Pediatr Gastroenterol Hepatol Nutr.
2018 Oct;21(4):234-247. 10.5223/pghn.2018.21.4.234.
Nutritional Support Strategies for the Preterm Infant in the Neonatal Intensive Care Unit
- Affiliations
-
- 1Department of Pediatrics, University of Colorado School of Medicine, Aurora, CO, United States. bill.hay@ucdenver.edu
- KMID: 2421985
- DOI: http://doi.org/10.5223/pghn.2018.21.4.234
Abstract
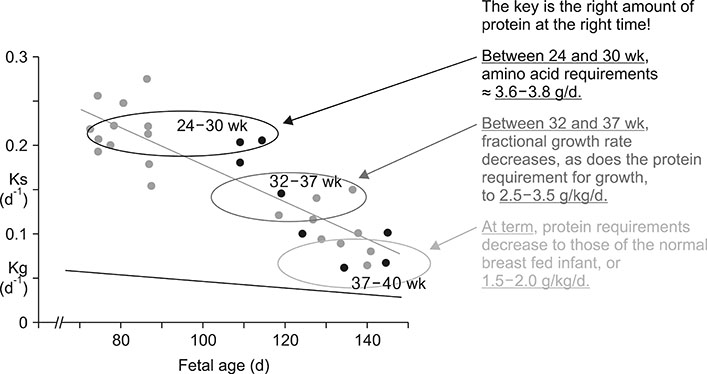
- The goal of nutrition of the preterm infant is to "provide nutrients to approximate the rate of growth and composition of weight gain for a normal fetus of the same postmenstrual age and to maintain normal concentrations of blood and tissue nutrients" (American Academy of Pediatrics 2014). Failure to provide the necessary amounts of all of the essential nutrients to preterm infants has produced not only growth failure, but also increased morbidity and less than optimal neurodevelopment. This continues to be true despite many efforts to increase nutrition of the preterm infants. In contrast, enhanced nutrition of very preterm infants, both intravenous and enteral, beginning right after birth, promotes positive energy and protein balance and improves longer term neurodevelopmental outcomes. The benefits are long lasting too, particularly for prevention of later life chronic diseases.
Keyword
MeSH Terms
Figure
Reference
-
1. Kleinman RE, Greer FR. American Academy of Pediatrics. Pediatric Nutrition. 7th ed. Elk Grove Village, IL: American Academy of Pediatrics;2014.2. Bouyssi-Kobar M, du Plessis AJ, McCarter R, Brossard-Racine M, Murnick J, Tinkleman L, et al. Third trimester brain growth in preterm infants compared with in utero healthy fetuses. Pediatrics. 2016; 138:e20161640.
Article3. Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006; 117:1253–1261.
Article4. Horbar JD, Ehrenkranz RA, Badger GJ, Edwards EM, Morrow KA, Soll RF, et al. Weight growth velocity and postnatal growth failure in infants 501 to 1500 grams:2000-2013. Pediatrics. 2015; 136:e84–e92.5. Dinerstein A, Nieto RM, Solana CL, Perez GP, Otheguy LE, Larguia AM. Early and aggressive nutritional strategy (parenteral and enteral) decreases postnatal growth failure in very low birth weight infants. J Perinatol. 2006; 26:436–442.
Article6. Stephens BE, Walden RV, Gargus RA, Tucker R, McKinley L, Mance M, et al. First-week protein and energy intakes are associated with 18-month developmental outcomes in extremely low birth weight infants. Pediatrics. 2009; 123:1337–1343.
Article7. Binenbaum G, Bell EF, Donohue P, Quinn G, Shaffer J, Tomlinson LA, et al. G-ROP Study Group. Development of modified screening criteria for retinopathy of prematurity: primary results from the postnatal growth and retinopathy of prematurity study. JAMA Ophthalmol. 2018; 136:1034–1040.
Article8. Matinolli HM, Hovi P, Männistö S, Sipola-Leppänen M, Eriksson JG, Mäkitie O, et al. Early protein intake is associated with body composition and resting energy expenditure in young adults born with very low birth weight. J Nutr. 2015; 145:2084–2091.
Article9. Hay WW. Optimizing nutrition of the preterm infant. Zhongguo Dang Dai Er Ke Za Zhi. 2017; 19:1–21.10. Belfort MB, Rifas-Shiman SL, Sullivan T, Collins CT, McPhee AJ, Ryan P, et al. Infant growth before and after term: effects on neurodevelopment in preterm infants. Pediatrics. 2011; 128:e899–e906.
Article11. Belfort MB, Gillman MW, Buka SL, Casey PH, McCormick MC. Preterm infant linear growth and adiposity gain: trade-offs for later weight status and intelligence quotient. J Pediatr. 2013; 163:1564–1569.
Article12. Latal-Hajnal B, von Siebenthal K, Kovari H, Bucher HU, Largo RH. Postnatal growth in VLBW infants: significant association with neurodevelopmental outcome. J Pediatr. 2003; 143:163–170.
Article13. Chong CYL, Bloomfield FH, O'Sullivan JM. Factors affecting gastrointestinal microbiome development in neonates. Nutrients. 2018; 10:274.
Article14. Commare CE, Tappenden KA. Development of the infant intestine: implications for nutrition support. Nutr Clin Pract. 2007; 22:159–173.
Article15. Berni Canani R, Passariello A, Buccigrossi V, Terrin G, Guarino A. The nutritional modulation of the evolving intestine. J Clin Gastroenterol. 2008; 42:Suppl 3 Pt 2. S197–S200.
Article16. Amin H, Holst JJ, Hartmann B, Wallace L, Wright J, Sigalet DL. Functional ontogeny of the proglucagon- derived peptide axis in the premature human neonate. Pediatrics. 2008; 121:e180–e186.17. Kitanaka T, Alonso JG, Gilbert RD, Siu BL, Clemons GK, Longo LD. Fetal responses to long-term hypoxemia in sheep. Am J Physiol. 1989; 256:R1348–R1354.
Article18. Stockman JA 3rd, Clark DA. Weight gain: a response to transfusion in selected preterm infants. Am J Dis Child. 1984; 138:828–830.
Article19. Harding JE, Cormack BE, Alexander T, Alsweiler JM, Bloomfield FH. Advances in nutrition of the newborn infant. Lancet. 2017; 389:1660–1668.
Article20. Sunehag A, Ewald U, Larsson A, Gustafsson J. Glucose production rate in extremely immature neonates (< 28 weeks) studied by use of deuterated glucose. Pediatr Res. 1993; 33:97–100.
Article21. Chacko S, Sunehag A. Gluconeogenesis continues in premature infants receiving total parenteral nutrition. Arch Dis Child Fetal Neonatal Ed. 2010; 95:F413–F418.
Article22. Rozance PJ, Hay WW Jr. IModern management of preterm infants prevents adverse developmental outcomes from hypoglycemia. Pediatrics. 2016; 138:e20162881.
Article23. Goode RH, Rettiganti M, Li J, Lyle RE, Whiteside-Mansell L, Barrett KW, et al. Developmental outcomes of preterm infants with neonatal hypoglycemia. Pediatrics. 2016; 138:e20161424.
Article24. Mohsen L, Abou-Alam M, El-Dib M, Labib M, Elsada M, Aly H. A prospective study on hyperglycemia and retinopathy of prematurity. J Perinatol. 2014; 34:453–457.
Article25. Picard M, Juster RP, McEwen BS. Mitochondrial allostatic load puts the ‘gluc’ back in glucocorticoids. Nat Rev Endocrinol. 2014; 10:303–310.
Article26. Stoll B, Horst DA, Cui L, Chang X, Ellis KJ, Hadsell DL, et al. Chronic parenteral nutrition induces hepatic inflammation, steatosis, and insulin resistance in neonatal pigs. J Nutr. 2010; 140:2193–2200.
Article27. Wang A, Huen SC, Luan HH, Yu S, Zhang C, Gallezot JD, et al. Opposing effects of fasting metabolism on tissue tolerance in bacterial and viral inflammation. Cell. 2016; 166:1512–1525.
Article28. Basu SK, Kaiser JR, Guffey D, Minard CG, Guillet R, Gunn AJ. CoolCap Study Group. Hypoglycaemia and hyperglycaemia are associated with unfavourable outcome in infants with hypoxic ischaemic encephalopathy: a post hoc analysis of the CoolCap Study. Arch Dis Child Fetal Neonatal Ed. 2016; 101:F419–F455.
Article29. Jing YH, Song YF, Yao YM, Yin J, Wang DG, Gao LP. Retardation of fetal dendritic development induced by gestational hyperglycemia is associated with brain insulin/ IGF-I signals. Int J Dev Neurosci. 2014; 37:15–20.
Article30. Meetze W, Bowsher R, Compton J, Moorehead H. Hyperglycemia in extremely- low-birth-weight infants. Biol Neonate. 1998; 74:214–221.
Article31. Beardsall K, Vanhaesebrouck S, Ogilvy-Stuart AL, Ahluwalia JS, Vanhole C, Palmer C, et al. A randomised controlled trial of early insulin therapy in very low birth weight infants, “NIRTURE” (neonatal insulin replacement therapy in Europe). BMC Pediatr. 2007; 7:29.
Article32. Zamir I, Tornevi A, Abrahamsson T, Ahlsson F, Engström E, Hallberg B, et al. Hyperglycemia in extremely preterm infants-insulin treatment, mortality and nutrient intakes. J Pediatr. 2018; 200:104–110.
Article33. Burattini I, Bellagamba MP, Spagnoli C, D'Ascenzo R, Mazzoni N, Peretti A, et al. Targeting 2.5 versus 4 g/kg/day of amino acids for extremely low birth weight infants: a randomized clinical trial. J Pediatr. 2013; 163:1278–1282.
Article34. Bellagamba M, Carmenati E, D'Ascenzo R, Malatesta M, Spagnoli C, Biagetti C, et al. One extra gram of protein to preterm infants from birth to 1800 g: a single-blinded randomized clinical trial. J Pediatr Gastroenterol Nutr. 2016; 62:879–884.35. Ogilvy-Stuart AL, Beardsall K. Management of hyperglycaemia in the preterm infant. Arch Dis Child Fetal Neonatal Ed. 2010; 95:F126–F131.
Article36. Lapillonne A, Eleni dit Trolli S, Kermorvant-Duchemin E. Postnatal docosahexaenoic acid deficiency is an inevitable consequence of current recommendations and practices in preterm infants. Neonatology. 2010; 98:397–403.
Article37. Tam EWY, Chau V, Barkovich AJ, Ferriero DM, Miller SP, Rogers EE, et al. Early postnatal docosahexaenoic acid levels and improved preterm brain development. Pediatr Res. 2016; 79:723–730.
Article38. Carlson SE, Werkman SH, Rhodes PG, Tolley EA. Visual acuity development in healthy preterm infants: effect of marine oil supplementation. Am J Clin Nutr. 1993; 58:35–42.
Article39. Gould JF, Colombo J, Collins CT, Makrides M, Hewawasam E, Smithers LG. Assessing whether early attention of very preterm infants can be improved by an omega-3 long-chain polyunsaturated fatty acid intervention: a follow-up of a randomised controlled trial. BMJ Open. 2018; 8:e020043.
Article40. El Kasmi KC, Anderson AL, Devereaux MW, Vue PM, Zhang W, Setchell KD, et al. Phytosterols promote liver injury and Kupffer cell activation in parenteral nutrition-associated liver disease. Sci Transl Med. 2013; 5:206ra137.
Article41. Anez-Bustillos L, Dao DT, Fell GL, Baker MA, Gura KM, Bistrian BR, et al. Redefining essential fatty acids in the era of novel intravenous lipid emulsions. Clin Nutr. 2018; 37:784–789.
Article42. Hay WW Jr, Brown , LD , Regnault TRH. Fetal requirements and placental transfer of nitrogenous compounds. In : Polin R, Abman S, Benetz W, Rowitch D, editors. Fetal and neonatal physiology. 5th ed. Philadelphia: Elsevier;2016. p. 444–458.43. Ziegler EE, O'Donnell AM, Nelson SE, Fomon SJ. Body composition of the reference fetus. Growth. 1976; 40:329–341.44. Thureen PJ, Anderson AH, Baron KA, Melara DL, Hay WW Jr, Fennessey PV. Protein balance in the first week of life in ventilated neonates receiving parenteral nutrition. Am J Clin Nutr. 1998; 68:1128–1135.
Article45. Hay WW, Ziegler EE. Growth failure among preterm infants is not innocuous and must be prevented. J Perinatol. 2016; 36:500–502.
Article46. Miller M, Vaidya R, Rastogi D, Bhutada A, Rastogi S. From parenteral to enteral nutrition: a nutrition-based approach for evaluating postnatal growth failure in preterm infants. JPEN J Parenter Enteral Nutr. 2014; 38:489–497.47. Osborn DA, Schindler T, Jones LJ, Sinn JK, Bolisetty S. Higher versus lower amino acid intake in parenteral nutrition for newborn infants. Cochrane Database Syst Rev. 2018; 3:CD005949.
Article48. Ridout E, Melara D, Rottinghaus S, Thureen PJ. Blood urea nitrogen concentration as a marker of amino- acid intolerance in neonates with birthweight less than 1250 g. J Perinatol. 2005; 25:130–133.
Article49. Micheli JL, Schutz Y. Protein. In : Tsang RC, Lucas A, Uauy R, Zlotkin S, editors. Nutritional needs of the preterm infant; Scientific basis and practical guidelines. Pawling, NY: Caduceus Medical Publishers;1993. p. 29–46.50. Kashyap S, Forsyth M, Zucker C, Ramakrishnan R, Dell RB, Heird WC. Effects of varying protein and energy intakes on growth and metabolic response in low birth weight infants. J Pediatr. 1986; 108:955–963.
Article51. Smart JL. Vulnerability of developing brain to undernutrition. Ups J Med Sci Suppl. 1990; 48:21–41.52. Smart JL. Critical periods in brain development. In : Bock GR, Whelan J, editors. The childhood environment and adult disease: Ciba Foundation Symposium 156. Chichester: Wiley;1991. p. 109–128.53. Beauport L, Schneider J, Faouzi M, Hagmann P, Hüppi PS, Tolsa JF, et al. Impact of early nutritional intake on preterm brain: a magnetic resonance imaging study. J Pediatr. 2017; 181:29–36.e1.
Article54. Reid J, Makrides M, McPhee AJ, Stark MJ, Miller J, Collins CT. The effect of increasing the protein content of human milk fortifier to 1.8 g/100 mL on growth in preterm infants: a randomised controlled trial. Nutrients. 2018; 10:634.
Article55. Morgan C, McGowan P, Herwitker S, Hart AE, Turner MA. Postnatal head growth in preterm infants: a randomized controlled parenteral nutrition study. Pediatrics. 2014; 133:e120–e128.
Article56. Clark RH, Chace DH, Spitzer AR. Effects of two different doses of amino acid supplementation on growth and blood amino acid levels in premature neonates admitted to the neonatal intensive care unit: a randomized, controlled trial. Pediatrics. 2007; 120:1286–1296.
Article57. Poindexter BB, Langer JC, Dusick AM, Ehrenkranz RA. National Institute of Child Health and Human Development Neonatal Research Network. Early provision of parenteral amino acids in extremely low birth weight infants: relation to growth and neurodevelopmental outcome. J Pediatr. 2006; 148:300–305.
Article58. Lucas A, Morley R, Cole TJ, Gore SM, Lucas PJ, Crowle P, et al. Early diet in preterm babies and developmental status at 18 months. Lancet. 1990; 335:1477–1481.
Article59. Tottman AC, Alsweiler JM, Bloomfield FH, Gamble G, Jiang Y, Leung M, et al. Long-term outcomes of hyperglycemic preterm infants randomized to tight glycemic control. J Pediatr. 2018; 193:68–75.e1.
Article60. SIFT Investigators Group. Early enteral feeding strategies for very preterm infants: current evidence from Cochrane reviews. Arch Dis Child Fetal Neonatal Ed. 2013; 98:F470–F472.61. Owens L, Burrin DG, Berseth CL. Minimal enteral feeding induces maturation of intestinal motor function but not mucosal growth in neonatal dogs. J Nutr. 2002; 132:2717–2722.
Article62. Niinikoski H, Stoll B, Guan X, Kansagra K, Lambert BD, Stephens J, et al. Onset of small intestinal atrophy is associated with reduced intestinal blood flow in TPN-fed neonatal piglets. J Nutr. 2004; 134:1467–1474.
Article63. Arnon S, Sulam D, Konikoff F, Regev RH, Litmanovitz I, Naftali T. Very early feeding in stable small for gestational age preterm infants: a randomized clinical trial. J Pediatr (Rio J). 2013; 89:388–393.
Article64. Abiramalatha T, Thomas N, Gupta V, Viswanathan A, McGuire W. High versus standard volume enteral feeds to promote growth in preterm or low birth weight infants. Cochrane Database Syst Rev. 2017; 9:CD012413.
Article65. Oddie SJ, Young L, McGuire W. Slow advancement of enteral feed volumes to prevent necrotising enterocolitis in very low birth weight infants. Cochrane Database Syst Rev. 2017; 8:CD001241.
Article66. Radmacher PG, Adamkin DH. Fortification of human milk for preterm infants. Semin Fetal Neonatal Med. 2017; 22:30–35.
Article67. Kuschel CA, Harding JE. Multicomponent fortified human milk for promoting growth in preterm infants. Cochrane Database Syst Rev. 2004; (1):CD000343.
Article68. Arnold M, Adamkin D, Radmacher P. Improving fortification with weekly analysis of human milk for VLBW infants. J Perinatol. 2017; 37:194–196.
Article69. Rochow N, Fusch G, Choi A, Chessell L, Elliott L, McDonald K, et al. Target fortification of breast milk with fat, protein, and carbohydrates for preterm infants. J Pediatr. 2013; 163:1001–1007.
Article70. Arslanoglu S, Moro GE, Ziegler EE. The Wapm Working Group On Nutrition. Optimization of human milk fortification for preterm infants: new concepts and recommendations. J Perinat Med. 2010; 38:233–238.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Support in Premature Infants
- Strategies to support language development in neonatal intensive care unit: a narrative review
- Clinical Significance of the Nutritional Support Team for Preterm Infants in a Neonatal Intensive Care Unit
- Predictors of Early Postpartum Depression in Mothers of Preterm Infants in Neonatal Intensive Care Units
- Organisation of Special and Intensive Care Facilities for Babies