Trends and Outcomes of Transcatheter Aortic Valve Implantation (TAVI) in Korea: the Results of the First Cohort of Korean TAVI Registry
- Affiliations
-
- 1Department of Cardiology, Korea University Anam Hospital, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea.
- 2Department of Cardiology, CHA Bundang Medical Center, Department of Internal Medicine, CHA University School of Medicine, Seongnam, Korea.
- 3Department of Cardiology, Asan Medical Center, Department of Internal Medicine, University of Ulsan College of Medicine, Seoul, Korea.
- 4Department of Cardiology, Seoul National University Hospital, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea. hyosoo@snu.ac.kr
- 5Department of Cardiology, Severance Hospital, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 6Department of Cardiology, Samsung Medical Center, Department of Internal Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 7Department of Cardiology, Seoul St. Mary's Hospital, Department of Internal Medicine, The Catholic University of Korea School of Medicine, Seoul, Korea. kiyuk@catholic.ac.kr
- KMID: 2414907
- DOI: http://doi.org/10.4070/kcj.2018.0117
Abstract
- BACKGROUND AND OBJECTIVES
There has been no nation-wide data on the outcomes of transcatheter aortic valve implantation (TAVI) after commercialization of TAVI in Korea. We report clinical features and outcomes of the first cohort of TAVI performed from Jun 2015 to Jun 2017 in Korea.
METHODS
The first cohort of Korean-TAVI (K-TAVI) registry includes 576 consecutive patients with severe symptomatic aortic stenosis who underwent TAVI from 17 Korean hospitals for 2 years.
RESULTS
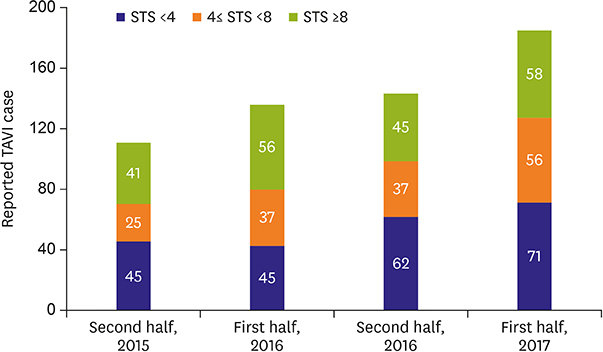
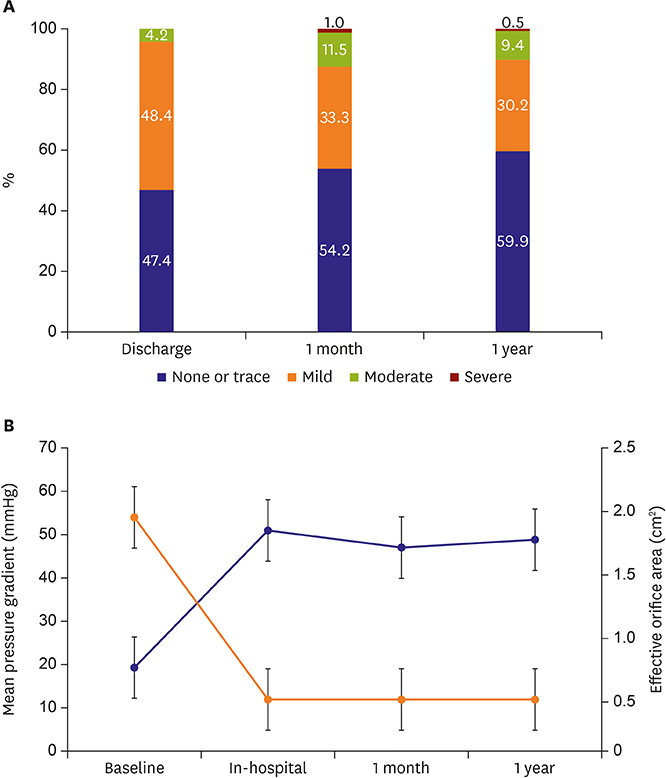
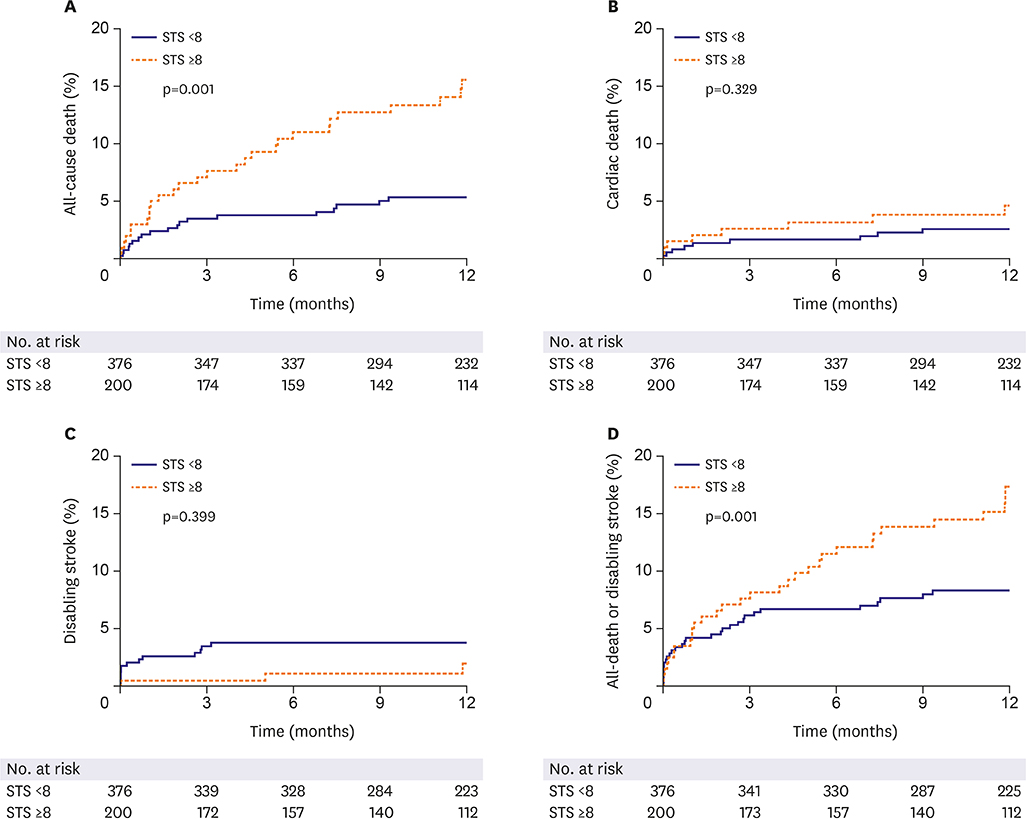
Most of TAVI procedures were performed for septuagenarians and octogenarians (90.8%) through transfemoral approach (98.3%). The rate of device success was 92.5% and permanent pacemaker was implanted in 5.6%. In successive years, incidences of paravalvular leakage (PVL) and major bleeding declined. Society of Thoracic Surgeons (STS) score was 5.2 (3.0 to 9.0) and 34.7% of patients had high surgical risk (STS ≥8). One-year all-cause death occurred in 8.9% and was significantly lower in low to intermediate risk one than in high risk (5.4% vs. 15.5%, p < 0.001). The independent predictors of 1-year mortality were age (hazard ratio [HR], 1.087; 95% confidence interval [CI], 1.036-1.141; p=0.001), moderate or severe PVL (HR, 4.631; 95% CI, 1.624-13.203; p=0.004) and end-stage renal disease (HR, 5.785; 95% CI, 2.717-12.316; p < 0.001).
CONCLUSIONS
K-TAVI registry showed favorable 1-year outcomes with decreasing complication rate over time in real-world Korean patients. Two-thirds of patients were low to intermediate surgical risk and showed a significantly lower mortality than the high-risk patients, suggesting the promising future on the expanded indications of TAVI.
MeSH Terms
Figure
Cited by 7 articles
-
Moderate Aortic Valve Stenosis with Left Ventricular Systolic Dysfunction: Potential Role of Early Aortic Valve Replacement
Ju-Hee Lee
Korean Circ J. 2020;50(9):801-803. doi: 10.4070/kcj.2020.0301.Comparing the Procedural and Clinical Outcomes of Sapien XT and Sapien 3 Valves in Transcatheter Aortic Valve Replacement in Korean Patients
Hyungdon Kook, Duck Hyun Jang, Kyung-Sook Yang, Hyung Joon Joo, Jae Hyoung Park, Soon Jun Hong, Do-Sun Lim, Seung-Hyuk Choi, Young Jin Choi, Kiyuk Chang, Cheol Woong Yu
Korean Circ J. 2020;50(10):907-922. doi: 10.4070/kcj.2020.0061.Sapien 3 versus Sapien XT Balloon-expanding Valve for Transcatheter Aortic Valve Replacement: Improved Immediate and Late Outcomes at the Expense of Smaller Effective Orifice Area
Young-Guk Ko
Korean Circ J. 2020;50(10):923-924. doi: 10.4070/kcj.2020.0353.Good Patients Make Favorable Clinical Outcome: K-TAVI Registry Reports
Choongki Kim, Myeong-Ki Hong
Korean Circ J. 2018;48(5):427-429. doi: 10.4070/kcj.2018.0095.Long-term Survival in Korean Elderly Patients with Symptomatic Severe Aortic Stenosis Who Refused Aortic Valve Replacement
Jin Kyung Oh, Jae-Hyeong Park, Jin Kyung Hwang, Chang Hoon Lee, Jong Seon Park, Joong-Il Park, Hoon-Ki Park, Jung Sun Cho, Bong-suk Seo, Seok-Woo Seong, Byung Joo Sun, Jae-Hwan Lee, In-Whan Seong
Korean Circ J. 2019;49(2):160-169. doi: 10.4070/kcj.2018.0208.Aortic Stenosis and Transcatheter Aortic Valve Implantation: Current Status and Future Directions in Korea
Choongki Kim, Myeong-Ki Hong
Korean Circ J. 2019;49(4):283-297. doi: 10.4070/kcj.2019.0044.Aortic Valve Replacement in the Era of Transcatheter Aortic Valve Implantation: Current Status in Korea
Suk Ho Sohn, Kyung Hwan Kim, Yoonjin Kang, Jae Woong Choi, Seung Hyun Lee, Sung Ho Shinn, Cheong Lim, Kiick Sung, Jae Suk Yoo, Suk Jung Choo
J Korean Med Sci. 2023;38(48):e404. doi: 10.3346/jkms.2023.38.e404.
Reference
-
1. Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010; 363:1597–1607.2. Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011; 364:2187–2198.3. Leon MB, Smith CR, Mack MJ, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016; 374:1609–1620.4. Reardon MJ, Van Mieghem NM, Popma JJ, et al. Surgical or transcatheter aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2017; 376:1321–1331.5. Grube E, Schuler G, Buellesfeld L, et al. Percutaneous aortic valve replacement for severe aortic stenosis in high-risk patients using the second- and current third-generation self-expanding CoreValve prosthesis: device success and 30-day clinical outcome. J Am Coll Cardiol. 2007; 50:69–76.6. Kappetein AP, Head SJ, Genereux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. Eur Heart J. 2012; 33:2403–2418.
Article7. Sawa Y, Saito S, Kobayashi J, et al. First clinical trial of a self-expandable transcatheter heart valve in Japan in patients with symptomatic severe aortic stenosis. Circ J. 2014; 78:1083–1090.
Article8. Mack MJ, Brennan JM, Brindis R, et al. Outcomes following transcatheter aortic valve replacement in the United States. JAMA. 2013; 310:2069–2077.
Article9. Ludman PF, Moat N, de Belder MA, et al. Transcatheter aortic valve implantation in the United Kingdom: temporal trends, predictors of outcome, and 6-year follow-up: a report from the UK Transcatheter Aortic Valve Implantation (TAVI) Registry, 2007 to 2012. Circulation. 2015; 131:1181–1190.10. Takimoto S, Saito N, Minakata K, et al. Favorable clinical outcomes of transcatheter aortic valve implantation in Japanese patients- first report from the Post-Approval K-TAVI Registry. Circ J. 2016; 81:103–109.11. Sinning JM, Ghanem A, Steinhauser H, et al. Renal function as predictor of mortality in patients after percutaneous transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2010; 3:1141–1149.
Article12. Van Mieghem NM, van der Boon RM, Nuis RJ, et al. Cause of death after transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 2014; 83:E277–82.
Article13. Barbash IM, Finkelstein A, Barsheshet A, et al. Outcomes of patients at estimated low, intermediate, and high risk undergoing transcatheter aortic valve implantation for aortic stenosis. Am J Cardiol. 2015; 116:1916–1922.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aortic Stenosis and Transcatheter Aortic Valve Implantation: Current Status and Future Directions in Korea
- Recent updates in transcatheter aortic valve implantation
- Comparison of Early Clinical Results of Transcatheter versus Surgical Aortic Valve Replacement in Symptomatic High Risk Severe Aortic Stenosis Patients
- A Case of Severe Aortic Stenosis Patient With High Operative Risk Treated by Transcatheter Aortic-Valve Implantation
- Transcatheter Aortic Valve Implantation in a Patient with Previous Mitral Valve Replacement