J Dent Anesth Pain Med.
2018 Jun;18(3):169-175. 10.17245/jdapm.2018.18.3.169.
Comparative randomized study of propofol target-controlled infusion versus sevoflurane anesthesia for third molar extraction
- Affiliations
-
- 1Concord Repatriation General Hospital, Sydney, Australia.
- 2HCF Dental Centre, Sydney, Australia.
- KMID: 2415181
- DOI: http://doi.org/10.17245/jdapm.2018.18.3.169
Abstract
- BACKGROUND
The objective of this study was to compare hemodynamic and recovery characteristics of total intravenous anesthesia using propofol target-controlled infusion (TCI) versus sevoflurane for extraction of four third molar teeth.
METHODS
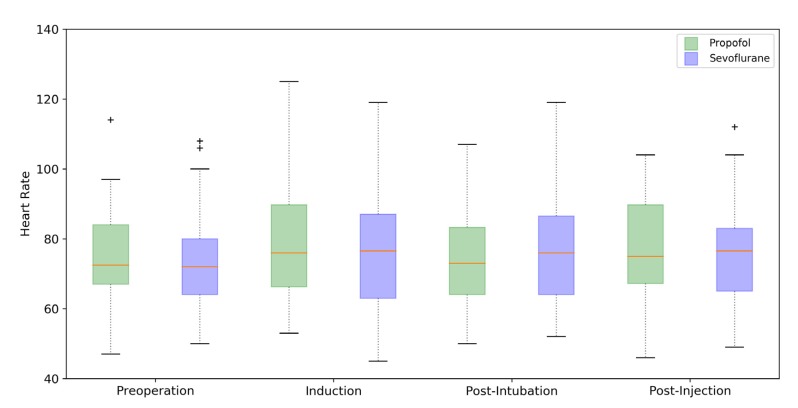
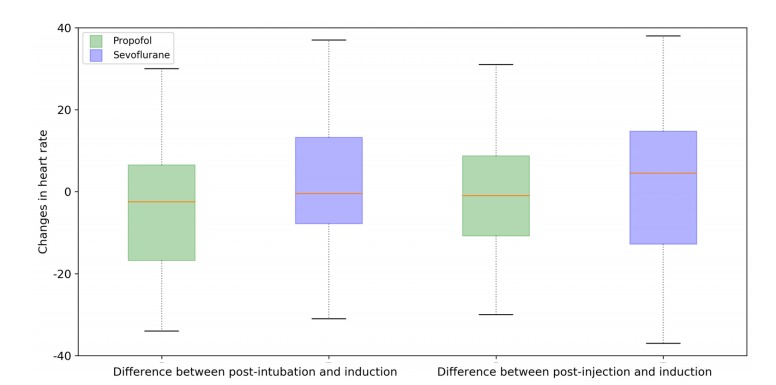
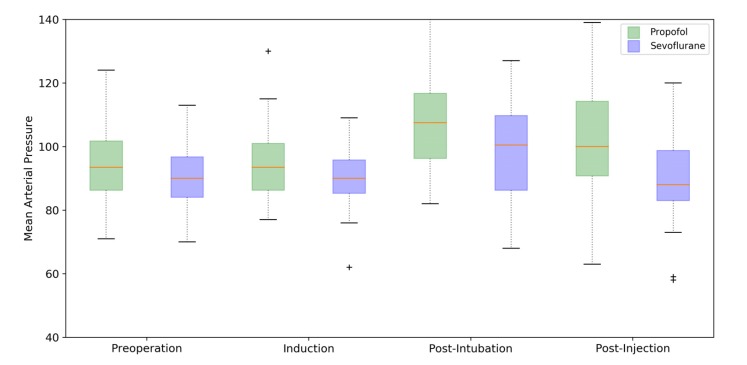
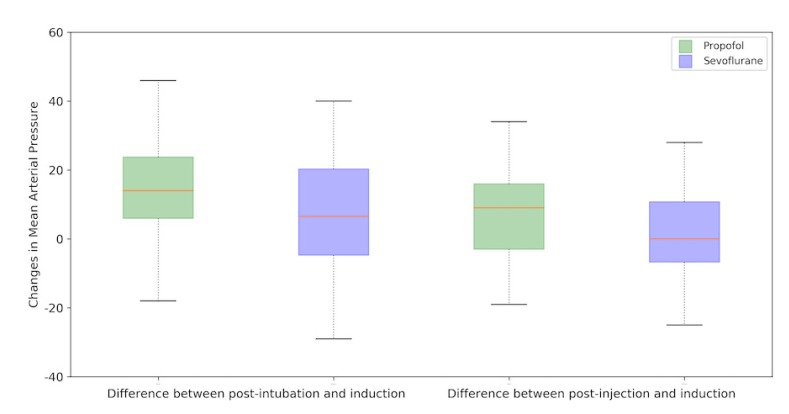
One hundred patients undergoing extraction of four third molar teeth under general anesthesia were randomized to one of two groups. Group 1 received propofol TCI-oxygen for induction and propofol TCI-oxygen-air for maintenance. Group II received a propofol bolus of 2 mg/kg for induction and sevoflurane-oxygen-air for maintenance. Heart rate, mean arterial pressure (MAP), operating time, time to emergence, nausea and vomiting, and sedation and pain scores were measured in each group.
RESULTS
Demographic data, including age, gender, weight, and height, were not significantly different between the two groups. The MAP was significantly higher after intubation (P = 0.007) and injection of anesthesia (P = 0.004) in the propofol group than in the sevoflurane group, with significant reflex bradycardia (P = 0.028). The mean time to emergence from anesthesia using propofol was 25 s shorter than that of sevoflurane (P = 0.02). Postoperatively, the propofol group was less sedated than the sevoflurane group at 30 min (0.02 versus 0.12), but this difference was not significant (P = 0.065).
CONCLUSION
Both propofol TCI and sevoflurane are good alternatives for induction and maintenance of anesthesia for short day-case surgery. However, propofol TCI does not blunt the hemodynamic response to sudden, severe stimuli as strongly as sevoflurane, and this limitation may be a cause for concern in patients with cardiac comorbidities.
Keyword
MeSH Terms
Figure
Reference
-
1. Raeder J, Gupta A, Pedersen FM. Recovery characteristics of sevoflurane- or propofol-based anaesthesia for day-care surgery. Acta Anaesthesiol Scand. 1997; 41:988–994. PMID: 9311396.
Article2. Matsuura H, Inoue S, Kawagucji M. The risk of postoperative nausea and vomiting between surgical patients received propofol and sevoflurane anesthesia: A matched study. Acta Anaesthesiol Taiwan. 2016; 54:114–120. PMID: 27825646.
Article3. Pokkinen SM, Yli-Hankala A, Kalliomaki ML. The effects of propofol vs. sevoflurane on post-operative pain and need of opioid. Acta Anaesthesiol Scand. 2014; 58:980–985. PMID: 25039403.
Article4. Absalom AR, Mani V, De Smet T, Struys MM. Pharmacokinetic models for propofol – defining and illuminating the devil in the detail. Br J Anaesth. 2009; 103:26–37. PMID: 19520702.5. Russell D, Wilkes MP, Hunter SC, Glen JB, Hutton P, Kenny GNC. Manual compared with target-controlled infusion of propofol. Br J Anaesth. 1995; 75:562–566. PMID: 7577281.
Article6. Glen JB. The development of ‘Diprifusor’: a TCI system for propofol. Anaesthesia. 1998; (53 Suppl 1):13–21.
Article7. Gray JM, Kenny GN. Development of the technology for ‘Diprifusor’ TCI systems. Anaesthesia. 1998; (53 Suppl 1):22–27. PMID: 9640111.
Article8. Bharti N, Chari P, Kumar P. Effect of sevoflurane versus propofol-based anesthesia on the hemodynamic response and recovery characteristics in patients undergoing microlaryngeal surgery. Saudi J Anaesth. 2012; 6:380–384. PMID: 23493938.
Article9. Godet G, Watremez C, Kettani CE, Soriano C, Coriat P. A comparison of sevoflurane, target-controlled infusion propofol, and propofol/isoflurane anesthesia in patients undergoing carotid surgery; a quality of anesthesia and recovery profile. Anesth Analg. 2001; 93:560–565. PMID: 11524318.
Article10. Shimonov M, Ezri T, Blecher M, Cherniak A, Azamfirei L. Hemodynamic effects of sevoflurane versus propofol anesthesia for laparoscopic radiofrequency ablation of liver tumours. S AFR J Anesth Analg. 2006; 12:149–152.11. Smith I, Thwaites AJ. Target-controlled propofol vs. sevoflurane; a double-blind, randomized comparison in day-case anaesthesia. Anaesthesia. 1999; 54:745–752. PMID: 10460526.12. Akkurt BC, Temiz M, Inanoglu K, Aslan A, Turhanoglu S, Asfuroglu Z, et al. Comparison of recovery characteristics, postoperative nausea and vomiting, and gastrointestinal motility with total intravenous anesthesia with propofol versus inhalation anesthesia with desflurane for laparoscopic cholecystectomy: a randomized controlled study. Curr Ther Res Clin Exp. 2009; 70:95–103.
Article13. Watson KR, Shah MV. Clinical comparison of ‘single agent’ anaesthesia with sevoflurane versus target controlled infusion of propofol. Br J Anaesth. 2000; 85:541–546. PMID: 11064611.
Article14. Fahy BG, Chau DF. The technology of processed electroencephalogram monitoring devices for assessment of depth of anesthesia. Anesth Analg. 2018; 126:111–117. PMID: 28786839.
Article15. Ellerkmann RK, Soegle M, Riese G, Zinserling J, Wirz S, Hoeft A, et al. The Entropy Module and Bispectral Index as guidance for propofol-remifentanil anaesthesia in combination with regional anaesthesia compared with a standard clinical practice group. Anaesth Intensive Care. 2010; 38:159–166. PMID: 20191792.
Article16. Höcker J, Tonner PH, Böllert P, Paris A, Scholz J, Meier-Paika C, et al. Propofol/remifentanil vs. sevoflurane/remifentanil for longlasting surgical procedures: a randomized controlled trial. Anaesthesia. 2006; 61:752–757. PMID: 16867087.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Target Controlled Conscious Sedation with Propofol and Remifentanil for the Extraction of Impacted Wisdom Teeth
- Target controlled infusion for total intravenous anesthesia in children
- A Comparison of the Recovery Characteristics of Propofol and Sevoflurane Anesthesia under Bispectral Index System Monitoring
- Comparison of Sevoflurane-Nitrous Oxide and Target- Controlled Propofol with Fentanyl Anesthesia for Hysteroscopy
- Three minutes propofol after sevoflurane anesthesia to prevent emergence agitation following inguinal hernia repair in children: a randomized controlled trial