Ann Lab Med.
2017 Nov;37(6):484-493. 10.3343/alm.2017.37.6.484.
Benefits of Thromboelastography and Thrombin Generation Assay for Bleeding Prediction in Patients With Thrombocytopenia or Hematologic Malignancies
- Affiliations
-
- 1Department of Laboratory Medicine, Seoul National University College of Medicine, Seoul, Korea. lukekhk@snu.ac.kr
- 2Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. kim_dajung@hanmail.net
- KMID: 2425988
- DOI: http://doi.org/10.3343/alm.2017.37.6.484
Abstract
- BACKGROUND
Thromboelastography (TEG) provides comprehensive information on the whole blood clot formation phases, whereas thrombin generation assay (TGA) reveals the endogenous thrombin levels in plasma. We investigated the potential significance of TEG and TGA parameters for prediction of clinical bleeding in hematologic patients on the basis of the patient's platelet levels.
METHODS
TEG and TGA were performed in 126 patients with thrombocytopenia or hematologic malignancies. The bleeding tendencies were stratified on the basis of the World Health Organization bleeding grade.
RESULTS
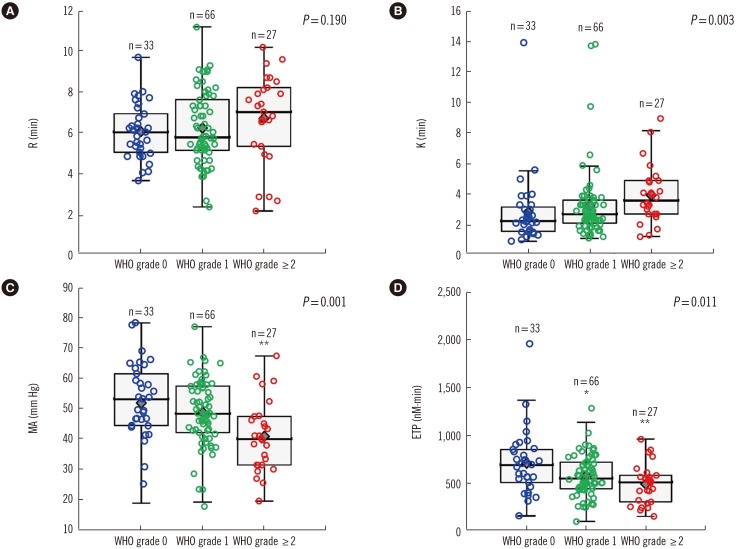
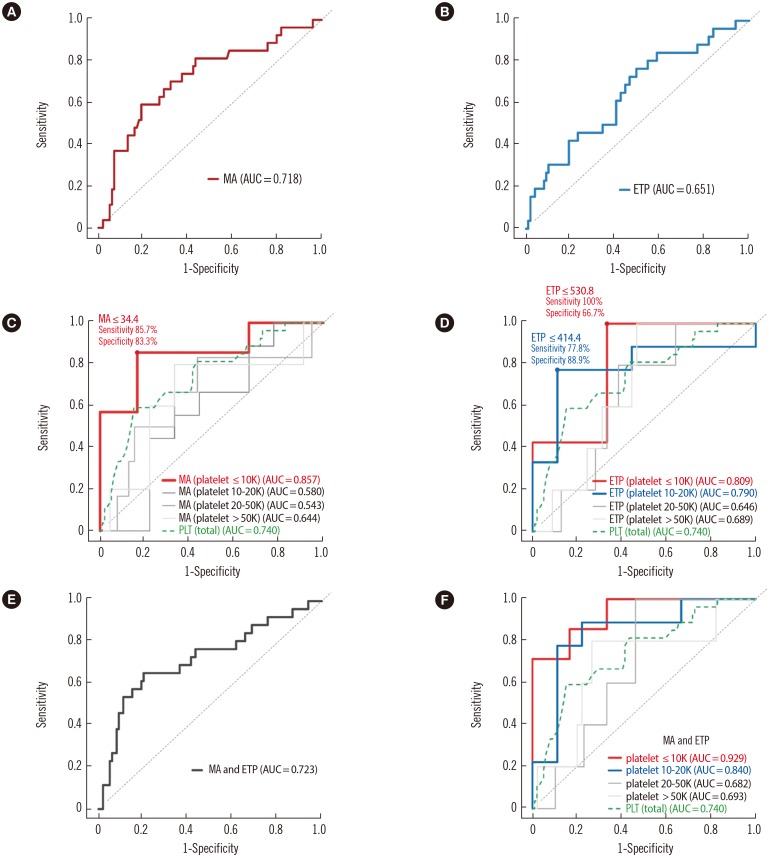
Maximum amplitude (MA) and clot formation in TEG and endogenous thrombin potential (ETP) in TGA showed significant associations with high bleeding grades (P=0.001 and P=0.011, respectively). In patients with platelet counts ≤10×10â¹/L, low MA values were strongly associated with a high bleeding risk. For bleeding prediction, the area under the curve (AUC) of MA (0.857) and ETP (0.809) in patients with severe thrombocytopenia tended to be higher than that of platelets (0.740) in all patients. Patients with platelet counts ≤10×10â¹/L displayed the highest AUC of the combined MA and ETP (0.929).
CONCLUSIONS
Both TEG and TGA were considered to be good predictors of clinical bleeding in patients with severe thrombocytopenia. Combination of the ETP and MA values resulted in a more sensitive bleeding risk prediction in those with severe thrombocytopenia.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Prediction of Mid-term Platelet Transfusion in Stable Trauma Patients Using Rotational Thromboelastometry
Ha Jin Lim, Hyunseok Jang, Naa Lee, Euisung Jeong, Yunchul Park, Younggoun Jo, Jungchul Kim, Young Eun Lee, Hyun-Jung Choi, Seung-Jung Kee, Jong Hee Shin, Myung Geun Shin
Ann Lab Med. 2024;44(1):74-81. doi: 10.3343/alm.2024.44.1.74.
Reference
-
1. DeLoughery TG. Management of acquired bleeding problems in cancer patients. Hematol Oncol Clin North Am. 2010; 24:603–624. PMID: 20488357.2. Provan D, Stasi R, Newland AC, Blanchette VS, Bolton-Maggs P, Bussel JB, et al. International consensus report on the investigation and management of primary immune thrombocytopenia. Blood. 2010; 115:168–186. PMID: 19846889.3. Estcourt LJ, Stanworth SJ, Harrison P, Powter G, McClure M, Murphy MF, et al. Prospective observational cohort study of the association between thromboelastometry, coagulation and platelet parameters and bleeding in patients with haematological malignancies-the ATHENA study. Br J Haematol. 2014; 166:581–591. PMID: 24797282.4. Slichter SJ. Relationship between platelet count and bleeding risk in thrombocytopenic patients. Transfus Med Rev. 2004; 18:153–167. PMID: 15248165.5. Neunert C, Lim W, Crowther M, Cohen A, Solberg L Jr, Crowther MA. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011; 117:4190–4207. PMID: 21325604.6. Greene LA, Chen S, Seery C, Imahiyerobo AM, Bussel JB. Beyond the platelet count: immature platelet fraction and thromboelastometry correlate with bleeding in patients with immune thrombocytopenia. Br J Haematol. 2014; 166:592–600. PMID: 24797389.7. Zia AN, Chitlur M, Rajpurkar M, Ozgonenel B, Lusher J, Callaghan JH, et al. Thromboelastography identifies children with rare bleeding disorders and predicts bleeding phenotype. Haemophilia. 2015; 21:124–132. PMID: 25545302.8. Gunduz E, Akay OM, Bal C, Gulbas Z. Can thrombelastography be a new tool to assess bleeding risk in patients with idiopathic thrombocytopenic purpura? Platelets. 2011; 22:516–520. PMID: 21557684.9. Tran HT, Tjønnfjord GE, Holme PA. Use of thromboelastography and thrombin generation assay to predict clinical phenotype in patients with severe FVII deficiency. Haemophilia. 2014; 20:141–146. PMID: 23992369.10. Green D. Management of bleeding complications of hematologic malignancies. Semin Thromb Hemost. 2007; 33:427–434. PMID: 17525900.11. Kitchens CS. To bleed or not to bleed? Is that the question for the PTT? J Thromb Haemost. 2005; 3:2607–2611. PMID: 16150051.12. Al Dieri R, Peyvandi F, Santagostino E, Giansily M, Mannucci PM, Schved JF, et al. The thrombogram in rare inherited coagulation disorders: its relation to clinical bleeding. Thromb Haemost. 2002; 88:576–582. PMID: 12362226.13. Dargaud Y, Béguin S, Lienhart A, Al Dieri R, Trzeciak C, Bordet JC, et al. Evaluation of thrombin generating capacity in plasma from patients with haemophilia A and B. Thromb Haemost. 2005; 93:475–480. PMID: 15735797.14. Kim SY, Kim JE, Kim HK, Kim I, Yoon SS, Park S. Influence of coagulation and anticoagulant factors on global coagulation assays in healthy adults. Am J Clin Pathol. 2013; 139:370–379. PMID: 23429374.15. Josephson CD, Granger S, Assmann SF, Castillejo MI, Strauss RG, Slichter SJ, et al. Bleeding risks are higher in children versus adults given prophylactic platelet transfusions for treatment-induced hypoproliferative thrombocytopenia. Blood. 2012; 120:748–760. PMID: 22538854.16. Hemker HC, Giesen P, Al Dieri R, Regnault V, de Smedt E, Wagenvoord R, et al. Calibrated automated thrombin generation measurement in clotting plasma. Pathophysiol Haemost Thromb. 2003; 33:4–15. PMID: 12853707.17. Hanley JA, McNeil BJ. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 1983; 148:839–843. PMID: 6878708.18. Hollý P, Lisá L, Plameňová I, Dobrotová M, Kubisz P. Recombinant activated factor VII as an additional agent in the management of bleeding in patients with chemotherapy-induced thrombocytopenia. Blood Transfus. 2013; 11:466–468. PMID: 23245723.19. Gerotziafas GT, Chakroun T, Depasse F, Arzoglou P, Samama MM, Elalamy I. The role of platelets and recombinant factor VIIa on thrombin generation, platelet activation and clot formation. Thromb Haemost. 2004; 91:977–985. PMID: 15116259.20. Nielsen VG, Cohen BM, Cohen E. Effects of coagulation factor deficiency on plasma coagulation kinetics determined via thrombelastography: critical roles of fibrinogen and factors II, VII, X and XII. Acta Anaesthesiol Scand. 2005; 49:222–231. PMID: 15715625.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Experience of Coagulation Management in Multiple Myeloma Patient with Thrombocytopenia Using Thromboelastography: A case report
- Influence of Blood Coagulation Factors on Thromboelastographic Parameters in Healthy Adults
- RUNX1 Germline Mutation in a Patient with Chronic Thrombocytopenia
- The Management of Heparin-induced Thrombocytopenia with Thrombosis after Open Heart Surgery: A Case Report
- Prediction and prevention of post-procedural bleedings in patients with cirrhosis