Korean J Radiol.
2018 Oct;19(5):880-887. 10.3348/kjr.2018.19.5.880.
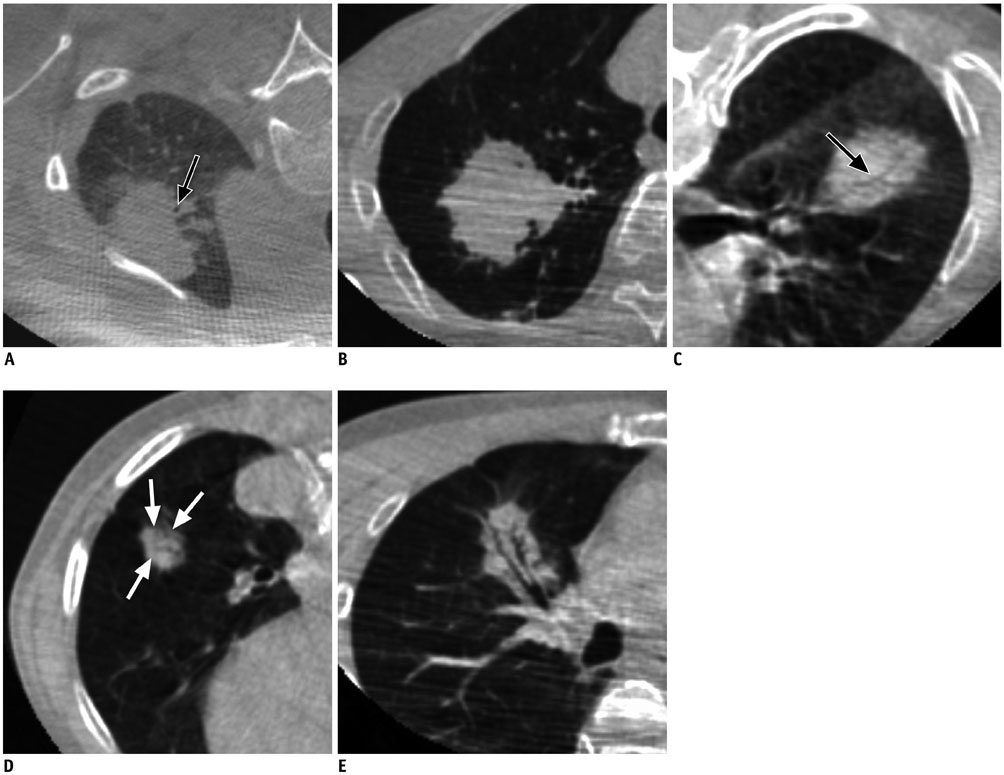
Open Bronchus Sign on CT: A Risk Factor for Hemoptysis after Percutaneous Transthoracic Biopsy
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, and Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul 03080, Korea. cmpark.morphius@gmail.com
- 2Cancer Research Institute, Seoul National University, Seoul 03080, Korea.
- 3Department of Radiology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul 05030, Korea.
- KMID: 2418551
- DOI: http://doi.org/10.3348/kjr.2018.19.5.880
Abstract
OBJECTIVE
We hypothesized that open bronchi within target pulmonary lesions are associated with percutaneous transthoracic needle biopsy (PTNB)-related hemoptysis. We sought to analyze and compare patient characteristics and target features as well as biopsy-related factors between patients with and without PTNB-related hemoptysis.
MATERIALS AND METHODS
We retrospectively analyzed 1484 patients (870 males and 614 females; median age, 66 years) who had undergone 1569 cone-beam CT (CBCT)-guided PTNBs. Patient characteristics (sex, age, and pathologic diagnosis), nodule features (nodule type, size, location, and presence of an open bronchus in target nodules), and biopsy-related factors (biopsy needle size, pleura-to-target distance, blood test results, open bronchus unavoidability [OBU] index, etc.) were investigated. OBU index, which was assessed using the pre-procedural CBCT, was a subjective scoring system for the probability of needle penetration into the open bronchus. Univariate analysis and subsequent multivariate logistic regression analysis were conducted to reveal the independent risk factors for PTNB-related hemoptysis. For a subgroup of nodules with open bronchi, a trend analysis between the occurrence of hemoptysis and the OBU index was performed.
RESULTS
The independent risk factors for hemoptysis were sex (female; odds ratio [OR], 1.918; p < 0.001), nodule size (OR, 0.837; p < 0.001), open bronchus (OR, 2.101; p < 0.001), and pleura-to-target distance (OR, 1.135; p = 0.003). For the target nodules with open bronchi, a significant trend between hemoptysis and OBU index (p < 0.001) was observed.
CONCLUSION
An open bronchus in a biopsy target is an independent predictor of hemoptysis, and careful imaging review may potentially reduce PTNB-related hemoptysis.
Keyword
MeSH Terms
Figure
Reference
-
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017; 67:7–30.
Article2. Callister ME, Baldwin DR, Akram AR, Barnard S, Cane P, Draffan J, et al. British Thoracic Society guidelines for the investigation and management of pulmonary nodules. Thorax. 2015; 70:Suppl 2. ii1–ii54.3. Ost DE, Gould MK. Decision making in patients with pulmonary nodules. Am J Respir Crit Care Med. 2012; 185:363–372.
Article4. Rotolo N, Floridi C, Imperatori A, Fontana F, Ierardi AM, Mangini M, et al. Comparison of cone-beam CT-guided and CT fluoroscopy-guided transthoracic needle biopsy of lung nodules. Eur Radiol. 2016; 26:381–389.
Article5. Song YS, Park CM, Park KW, Kim KG, Lee HJ, Shim MS, et al. Does antiplatelet therapy increase the risk of hemoptysis during percutaneous transthoracic needle biopsy of a pulmonary lesion? AJR Am J Roentgenol. 2013; 200:1014–1019.
Article6. Lee BE, Kletsman E, Rutledge JR, Korst RJ. Utility of endobronchial ultrasound-guided mediastinal lymph node biopsy in patients with non-small cell lung cancer. J Thorac Cardiovasc Surg. 2012; 143:585–590.
Article7. Lee SM, Park CM, Lee KH, Bahn YE, Kim JI, Goo JM. C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of lung nodules: clinical experience in 1108 patients. Radiology. 2014; 271:291–300.
Article8. Wang Y, Jiang F, Tan X, Tian P. CT-guided percutaneous transthoracic needle biopsy for paramediastinal and nonparamediastinal lung lesions: diagnostic yield and complications in 1484 patients. Medicine (Baltimore). 2016; 95:e4460.9. Lim WH, Park CM, Yoon SH, Lim HJ, Hwang EJ, Lee JH, et al. Time-dependent analysis of incidence, risk factors and clinical significance of pneumothorax after percutaneous lung biopsy. Eur Radiol. 2018; 28:1328–1337.
Article10. Choo JY, Park CM, Lee NK, Lee SM, Lee HJ, Goo JM. Percutaneous transthoracic needle biopsy of small (≤ 1 cm) lung nodules under C-arm cone-beam CT virtual navigation guidance. Eur Radiol. 2013; 23:712–719.11. Jin KN, Park CM, Goo JM, Lee HJ, Lee Y, Kim JI, et al. Initial experience of percutaneous transthoracic needle biopsy of lung nodules using C-arm cone-beam CT systems. Eur Radiol. 2010; 20:2108–2115.
Article12. Saba L, Montisci R, Raz E, Sanfilippo R, Suri JS, Piga M. Association between carotid artery plaque type and cerebral microbleeds. AJNR Am J Neuroradiol. 2012; 33:2144–2150.
Article13. Khan MF, Straub R, Moghaddam SR, Maataoui A, Gurung J, Wagner TO, et al. Variables affecting the risk of pneumothorax and intrapulmonal hemorrhage in CT-guided transthoracic biopsy. Eur Radiol. 2008; 18:1356–1363.
Article14. Tai R, Dunne RM, Trotman-Dickenson B, Jacobson FL, Madan R, Kumamaru KK, et al. Frequency and severity of pulmonary hemorrhage in patients undergoing percutaneous CT-guided transthoracic lung biopsy: single-institution experience of 1175 cases. Radiology. 2016; 279:287–296.
Article15. Yeow KM, See LC, Lui KW, Lin MC, Tsao TC, Ng KF, et al. Risk factors for pneumothorax and bleeding after CT-guided percutaneous coaxial cutting needle biopsy of lung lesions. J Vasc Interv Radiol. 2001; 12:1305–1312.
Article16. Yildirim E, Kirbas I, Harman A, Ozyer U, Tore HG, Aytekin C, et al. CT-guided cutting needle lung biopsy using modified coaxial technique: factors effecting risk of complications. Eur J Radiol. 2009; 70:57–60.
Article17. Anzidei M, Sacconi B, Fraioli F, Saba L, Lucatelli P, Napoli A, et al. Development of a prediction model and risk score for procedure-related complications in patients undergoing percutaneous computed tomography-guided lung biopsy. Eur J Cardiothorac Surg. 2015; 48:e1–e6.
Article18. Cheng YC, Tsai SH, Cheng Y, Chen JH, Chai JW, Chen CC. Percutaneous transthoracic lung biopsy: comparison between C-arm cone-beam CT and conventional CT guidance. Transl Oncol. 2015; 8:258–264.
Article19. Choi MJ, Kim Y, Hong YS, Shim SS, Lim SM, Lee JK. Transthoracic needle biopsy using a C-arm cone-beam CT system: diagnostic accuracy and safety. Br J Radiol. 2012; 85:e182–e187.
Article20. Jaconi M, Pagni F, Vacirca F, Leni D, Corso R, Cortinovis D, et al. C-arm cone-beam CT-guided transthoracic lung core needle biopsy as a standard diagnostic tool: an observational study. Medicine (Baltimore). 2015; 94:e698.21. Jiao de C, Li TF, Han XW, Wu G, Ma J, Fu MT, et al. Clinical applications of the C-arm cone-beam CT-based 3D needle guidance system in performing percutaneous transthoracic needle biopsy of pulmonary lesions. Diagn Interv Radiol. 2014; 20:470–474.
Article22. Otto S, Mensel B, Friedrich N, Schäfer S, Mahlke C, von Bernstorff W, et al. Predictors of technical success and rate of complications of image-guided percutaneous transthoracic lung needle biopsy of pulmonary tumors. PLoS One. 2015; 10:e0124947.
Article23. Choi JW, Park CM, Goo JM, Park YK, Sung W, Lee HJ, et al. C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of small (≤ 20 mm) lung nodules: diagnostic accuracy and complications in 161 patients. AJR Am J Roentgenol. 2012; 199:W322–W330.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Computed tomography of bronchioloalveolar carcinoma showing open bronchus sign
- Air Embolization after Computed Tomography-Guided Percutaneous Transthoracic Needle Biopsy
- Hematoma-Filled Pneumatocele after CT-Guided Percutaneous Transthoracic Needle Lung Biopsy: Two Case Reports
- Painful Percutaneous Transthoracic Needle Biopsy of Schwannoma: A Case Report
- Lung Cancer With CT-Bronchus Sign: Correlation with CT-findings and the Yield of Bronchoscopic Biopsy