agrammatic Primary Progressive Aphasia: A Case Report
- Affiliations
-
- 1Department of Neurology, Cognitive Disorders and Dementia Center, College of Medicine, Dong-A University, Busan, Korea. neuropark@dau.ac.kr
- KMID: 2442857
- DOI: http://doi.org/10.12779/dnd.2016.15.2.55
Abstract
- BACKGROUND
Non-fluent agrammatic primary progressive aphasia (naPPA) is characterized by progressive non-fluent speech disorder and might be associated with taupathy such as corticobasal degeneration (CBD) and progressive supranuclear palsy. We report a case of overlap syndrome presented with language impairment, and diagnosed as naPPA with possible CBD.
CASE REPORT
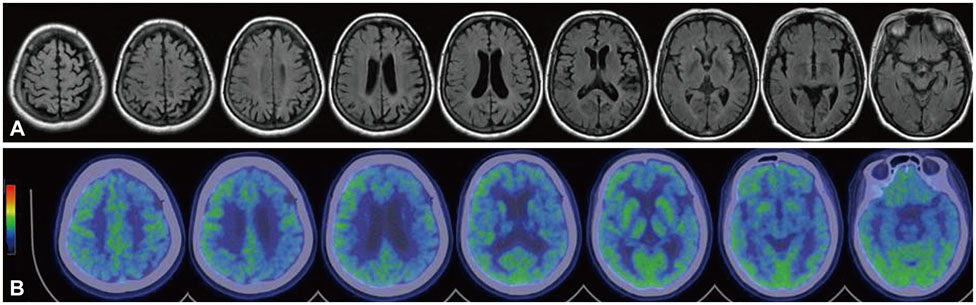
A 58-year-old woman visited a memory and dementia clinic, with a 10-month history of progressive language disturbance. She was diagnosed as naPPA and overlapping CBD, based on the clinical features and neuroimaging findings including florbetaben PET.
CONCLUSIONS
naPPA is pathologically caused by taupathy, and might progress to asymmetrical parkinsonism and apraxia, suggestive of CBD. Overlapping clinical features in our case represent various phenotypes of taupathy.
MeSH Terms
Figure
Reference
-
1. Hardiman O, Doherty CP. Neurodegenerative Disorders. London: Springer;2011. p. 115–117.
Article2. Grossman M. The non-fluent/agrammatic variant of primary progressive aphasia. Lancet Neurol. 2012; 11:545–555.
Article3. Mesulam MM. Slowly progressive aphasia without generalized dementia. Ann Neurol. 1982; 11:592–598.
Article4. Kertesz A, Hudson L, Mackenzie IR, Munoz DG. The pathology and nosology of primary progressive aphasia. Neurology. 1994; 44:2065–2072.
Article5. Grimes DA, Lang AE, Bergeron CB. Dementia as the most common presentation of cortical-basal ganglionic degeneration. Neurology. 1999; 53:1969–1974.
Article6. Gorno-Tempini ML, Murray RC, Rankin KP, Weiner MW, Miller BL. Clinical, cognitive and anatomical evolution from nonfluent progressive aphasia to corticobasal syndrome: a case report. Neurocase. 2004; 10:426–436.
Article7. Boeve B, Dickson D, Duffy J, Bartleson J, Trenerry M, Petersen R. Progressive nonfluent aphasia and subsequent aphasic dementia associated with atypical progressive supranuclear palsy pathology. Eur Neurol. 2003; 49:72–78.
Article8. Boeve BF. Parkinson-related dementias. Neurol Clin. 2007; 25:761–781. vii
Article9. Wenning GK, Litvan I, Jankovic J, Granata R, Mangone CA, McKee A, et al. Natural history and survival of 14 patients with corticobasal degeneration confirmed at postmortem examination. J Neurol Neurosurg Psychiatry. 1998; 64:184–189.
Article10. Armstrong MJ, Litvan I, Lang AE, Bak TH, Bhatia KP, Borroni B, et al. Criteria for the diagnosis of corticobasal degeneration. Neurology. 2013; 80:496–503.
Article11. Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011; 76:1006–1014.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Longitudinal Clinical Changes of Non-Fluent/Agrammatic Primary Progressive Aphasia as Tau Spectrum Disorder: A Case Report
- A Case of the Fluent Form of Primary Progressive Aphasia Presenting as Conduction Aphasia
- Progressive Nonfluent Aphasia With Ideomotor Apraxia and Rigidity in the Right Upper Extremity
- A Case of Idiopathic Parkinson's Disease Combined with Progressive Nonfluent Aphasia
- Primary Progressive Aphasia and the Left Hemisphere Language Network