Ann Rehabil Med.
2014 Apr;38(2):263-268.
Concomitant Occurrence of Cervical Myelopathy, Cerebral Infarction, and Peripheral Neuropathy in Systemic Lupus Erythematosus: A Case Report
- Affiliations
-
- 1Department of Rehabilitation Medicine, Ewha Womans University School of Medicine, Seoul, Korea. yoonreha@ewha.ac.kr
Abstract
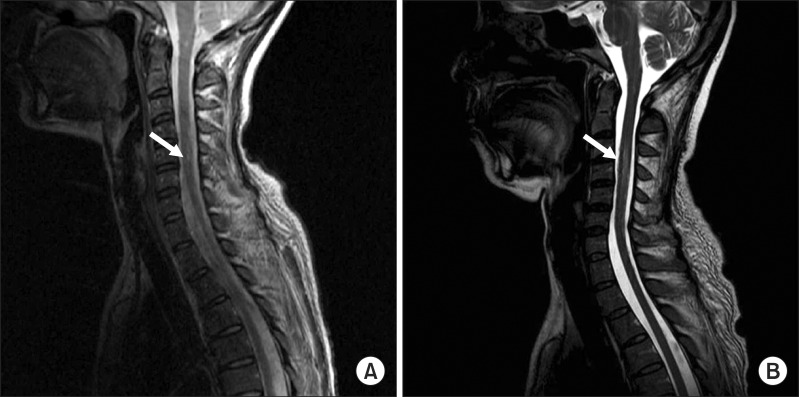
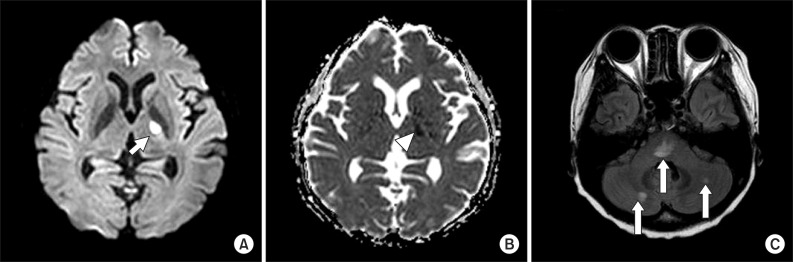
- Systemic lupus erythematosus (SLE) is an autoimmune connective tissue disease characterized by multiorgan involvement with diverse clinical presentations. Central nervous system involvement in neuropsychiatric syndromes of SLE (NPSLE), such as cerebrovascular disease and myelopathy, is a major cause of morbidity and mortality in SLE patients. The concomitant occurrence of myelopathy, cerebrovascular disease, and peripheral neuropathy in a patient with SLE has not yet been reported. We report on a 41-year-old woman with SLE who showed motor and sensory impairment with urinary retention and was diagnosed with cervical myelopathy and acute cerebral infarction by spine and brain magnetic resonance imaging and peripheral neuropathy by electrodiagnostic examination. Even though pathogenesis of NPSLE is not well elucidated, we assume that increased antibodies of anti-double stranded DNA (anti-dsDNA), presence of lupus anticoagulant and hypertension are risk factors that have caused neuropsychiatric lupus in this patient.
MeSH Terms
-
Adult
Antibodies
Brain
Central Nervous System
Cerebral Infarction*
Connective Tissue Diseases
DNA
Female
Humans
Hypertension
Lupus Coagulation Inhibitor
Lupus Erythematosus, Systemic*
Magnetic Resonance Imaging
Mortality
Peripheral Nervous System Diseases*
Risk Factors
Spinal Cord Diseases*
Spine
Urinary Retention
Antibodies
DNA
Lupus Coagulation Inhibitor
Figure
Reference
-
1. Park SH. Systemic lupus erythematosus. J Korean Med Assoc. 2009; 52:645–656.
Article2. American College of Rheumatology. The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum. 1999; 42:599–608. PMID: 10211873.3. van Dam AP. Diagnosis and pathogenesis of CNS lupus. Rheumatol Int. 1991; 11:1–11. PMID: 1866569.
Article4. Futrell N, Millikan C. Frequency, etiology, and prevention of stroke in patients with systemic lupus erythematosus. Stroke. 1989; 20:583–591. PMID: 2718197.
Article5. Łukjanowicz M, Brzosko M. Myelitis in the course of systemic lupus erythematosus: review. Pol Arch Med Wewn. 2009; 119:67–72. PMID: 19341181.
Article6. Florica B, Aghdassi E, Su J, Gladman DD, Urowitz MB, Fortin PR. Peripheral neuropathy in patients with systemic lupus erythematosus. Semin Arthritis Rheum. 2011; 41:203–211. PMID: 21641018.
Article7. Stahl HD, Ettlin TH, Plohmann A, Radu EW, Muller-Brand J, Steiger U, et al. Central nervous system lupus: concomitant occurrence of myelopathy and cognitive dysfunction. Clin Rheumatol. 1994; 13:273–279. PMID: 8088073.8. Govoni M, Bombardieri S, Bortoluzzi A, Caniatti L, Casu C, Conti F, et al. Factors and comorbidities associated with first neuropsychiatric event in systemic lupus erythematosus: does a risk profile exist? A large multicentre retrospective cross-sectional study on 959 Italian patients. Rheumatology (Oxford). 2012; 51:157–168. PMID: 22075066.
Article9. Liveson JA, Ma DM. Laboratory reference for clinical neurophysiology. Philadelphia, PA: F.A. Davis;1992.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Ruptured Aneurysm in a Patient with Systemic Lupus Erythematosus: Case Report
- Intractable Progressive Cerebral Infarction with Multiple Atypical Aneurysms in Systemic Lupus Erythematosus
- A Case of Neurogenic Bladder Associated with Systemic Lupus Erythematosus
- A Case of Transverse Myelitis as a First Manifestation of Systemic Lupus Erythematosus
- A Case of Generalized Pustular Psoriasis Associated with Systemic Lupus Erythematosus