Korean J Radiol.
2018 Jun;19(3):516-525. 10.3348/kjr.2018.19.3.516.
Nodule Classification on Low-Dose Unenhanced CT and Standard-Dose Enhanced CT: Inter-Protocol Agreement and Analysis of Interchangeability
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam 13620, Korea. lkwrad@gmail.com
- 2Department of Radiology, Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul 03722, Korea.
- 3Department of Radiology and Research Institute of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Seoul 05505, Korea.
- 4Department of Radiology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul 03080, Korea.
- 5Cancer Research Institute, Seoul National University College of Medicine, Seoul 03080, Korea.
- KMID: 2410823
- DOI: http://doi.org/10.3348/kjr.2018.19.3.516
Abstract
OBJECTIVE
To measure inter-protocol agreement and analyze interchangeability on nodule classification between low-dose unenhanced CT and standard-dose enhanced CT.
MATERIALS AND METHODS
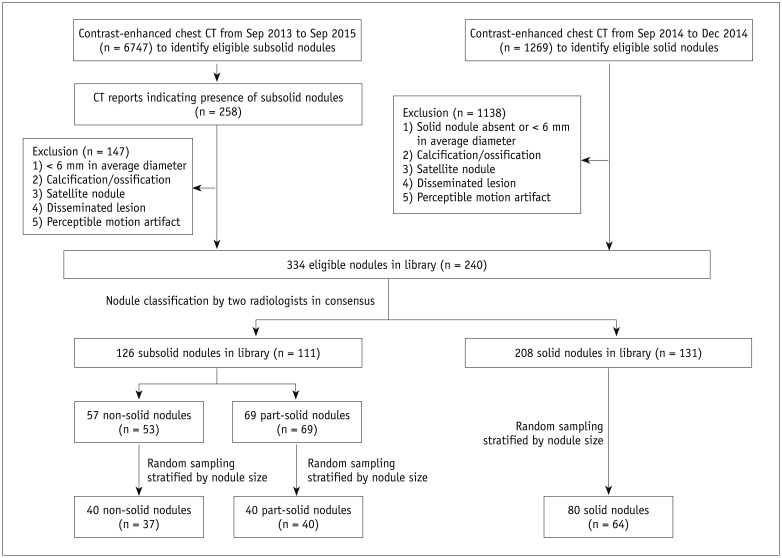
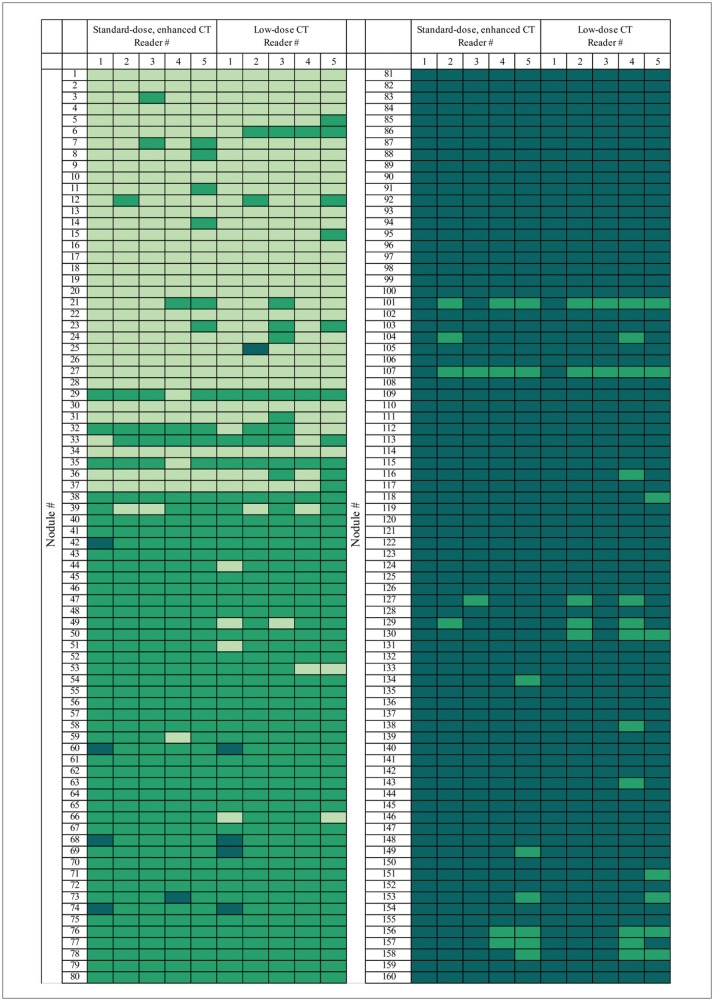
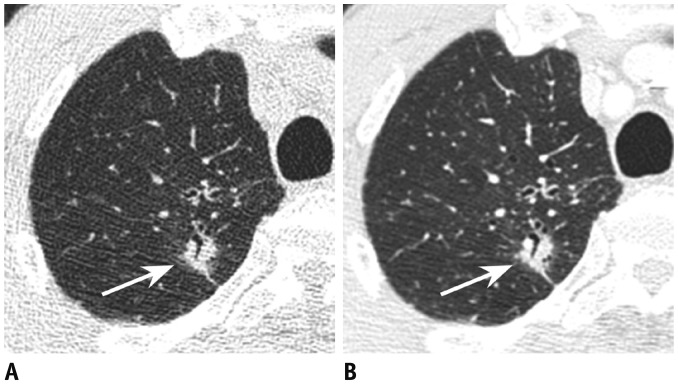
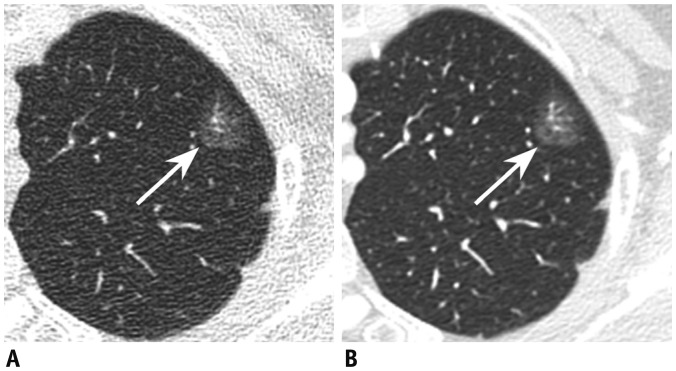
From nodule libraries containing both low-dose unenhanced and standard-dose enhanced CT, 80 solid and 80 subsolid (40 part-solid, 40 non-solid) nodules of 135 patients were selected. Five thoracic radiologists categorized each nodule into solid, part-solid or non-solid. Inter-protocol agreement between low-dose unenhanced and standard-dose enhanced images was measured by pooling κ values for classification into two (solid, subsolid) and three (solid, part-solid, non-solid) categories. Interchangeability between low-dose unenhanced and standard-dose enhanced CT for the classification into two categories was assessed using a pre-defined equivalence limit of 8 percent.
RESULTS
Inter-protocol agreement for the classification into two categories {κ, 0.96 (95% confidence interval [CI], 0.94-0.98)} and that into three categories (κ, 0.88 [95% CI, 0.85-0.92]) was considerably high. The probability of agreement between readers with standard-dose enhanced CT was 95.6% (95% CI, 94.5-96.6%), and that between low-dose unenhanced and standard-dose enhanced CT was 95.4% (95% CI, 94.7-96.0%). The difference between the two proportions was 0.25% (95% CI, −0.85-1.5%), wherein the upper bound CI was markedly below 8 percent.
CONCLUSION
Inter-protocol agreement for nodule classification was considerably high. Low-dose unenhanced CT can be used interchangeably with standard-dose enhanced CT for nodule classification.
Keyword
Figure
Reference
-
1. MacMahon H, Naidich DP, Goo JM, Lee KS, Leung AN, Mayo JR, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology. 2017; 284:228–243. PMID: 28240562.2. American College of Radiology. Lung CT screening reporting and data system (Lung-RADS). Accessed Apr 11, 2017. Web site. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads.3. National Lung Screening Trial Research Team. Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011; 365:395–409. PMID: 21714641.
Article4. Jacobs C, van Rikxoort EM, Scholten ET, de Jong PA, Prokop M, Schaefer-Prokop C, et al. Solid, part-solid, or non-solid?: classification of pulmonary nodules in low-dose chest computed tomography by a computer-aided diagnosis system. Invest Radiol. 2015; 50:168–173. PMID: 25478740.5. van Riel SJ, Sanchez CI, Bankier AA, Naidich DP, Verschakelen J, Scholten ET, et al. Observer variability for classification of pulmonary nodules on low-dose CT images and its effect on nodule management. Radiology. 2015; 277:863–871. PMID: 26020438.
Article6. Diederich S, Lenzen H, Windmann R, Puskas Z, Yelbuz TM, Henneken S, et al. Pulmonary nodules: experimental and clinical studies at low-dose CT. Radiology. 1999; 213:289–298. PMID: 10540674.
Article7. Gartenschläger M, Schweden F, Gast K, Westermeier T, Kauczor H, von Zitzewitz H, et al. Pulmonary nodules: detection with low-dose vs conventional-dose spiral CT. Eur Radiol. 1998; 8:609–614. PMID: 9569333.
Article8. Kim H, Park CM, Chae HD, Lee SM, Goo JM. Impact of radiation dose and iterative reconstruction on pulmonary nodule measurements at chest CT: a phantom study. Diagn Interv Radiol. 2015; 21:459–465. PMID: 26359871.
Article9. Rusinek H, Naidich DP, McGuinness G, Leitman BS, McCauley DI, Krinsky GA, et al. Pulmonary nodule detection: low-dose versus conventional CT. Radiology. 1998; 209:243–249. PMID: 9769838.
Article10. Obuchowski NA, Subhas N, Schoenhagen P. Testing for interchangeability of imaging tests. Acad Radiol. 2014; 21:1483–1489. PMID: 25300725.
Article11. Ridge CA, Yildirim A, Boiselle PM, Franquet T, Schaefer-Prokop CM, Tack D, et al. Differentiating between subsolid and solid pulmonary nodules at CT: inter- and intraobserver agreement between experienced thoracic radiologists. Radiology. 2016; 278:888–896. PMID: 26458208.
Article12. Obuchowski NA. Can electronic medical images replace hardcopy film? Defining and testing the equivalence of diagnostic tests. Stat Med. 2001; 20:2845–2863. PMID: 11568944.
Article13. Yamashiro T, Miyara T, Honda O, Kamiya H, Murata K, Ohno Y, et al. Adaptive iterative dose reduction using three dimensional processing (AIDR3D) improves chest CT image quality and reduces radiation exposure. PLoS One. 2014; 9:e105735. PMID: 25153797.
Article14. Lee SW, Kim Y, Shim SS, Lee JK, Lee SJ, Ryu YJ, et al. Image quality assessment of ultra low-dose chest CT using sinogramaffirmed iterative reconstruction. Eur Radiol. 2014; 24:817–826. PMID: 24442444.
Article15. Li B, Behrman RH. Comment on the “report of AAPM TG 204: size-specific dose estimates (SSDE) in pediatric and adult body CT examinations” [report of AAPM TG 204, 2011]. Med Phys. 2012; 39:4613–4614. author reply 4615-4616. PMID: 22830792.
Article16. Brady SL, Kaufman RA. Investigation of American Association of physicists in medicine report 204 size-specific dose estimates for pediatric CT implementation. Radiology. 2012; 265:832–840. PMID: 23093679.
Article17. McCollough C, Cody D, Edyvean S, Geise R, Gould B, Keat N, et al. The measurement, reporting, and management of radiation dose in CT. Virginia: American Association of Physicists in Medicine. 2008; 1–34.
Article18. Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner society: glossary of terms for thoracic imaging. Radiology. 2008; 246:697–722. PMID: 18195376.
Article19. MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005; 237:395–400. PMID: 16244247.
Article20. Yang Z, Zhou M. Kappa statistic for clustered matched-pair data. Stat Med. 2014; 33:2612–2633. PMID: 24532251.
Article21. Fleiss J. Measuring nominal scale agreement among many raters. Psychol Bull. 1971; 76:378–382.
Article22. Lee H, Kim B, Kim KJ, Seo J, Park S, Shin YG, et al. Introduction of heat map to fidelity assessment of compressed CT images. Med Phys. 2011; 38:4667–4671. PMID: 21928640.
Article23. Gould MK, Donington J, Lynch WR, Mazzone PJ, Midthun DE, Naidich DP, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of chest physicians evidence-based clinical practice guidelines. Chest. 2013; 143(5 Suppl):e93S–e120S. PMID: 23649456.24. Naidich DP, Bankier AA, MacMahon H, Schaefer-Prokop CM, Pistolesi M, Goo JM, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013; 266:304–317. PMID: 23070270.
Article25. Lee CT. What do we know about ground-glass opacity nodules in the lung? Transl Lung Cancer Res. 2015; 4:656–659. PMID: 26629441.26. Lee SM, Park CM, Goo JM, Lee HJ, Wi JY, Kang CH. Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology. 2013; 268:265–273. PMID: 23468575.
Article27. Sun H, Wang W. Differentiating between subsolid and solid pulmonary nodules at CT: what is our main task? Radiology. 2016; 281:976–978. PMID: 27870624.
Article28. Vardhanabhuti V, Loader RJ, Mitchell GR, Riordan RD, Roobottom CA. Image quality assessment of standard-and low-dose chest CT using filtered back projection, adaptive statistical iterative reconstruction, and novel model-based iterative reconstruction algorithms. AJR Am J Roentgenol. 2013; 200:545–552. PMID: 23436843.29. Katsura M, Matsuda I, Akahane M, Yasaka K, Hanaoka S, Akai H, et al. Model-based iterative reconstruction technique for ultralow-dose chest CT: comparison of pulmonary nodule detectability with the adaptive statistical iterative reconstruction technique. Invest Radiol. 2013; 48:206–212. PMID: 23344517.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diameter of the Solid Component in Subsolid Nodules on Low-Dose Unenhanced Chest Computed Tomography: Measurement Accuracy for the Prediction of Invasive Component in Lung Adenocarcinoma
- Evaluation of the effective dose and image quality of low-dose multi-detector CT for orthodontic treatment planning
- Dosimetric Effects of Low Dose 4D CT Using a Commercial Iterative Reconstruction on Dose Calculation in Radiation Treatment Planning: A Phantom Study
- Attenuation-Based Automatic Kilovoltage Selection and Sinogram-Affirmed Iterative Reconstruction: Effects on Radiation Exposure and Image Quality of Portal-Phase Liver CT
- Multidetector Computed Tomography for the Assessment of Adnexal Mass: Is Unenhanced CT Scan Necessary?