Korean J Radiol.
2018 Jun;19(3):508-515. 10.3348/kjr.2018.19.3.508.
Diameter of the Solid Component in Subsolid Nodules on Low-Dose Unenhanced Chest Computed Tomography: Measurement Accuracy for the Prediction of Invasive Component in Lung Adenocarcinoma
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam 13620, Korea. kyung8404@gmail.com
- 2Department of Radiology, SMG-SNU Boramae Medical Center, Seoul 07061, Korea.
- KMID: 2410822
- DOI: http://doi.org/10.3348/kjr.2018.19.3.508
Abstract
OBJECTIVE
To determine if measurement of the diameter of the solid component in subsolid nodules (SSNs) on low-dose unenhanced chest computed tomography (CT) is as accurate as on standard-dose enhanced CT in prediction of pathological size of invasive component of lung adenocarcinoma.
MATERIALS AND METHODS
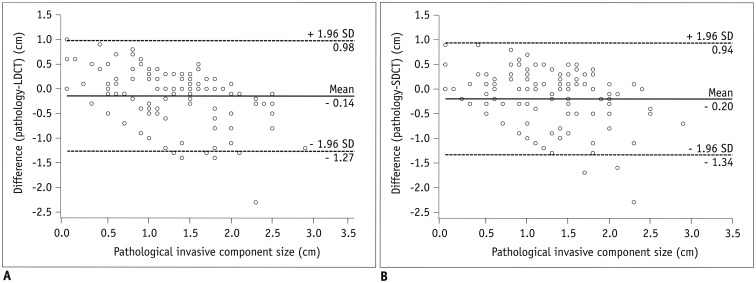
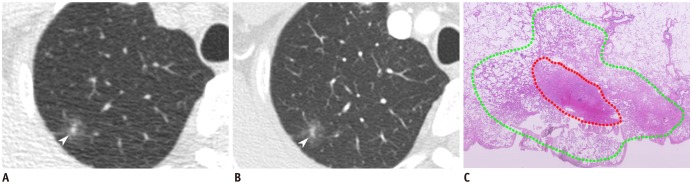
From February 2012 to October 2015, 114 SSNs were identified in 105 patients that underwent low-dose unenhanced and standard-dose enhanced CT pre-operatively. Three radiologists independently measured the largest diameter of the solid component. Intraclass correlation coefficients (ICCs) were used to assess inter-reader agreement. We estimated measurement differences between the size of solid component and that of invasive component. We measured diagnostic accuracy of the prediction of invasive adenocarcinoma using a size criterion of a solid component ≥ 6 mm, and compared them using a generalized linear mixed model.
RESULTS
Inter-reader agreement was excellent (ICC, 0.84.0.89). The mean ± standard deviation of absolute measurement differences between the solid component and invasive component was 4 ± 4 mm in low-dose unenhanced CT and 5 ± 4 mm in standard-dose enhanced CT. Diagnostic accuracy was 81.3% (95% confidence interval, 76.7.85.3%) in low-dose unenhanced CT and 76.6% (71.8.81.0%) in standard-dose enhanced CT, with no statistically significant difference (p = 0.130).
CONCLUSION
Measurement of the diameter of the solid component of SSNs on low-dose unenhanced chest CT was as accurate as on standard-dose enhanced CT for predicting the invasive component. Thus, low-dose unenhanced CT may be used safely in the evaluation of patients with SSNs.
Figure
Reference
-
1. Goo JM, Park CM, Lee HJ. Ground-glass nodules on chest CT as imaging biomarkers in the management of lung adenocarcinoma. AJR Am J Roentgenol. 2011; 196:533–543. PMID: 21343494.
Article2. Rami-Porta R, Bolejack V, Crowley J, Ball D, Kim J, Lyons G, et al. The IASLC lung cancer staging project: proposals for the revisions of the T descriptors in the forthcoming eighth edition of the TNM classification for lung cancer. J Thorac Oncol. 2015; 10:990–1003. PMID: 26134221.
Article3. Travis WD, Asamura H, Bankier AA, Beasley MB, Detterbeck F, Flieder DB, et al. The IASLC lung cancer staging project: proposals for coding T categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming eighth edition of the TNM classification of lung cancer. J Thorac Oncol. 2016; 11:1204–1223. PMID: 27107787.4. Lee HY, Choi YL, Lee KS, Han J, Zo JI, Shim YM, et al. Pure ground-glass opacity neoplastic lung nodules: histopathology, imaging, and management. AJR Am J Roentgenol. 2014; 202:W224–W233. PMID: 24555618.
Article5. Hwang EJ, Park CM, Ryu Y, Lee SM, Kim YT, Kim YW, et al. Pulmonary adenocarcinomas appearing as part-solid ground-glass nodules: is measuring solid component size a better prognostic indicator? Eur Radiol. 2015; 25:558–567. PMID: 25274618.
Article6. Zhang Y, Qiang JW, Ye JD, Ye XD, Zhang J. High resolution CT in differentiating minimally invasive component in early lung adenocarcinoma. Lung Cancer. 2014; 84:236–241. PMID: 24679953.
Article7. Austin JH, Garg K, Aberle D, Yankelevitz D, Kuriyama K, Lee HJ, et al. Radiologic implications of the 2011 classification of adenocarcinoma of the lung. Radiology. 2013; 266:62–71. PMID: 23070271.
Article8. Cohen JG, Reymond E, Lederlin M, Medici M, Lantuejoul S, Laurent F, et al. Differentiating pre- and minimally invasive from invasive adenocarcinoma using CT-features in persistent pulmonary part-solid nodules in Caucasian patients. Eur J Radiol. 2015; 84:738–744. PMID: 25623825.
Article9. Chae HD, Park CM, Park SJ, Lee SM, Kim KG, Goo JM. Computerized texture analysis of persistent part-solid ground-glass nodules: differentiation of preinvasive lesions from invasive pulmonary adenocarcinomas. Radiology. 2014; 273:285–293. PMID: 25102296.
Article10. Lee SM, Park CM, Goo JM, Lee HJ, Wi JY, Kang CH. Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology. 2013; 268:265–273. PMID: 23468575.
Article11. Lee KH, Goo JM, Park SJ, Wi JY, Chung DH, Go H, et al. Correlation between the size of the solid component on thin-section CT and the invasive component on pathology in small lung adenocarcinomas manifesting as ground-glass nodules. J Thorac Oncol. 2014; 9:74–82. PMID: 24346095.
Article12. MacMahon H, Naidich DP, Goo JM, Lee KS, Leung ANC, Mayo JR, et al. Guidelines for management of incidental pulmonary nodules detected on CT images: from the Fleischner Society 2017. Radiology. 2017; 284:228–243. PMID: 28240562.13. Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol. 2002; 178:1053–1057. PMID: 11959700.14. Kim H, Park CM, Koh JM, Lee SM, Goo JM. Pulmonary subsolid nodules: what radiologists need to know about the imaging features and management strategy. Diagn Interv Radiol. 2014; 20:47–57. PMID: 24100062.
Article15. Scholten ET, Jacobs C, van Ginneken B, van Riel S, Vliegenthart R, Oudkerk M, et al. Detection and quantification of the solid component in pulmonary subsolid nodules by semiautomatic segmentation. Eur Radiol. 2015; 25:488–496. PMID: 25287262.
Article16. Kim H, Park CM, Chae HD, Lee SM, Goo JM. Impact of radiation dose and iterative reconstruction on pulmonary nodule measurements at chest CT: a phantom study. Diagn Interv Radiol. 2015; 21:459–465. PMID: 26359871.
Article17. Li B, Behrman RH. Comment on the “report of AAPM TG 204: size-specific dose estimates (SSDE) in pediatric and adult body CT examinations” [report of AAPM TG 204, 2011]. Med Phys. 2012; 39:4613–4614. author reply 4615-4616. PMID: 22830792.
Article18. Brady SL, Kaufman RA. Investigation of American Association of Physicists in Medicine report 204 size-specific dose estimates for pediatric CT implementation. Radiology. 2012; 265:832–840. PMID: 23093679.
Article19. McCollough C, Cody D, Edyvean S, Geise R, Gould B, Keat N, et al. The measurement, reporting, and management of radiation dose in CT. Virginia: American Association of Physicists in Medicine;2008. p. 1–34.20. Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, et al. The 2015 world health organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol. 2015; 10:1243–1260. PMID: 26291008.21. de Jong PA, Leiner T, Lammers JW, Gietema HA. Can low-dose unenhanced chest CT be used for follow-up of lung nodules? AJR Am J Roentgenol. 2012; 199:777–780. PMID: 22997367.
Article22. McCollough CH, Primak AN, Braun N, Kofler J, Yu L, Christner J. Strategies for reducing radiation dose in CT. Radiol Clin North Am. 2009; 47:27–40. PMID: 19195532.
Article23. Silverman JD, Paul NS, Siewerdsen JH. Investigation of lung nodule detectability in low-dose 320-slice computed tomography. Med Phys. 2009; 36:1700–1710. PMID: 19544787.
Article24. Yu L, Liu X, Leng S, Kofler JM, Ramirez-Giraldo JC, Qu M, et al. Radiation dose reduction in computed tomography: techniques and future perspective. Imaging Med. 2009; 1:65–84. PMID: 22308169.
Article25. Hein PA, Romano VC, Rogalla P, Klessen C, Lembcke A, Bornemann L, et al. Variability of semiautomated lung nodule volumetry on ultralow-dose CT: comparison with nodule volumetry on standard-dose CT. J Digit Imaging. 2010; 23:8–17. PMID: 18773240.
Article26. Sui X, Meinel FG, Song W, Xu X, Wang Z, Wang Y, et al. Detection and size measurements of pulmonary nodules in ultra-low-dose CT with iterative reconstruction compared to low dose CT. Eur J Radiol. 2016; 85:564–570. PMID: 26860668.
Article27. Christe A, Torrente JC, Lin M, Yen A, Hallett R, Roychoudhury K, et al. CT screening and follow-up of lung nodules: effects of tube current-time setting and nodule size and density on detectability and of tube current-time setting on apparent size. AJR Am J Roentgenol. 2011; 197:623–630. PMID: 21862804.
Article28. Hein PA, Romano VC, Rogalla P, Klessen C, Lembcke A, Dicken V, et al. Linear and volume measurements of pulmonary nodules at different CT dose levels - intrascan and interscan analysis. Rofo. 2009; 181:24–31. PMID: 19085687.
Article29. Siegelman JW, Supanich MP, Gavrielides MA. Pulmonary nodules with ground-glass opacity can be reliably measured with low-dose techniques regardless of iterative reconstruction: results of a phantom study. AJR Am J Roentgenol. 2015; 204:1242–1247. PMID: 26001234.
Article30. Park HS, Lee S, Haam S, Lee GD. Effect of formalin fixation and tumour size in small-sized non-small-cell lung cancer: a prospective, single-centre study. Histopathology. 2017; 71:437–445. PMID: 28407385.
Article31. Yoo RE, Goo JM, Hwang EJ, Yoon SH, Lee CH, Park CM, et al. Retrospective assessment of interobserver agreement and accuracy in classifications and measurements in subsolid nodules with solid components less than 8mm: which window setting is better? Eur Radiol. 2017; 27:1369–1376. PMID: 27456963.
Article32. Mao H, Labh K, Han F, Jiang S, Yang Y, Sun X. Diagnosis of the invasiveness of lung adenocarcinoma manifesting as ground glass opacities on high-resolution computed tomography. Thorac Cancer. 2016; 7:129–135. PMID: 26816547.
Article33. Collins J, Stern EJ. Ground-glass opacity at CT: the ABCs. AJR Am J Roentgenol. 1997; 169:355–367. PMID: 9242736.
Article34. Goodman LR, Gulsun M, Washington L, Nagy PG, Piacsek KL. Inherent variability of CT lung nodule measurements in vivo using semiautomated volumetric measurements. AJR Am J Roentgenol. 2006; 186:989–994. PMID: 16554568.
Article35. Cohen JG, Goo JM, Yoo RE, Park SB, van Ginneken B, Ferretti GR, et al. The effect of late-phase contrast enhancement on semi-automatic software measurements of CT attenuation and volume of part-solid nodules in lung adenocarcinomas. Eur J Radiol. 2016; 85:1174–1180. PMID: 27161068.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pulmonary Subsolid Nodules: An Overview & Management Guidelines
- Nodule Classification on Low-Dose Unenhanced CT and Standard-Dose Enhanced CT: Inter-Protocol Agreement and Analysis of Interchangeability
- Semi-Quantitative Analysis for Determining the Optimal Threshold Value on CT to Measure the Solid Portion of Pulmonary Subsolid Nodules
- Detection of Pulmonary Metastatic Nodules: Usefulness of Low-dose Multidetector CT in Comparison with Chest Radiograph
- Effect of the High-Pitch Mode in Dual-Source Computed Tomography on the Accuracy of Three-Dimensional Volumetry of Solid Pulmonary Nodules: A Phantom Study