Hip Pelvis.
2018 Jun;30(2):78-85. 10.5371/hp.2018.30.2.78.
Treatment of Periprosthetic Femoral Fractures Following Hip Arthroplasty
- Affiliations
-
- 1Department of Orthopaedic Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea. drjmlee@naver.com
- KMID: 2412688
- DOI: http://doi.org/10.5371/hp.2018.30.2.78
Abstract
- PURPOSE
This study was performed to assess potential improvements in clinical outcomes when applying recent advanced hip arthroplasty surgical techniques and understand the potential relationship between bone mineral density (BMD) and surgical outcomes.
MATERIALS AND METHODS
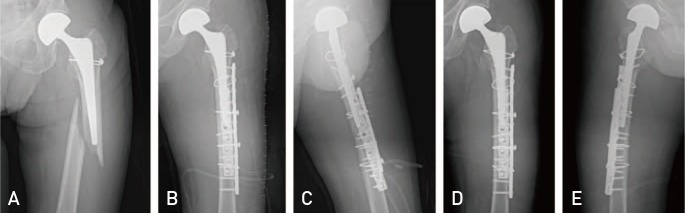
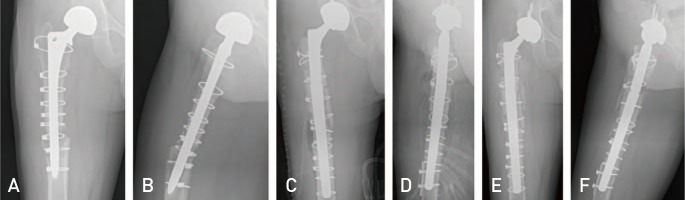
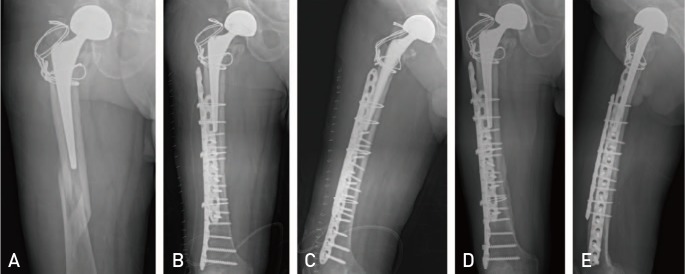
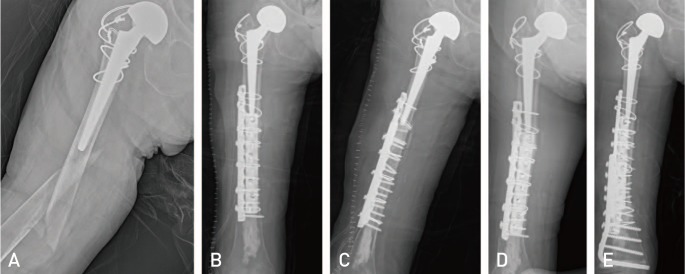
Among 37 cases of periprosthetic femoral fractures after hip arthroplasty treated between March 2014 and September 2016, all included a follow-up of at least one year and were included in this study. Outcomes were evaluated using the Beals and Tower's criteria. BMD was examined in 27 of 37 cases and the relationship between osteoporosis and treatment outcomes was analyzed. Advanced hip arthroplasty surgical approaches varied depending on the fracture type: i) open reduction with wiring for Vancouver A, ii) open reduction with double plate fixation for Vancouver B1, iii) revision THA with long stem for Vancouver B1-Nonunion, B2 and B3, and iv) open reduction with double plate fixation for Vancouver C.
RESULTS
When assessed using the Beals and Tower's criteria, 33 out of 37 (89.2%) patients were excellent and 4 (10.8%) were poor. These outcomes were an improvement compared with series I (81.8%). When analyzed according to the Vancouver classification, patients with type A (n=8), type B1 (n=16), and type B2 (n=2) were all excellent, the patients with type B3 were excellent (n=1) and poor (n=1), and the patients with type C were excellent (n=6) and poor (n=3). The mean BMD was −2.6 (T-score) in 27 of 37 cases and −4.4 in 4 cases with poor prognosis. Osteoporosis was statistically correlated to those classified as poor by Beals and Tower.
CONCLUSION
The results of the analysis suggest that applying new surgical hip arthroplasty treatment approaches leads to improved outcomes compared with the author's previous study. When treating periprosthetic femoral fractures following total hip arthroplasty, an appropriate internal fixation method should be selected, at least in part based on the Vancouver classification. In addition, osteoporosis may be a major prognostic factor for the outcomes of surgical treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Jämsen E, Salonen H, Taukojärvi A, et al. P-436: The incidence of periprosthetic femoral fractures after total hip replacement in the Pirkanmaa Hospital District, Finland during 2002–2010. Eur Geriatr Med. 2015; 6(Suppl 1):S149.
Article2. Richards CJ, Garbuz DS, Masri BA, Duncan CP. Vancouver type B3 periprosthetic fractures: evaluation and treatment. Instr Course Lect. 2009; 58:177–181. PMID: 19385531.3. Beals RK, Tower SS. Periprosthetic fractures of the femur. An analysis of 93 fractures. Clin Orthop Relat Res. 1996; (327):238–246.4. Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005; 20:857–865. PMID: 16230235.5. Lee JM. Periprosthetic femoral fractures after hip arthroplasty. J Korean Hip Soc. 2011; 23:174–183.
Article6. Lee JM, Hwang DW, Choi HJ, Seol YD, Lee DS. Treatment of periprosthetic femoral fractures after hip arthroplasty. J Korean Orthop Assoc. 2010; 45:114–119.
Article7. Lindahl H. Epidemiology of periprosthetic femur fracture around a total hip arthroplasty. Injury. 2007; 38:651–654. PMID: 17477925.
Article8. Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995; 44:293–304. PMID: 7797866.9. Garbuz DS, Masri BA, Duncan CP. Periprosthetic fractures of the femur: principles of prevention and management. Instr Course Lect. 1998; 47:237–242. PMID: 9571424.10. Moreta J, Aguirre U, de Ugarte OS, Jáuregui I, Mozos JL. Functional and radiological outcome of periprosthetic femoral fractures after hip arthroplasty. Injury. 2015; 46:292–298. PMID: 25085599.
Article11. Hannan MT, Felson DT, Anderson JJ. Bone mineral density in elderly men and women: results from the Framingham osteoporosis study. J Bone Miner Res. 1992; 7:547–553. PMID: 1615761.
Article12. Yoon BH, Lee YK, Jo WL, Ha YC, Choi DH, Koo KH. Incidence and risk period of periprosthetic femoral fracture after cementless bipolar hemiarthroplasty in elderly patients. J Arthroplasty. 2016; 31:1326–1330. PMID: 26796775.
Article13. Wilson D, Frei H, Masri BA, Oxland TR, Duncan CP. A biomechanical study comparing cortical onlay allograft struts and plates in the treatment of periprosthetic femoral fractures. Clin Biomech (Bristol, Avon). 2005; 20:70–76.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Periprosthetic Femoral Fractures after Hip Arthroplasty
- Treatment of Periprosthetic Femoral Fractures after Hip Arthroplasty
- Periprosthetic Atypical Femoral Fracture-like Fracture after Hip Arthroplasty: A Report of Three Cases
- Decision-Making and Principle of Management in Periprosthetic Femoral Fracture after Total Hip Arthroplasty
- Management of Ipsilateral Femoral Fracture After Hip Arthroplasty