Ann Rehabil Med.
2018 Apr;42(2):204-212. 10.5535/arm.2018.42.2.204.
Characteristics of Cricopharyngeal Dysphagia After Ischemic Stroke
- Affiliations
-
- 1Department of Rehabilitation Medicine, Nowon Eulji Medical Center, Eulji University, Seoul, Korea. khj2603@eulji.ac.kr
- KMID: 2432190
- DOI: http://doi.org/10.5535/arm.2018.42.2.204
Abstract
OBJECTIVE
To evaluate the characteristics of cricopharyngeal dysfunction (CPD), the frequency, and correlation with a brain lesion in patients with first-ever ischemic stroke, and to provide basic data for developing a therapeutic protocol for dysphagia management.
METHODS
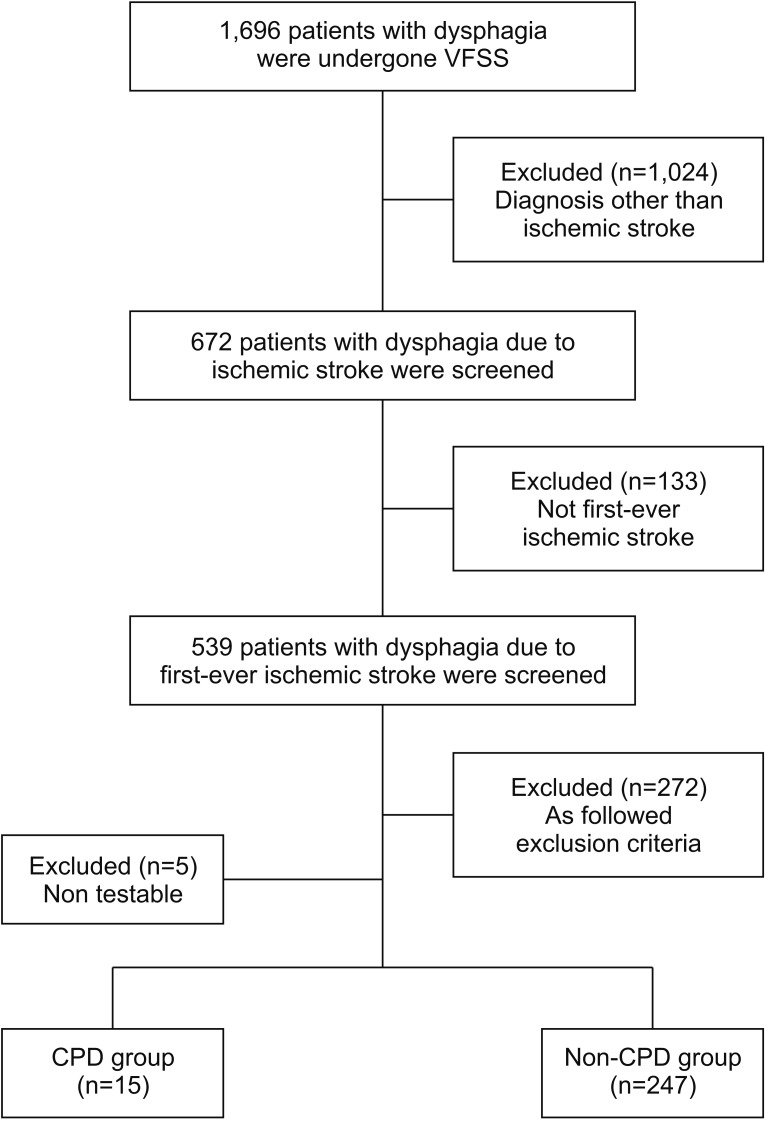
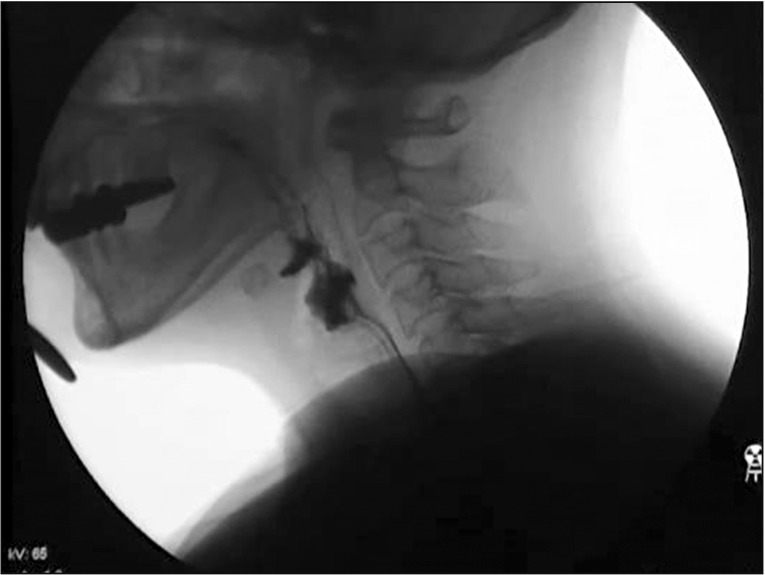
We retrospectively reviewed the medical records of a series of subjects post-stroke who underwent a videofluoroscopic swallowing study (VFSS) from January 2009 to December 2015. VFSS images were recorded on videotape and analyzed. CPD was defined as the retention of more than 25% of residue in the pyriform sinus after swallowing. The location of the brain lesion was assessed using magnetic resonance imaging.
RESULTS
Among the 262 dysphagic patients with first-ever ischemic stroke, 15 (5.7%) showed CPD on the VFSS. Patients with an infratentorial lesion had a significantly higher proportion of CPD than those with a supratentorial lesion (p=0.003), and lateral medullary infarction was identified as the single independent predictor of CPD (multivariable analysis: odds ratio=19.417; confidence interval, 5.560-67.804; p < 0.0001). Compared to patients without CPD, those with CPD had a significantly prolonged pharyngeal transit time, lower laryngeal elevation, and a higher pharyngeal constriction ratio and functional dysphagia scale score.
CONCLUSION
Overall, the results support the notion that an impaired upper esopharyngeal opening is likely related to the specific locations of brain lesions. The association of CPD with lateral medullary infarction can be explained based on the regulation of the pharyngolaryngeal motor system by the motor neurons present in the dorsal nucleus ambiguus. Overall, the results reveal the relation between CPD and the problems in the pharyngeal phase as well as the severity of dysphagia.
Keyword
MeSH Terms
Figure
Reference
-
1. Gonzalez-Fernandez M, Daniels SK. Dysphagia in stroke and neurologic disease. Phys Med Rehabil Clin N Am. 2008; 19:867–888. PMID: 18940646.2. Baredes S, Shah CS, Kaufman R. The frequency of cricopharyngeal dysfunction on videofluoroscopic swallowing studies in patients with dysphagia. Am J Otolaryngol. 1997; 18:185–189. PMID: 9164621.
Article3. Lang IM. Brain stem control of the phases of swallowing. Dysphagia. 2009; 24:333–348. PMID: 19399555.
Article4. Dou Z, Zu Y, Wen H, Wan G, Jiang L, Hu Y. The effect of different catheter balloon dilatation modes on cricopharyngeal dysfunction in patients with dysphagia. Dysphagia. 2012; 27:514–520. PMID: 22427310.
Article5. Kocdor P, Siegel ER, Tulunay-Ugur OE. Cricopharyngeal dysfunction: a systematic review comparing outcomes of dilatation, botulinum toxin injection, and myotomy. Laryngoscope. 2016; 126:135–141. PMID: 26360122.
Article6. Wan P, Chen X, Zhu L, Xu S, Huang L, Li X, et al. Dysphagia post subcortical and supratentorial stroke. J Stroke Cerebrovasc Dis. 2016; 25:74–82. PMID: 26508684.
Article7. Fager SK, Hakel M, Brady S, Barlow SM, Nordness A, Delgado A, et al. Adult neurogenic communication and swallowing disorders. In : Cifu DX, editor. Braddom's physical medicine and rehabilitation. 5th ed. Philadelphia: Elsevier;2016. p. 53–69.8. Logemann JA. Evaluation and treatment of swallowing disorders. Austin: Pro-Ed;1995.9. Kuhn MA, Belafsky PC. Management of cricopharyngeus muscle dysfunction. Otolaryngol Clin North Am. 2013; 46:1087–1099. PMID: 24262961.
Article10. Lee SY, Seo HG, Paik NJ. Botulinum toxin injection for dysphagia: a blinded retrospective videofluoroscopic swallowing study analysis. Am J Phys Med Rehabil. 2009; 88:491–494. PMID: 19325455.11. Kahrilas PJ, Logemann JA, Lin S, Ergun GA. Pharyngeal clearance during swallowing: a combined manometric and videofluoroscopic study. Gastroenterology. 1992; 103:128–136. PMID: 1612322.
Article12. Shaker R, Easterling C, Kern M, Nitschke T, Massey B, Daniels S, et al. Rehabilitation of swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroenterology. 2002; 122:1314–1321. PMID: 11984518.
Article13. Robbins J, Kays SA, Gangnon RE, Hind JA, Hewitt AL, Gentry LR, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007; 88:150–158. PMID: 17270511.
Article14. Steele CM, Huckabee ML. The influence of orolingual pressure on the timing of pharyngeal pressure events. Dysphagia. 2007; 22:30–36. PMID: 17024546.
Article15. Lee CK, Kim JA. Pattern of post-stroke swallowing disorder according to the brain lesion. J Korean Acad Rehabil Med. 2001; 25:193–201.16. Bian RX, Choi IS, Kim JH, Han JY, Lee SG. Impaired opening of the upper esophageal sphincter in patients with medullary infarctions. Dysphagia. 2009; 24:238–245. PMID: 18791766.
Article17. Steinhagen V, Grossmann A, Benecke R, Walter U. Swallowing disturbance pattern relates to brain lesion location in acute stroke patients. Stroke. 2009; 40:1903–1906. PMID: 19286597.
Article18. Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001; 82:677–682. PMID: 11346847.
Article19. Rademaker AW, Pauloski BR, Logemann JA, Shanahan TK. Oropharyngeal swallow efficiency as a representative measure of swallowing function. J Speech Hear Res. 1994; 37:314–325. PMID: 8028312.
Article20. Leonard RJ, Kendall KA, McKenzie S, Goncalves MI, Walker A. Structural displacements in normal swallowing: a videofluoroscopic study. Dysphagia. 2000; 15:146–152. PMID: 10839828.
Article21. Alfonsi E, Versino M, Merlo IM, Pacchetti C, Martignoni E, Bertino G, et al. Electrophysiologic patterns of oral-pharyngeal swallowing in parkinsonian syndromes. Neurology. 2007; 68:583–589. PMID: 17310027.
Article22. Ali GN, Wallace KL, Schwartz R, DeCarle DJ, Zagami AS, Cook IJ. Mechanisms of oral-pharyngeal dysphagia in patients with Parkinson’s disease. Gastroenterology. 1996; 110:383–392. PMID: 8566584.
Article23. Mu L, Sobotka S, Chen J, Su H, Sanders I, Adler CH, et al. Altered pharyngeal muscles in Parkinson disease. J Neuropathol Exp Neurol. 2012; 71:520–530. PMID: 22588389.
Article24. Ertekin C, Aydogdu I, Yuceyar N, Kiylioglu N, Tarlaci S, Uludag B. Pathophysiological mechanisms of oropharyngeal dysphagia in amyotrophic lateral sclerosis. Brain. 2000; 123(Pt 1):125–140. PMID: 10611127.
Article25. Martin RE, Sessle BJ. The role of the cerebral cortex in swallowing. Dysphagia. 1993; 8:195–202. PMID: 8359039.
Article26. Ertekin C, Turman B, Tarlaci S, Celik M, Aydogdu I, Secil Y, et al. Cricopharyngeal sphincter muscle responses to transcranial magnetic stimulation in normal subjects and in patients with dysphagia. Clin Neurophysiol. 2001; 112:86–94. PMID: 11137665.
Article27. Valdez DT, Salapatek A, Niznik G, Linden RD, Diamant NE. Swallowing and upper esophageal sphincter contraction with transcranial magnetic-induced electrical stimulation. Am J Physiol. 1993; 264(2 Pt 1):G213–G219. PMID: 8447403.
Article28. Kahrilas PJ, Dodds WJ, Dent J, Logemann JA, Shaker R. Upper esophageal sphincter function during deglutition. Gastroenterology. 1988; 95:52–62. PMID: 3371625.
Article29. Ertekin C, Aydogdu I, Tarlaci S, Turman AB, Kiylioglu N. Mechanisms of dysphagia in suprabulbar palsy with lacunar infarct. Stroke. 2000; 31:1370–1376. PMID: 10835459.
Article30. Perlman AL, Palmer PM, McCulloch TM, Vandaele DJ. Electromyographic activity from human laryngeal, pharyngeal, and submental muscles during swallowing. J Appl Physiol (1985). 1999; 86:1663–1669. PMID: 10233133.31. Venker-van Haagen AJ, Hartman W, van den Brom WE, Wolvekamp WT. Continuous electromyographic recordings of pharyngeal muscle activity in normal and previously denervated muscles in dogs. Am J Vet Res. 1989; 50:1725–1728. PMID: 2802303.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of Criopharyngeal Dysphagia and Zenker’s Diverticulum
- Interventional Management of Post-stroke Dysphagia
- Update on Cricopharyngeal Dysphagia
- A Case of Cricopharyngeal Dyskinesia
- Isolated Dysphagia Caused by Failure of Cricopharyngeal Muscle Relaxation after Left Lateral Medullary Lacunar Infarction: A case report