Endocrinol Metab.
2017 Dec;32(4):442-450. 10.3803/EnM.2017.32.4.442.
Changes in Body Composition According to Age and Sex among Young Non-Diabetic Korean Adults: the Kangbuk Samsung Health Study
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. hongsiri@hanmail.net
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea.
- 3Department of Neurology, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea.
- KMID: 2406188
- DOI: http://doi.org/10.3803/EnM.2017.32.4.442
Abstract
- BACKGROUND
Age-related decreases in lean mass represent a serious health problem. We aimed to analyze the risks of rapid decreases in lean mass by age and sex in relatively young Korean adults during a 4-year follow-up study.
METHODS
A total of 65,856 non-diabetic participants (59.5% men, mean age 39.1 years) in a health screening program were subjected to bioimpedance body composition analyses and metabolic parameter analyses at baseline and after 4 years. The participants were sub-divided according to age, and additionally to six groups by age and the degree of body weight change over the 4-year period. The actual changes in body weight, lean mass, and fat mass and the percent changes over the 4-year period were assessed.
RESULTS
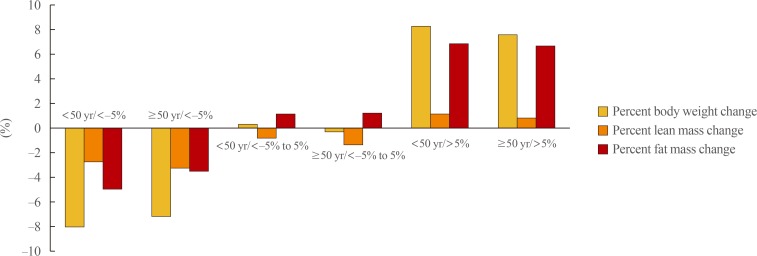
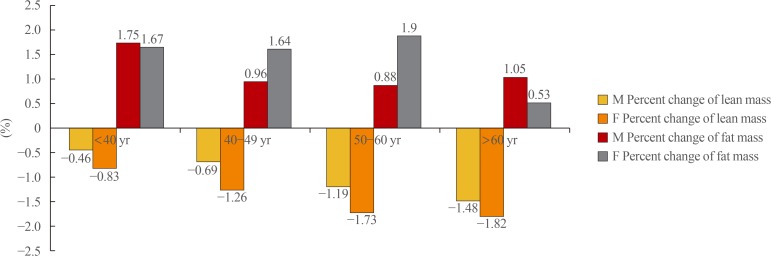
The percent change in lean mass decreased and the percent change of fat mass increased with increasing age in every age and sex group. However, the annual percent decrease in lean mass and percent increase in fat mass were significantly higher among women than among men (−0.26% vs. −0.15% and 0.34% vs. 0.42%, respectively; P<0.01). Participants who were older than 50 years and had a weight loss <−5% during the 4 years had significantly greater decreases in lean mass and smaller decreases in fat mass, compared to those who were younger than 50 years. An odds ratio analysis to determine the lowest quartile of the percent change in lean mass according to age group revealed that participants older than 60 years had a significantly increased risk of a rapid decrease in the lean mass percentage (2.081; 95% confidence interval, 1.678 to 2.581).
CONCLUSION
Even in this relatively young study population, the lean mass decreased significantly with age, and the risk of a rapid decrease in lean mass was higher among women than among men. Furthermore, the elderly exhibited a significantly more rapid decrease in lean mass, compared with younger participants.
Keyword
MeSH Terms
Figure
Reference
-
1. World Health Organization. Obesity and overweight [Internet]. Geneva: World Health Organization;c2017. cited 2017 Oct 19. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/.2. Garthe I, Raastad T, Sundgot-Borgen J. Long-term effect of nutritional counselling on desired gain in body mass and lean body mass in elite athletes. Appl Physiol Nutr Metab. 2011; 36:547–554. PMID: 21851204.
Article3. Seo MH, Rhee EJ. Metabolic and cardiovascular implications of a metabolically healthy obesity phenotype. Endocrinol Metab (Seoul). 2014; 29:427–434. PMID: 25559571.
Article4. Kang YM, Jung CH, Cho YK, Jang JE, Hwang JY, Kim EH, et al. Visceral adiposity index predicts the conversion of metabolically healthy obesity to an unhealthy phenotype. PLoS One. 2017; 12:e0179635. PMID: 28644850.
Article5. Choi KM. Sarcopenia and sarcopenic obesity. Endocrinol Metab (Seoul). 2013; 28:86–89. PMID: 24396659.
Article6. Newman AB, Yanez D, Harris T, Duxbury A, Enright PL, Fried LP, et al. Weight change in old age and its association with mortality. J Am Geriatr Soc. 2001; 49:1309–1318. PMID: 11890489.
Article7. Newman AB, Lee JS, Visser M, Goodpaster BH, Kritchevsky SB, Tylavsky FA, et al. Weight change and the conservation of lean mass in old age: the Health, Aging and Body Composition Study. Am J Clin Nutr. 2005; 82:872–878. PMID: 16210719.
Article8. Arnold AM, Newman AB, Cushman M, Ding J, Kritchevsky S. Body weight dynamics and their association with physical function and mortality in older adults: the Cardiovascular Health Study. J Gerontol A Biol Sci Med Sci. 2010; 65:63–70. PMID: 19386574.
Article9. Williamson DF, Pamuk ER. The association between weight loss and increased longevity. A review of the evidence. Ann Intern Med. 1993; 119(7 Pt 2):731–736. PMID: 8363207.
Article10. Allen TH, Anderson EC, Langham WH. Total body potassium and gross body composition in relation to age. J Gerontol. 1960; 15:348–357. PMID: 13682553.
Article11. Pierson RN Jr, Lin DH, Phillips RA. Total-body potassium in health: effects of age, sex, height, and fat. Am J Physiol. 1974; 226:206–212. PMID: 4809882.12. Borkan GA, Norris AH. Fat redistribution and the changing body dimensions of the adult male. Hum Biol. 1977; 49:495–513. PMID: 892769.13. Chumlea WC, Garry PJ, Hunt WC, Rhyne RL. Distributions of serial changes in stature and weight in a healthy elderly population. Hum Biol. 1988; 60:917–925. PMID: 3235081.14. Roberts SB, Fuss P, Heyman MB, Evans WJ, Tsay R, Rasmussen H, et al. Control of food intake in older men. JAMA. 1994; 272:1601–1606. PMID: 7966871.
Article15. Visser M, Pahor M, Tylavsky F, Kritchevsky SB, Cauley JA, Newman AB, et al. One- and two-year change in body composition as measured by DXA in a population-based cohort of older men and women. J Appl Physiol (1985). 2003; 94:2368–2374. PMID: 12598481.16. Hughes VA, Frontera WR, Roubenoff R, Evans WJ, Singh MA. Longitudinal changes in body composition in older men and women: role of body weight change and physical activity. Am J Clin Nutr. 2002; 76:473–481. PMID: 12145025.
Article17. Karvonen-Gutierrez C, Kim C. Association of mid-life changes in body size, body composition and obesity status with the menopausal transition. Healthcare (Basel). 2016; 4:E42. PMID: 27417630.
Article18. Lovejoy JC, Champagne CM, de Jonge L, Xie H, Smith SR. Increased visceral fat and decreased energy expenditure during the menopausal transition. Int J Obes (Lond). 2008; 32:949–958. PMID: 18332882.
Article19. Wellons M, Ouyang P, Schreiner PJ, Herrington DM, Vaidya D. Early menopause predicts future coronary heart disease and stroke: the Multi-Ethnic Study of Atherosclerosis. Menopause. 2012; 19:1081–1087. PMID: 22692332.20. Chen H, Bermudez OI, Tucker KL. Waist circumference and weight change are associated with disability among elderly Hispanics. J Gerontol A Biol Sci Med Sci. 2002; 57:M19–M25. PMID: 11773208.
Article21. Houston DK, Stevens J, Cai J, Morey MC. Role of weight history on functional limitations and disability in late adulthood: the ARIC study. Obes Res. 2005; 13:1793–1802. PMID: 16286527.
Article22. Lee JS, Kritchevsky SB, Tylavsky F, Harris T, Simonsick EM, Rubin SM, et al. Weight change, weight change intention, and the incidence of mobility limitation in well-functioning community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2005; 60:1007–1012. PMID: 16127104.
Article23. Launer LJ, Harris T, Rumpel C, Madans J. Body mass index, weight change, and risk of mobility disability in middle-aged and older women. The epidemiologic follow-up study of NHANES I. JAMA. 1994; 271:1093–1098. PMID: 8151851.
Article24. American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care. 2017; 40(Suppl 1):S11–S24. PMID: 27979889.25. Wang H, Hai S, Cao L, Zhou J, Liu P, Dong BR. Estimation of prevalence of sarcopenia by using a new bioelectrical impedance analysis in Chinese community-dwelling elderly people. BMC Geriatr. 2016; 16:216. PMID: 28031025.
Article26. Gibson AL, Holmes JC, Desautels RL, Edmonds LB, Nuudi L. Ability of new octapolar bioimpedance spectroscopy analyzers to predict 4-component-model percentage body fat in Hispanic, black, and white adults. Am J Clin Nutr. 2008; 87:332–338. PMID: 18258622.
Article27. Kyle UG, Genton L, Karsegard L, Slosman DO, Pichard C. Single prediction equation for bioelectrical impedance analysis in adults aged 20: 94 years. Nutrition. 2001; 17:248–253. PMID: 11312069.28. Forbes GB. Longitudinal changes in adult fat-free mass: influence of body weight. Am J Clin Nutr. 1999; 70:1025–1031. PMID: 10584047.
Article29. Williamson DF. Descriptive epidemiology of body weight and weight change in U.S. adults. Ann Intern Med. 1993; 119(7 Pt 2):646–649. PMID: 8363190.30. Brown JC, Harhay MO, Harhay MN. Sarcopenia and mortality among a population-based sample of community-dwelling older adults. J Cachexia Sarcopenia Muscle. 2016; 7:290–298. PMID: 27239410.
Article31. Roshanravan B, Patel KV, Fried LF, Robinson-Cohen C, de Boer IH, Harris T, et al. Association of muscle endurance, fatigability, and strength with functional limitation and mortality in the health aging and body composition study. J Gerontol A Biol Sci Med Sci. 2017; 72:284–291. PMID: 27907890.
Article32. Verschueren S, Gielen E, O'Neill TW, Pye SR, Adams JE, Ward KA, et al. Sarcopenia and its relationship with bone mineral density in middle-aged and elderly European men. Osteoporos Int. 2013; 24:87–98. PMID: 22776861.
Article33. Mauvais-Jarvis F. Sex differences in metabolic homeostasis, diabetes, and obesity. Biol Sex Differ. 2015; 6:14. PMID: 26339468.
Article34. Heitmann BL, Garby L. Composition (lean and fat tissue) of weight changes in adult Danes. Am J Clin Nutr. 2002; 75:840–847. PMID: 11976157.
Article35. Poehlman ET, Toth MJ, Gardner AW. Changes in energy balance and body composition at menopause: a controlled longitudinal study. Ann Intern Med. 1995; 123:673–675. PMID: 7574222.36. Aloia JF, McGowan DM, Vaswani AN, Ross P, Cohn SH. Relationship of menopause to skeletal and muscle mass. Am J Clin Nutr. 1991; 53:1378–1383. PMID: 2035465.
Article37. Aloia JF, Vaswani A, Russo L, Sheehan M, Flaster E. The influence of menopause and hormonal replacement therapy on body cell mass and body fat mass. Am J Obstet Gynecol. 1995; 172:896–900. PMID: 7892882.38. Sorensen MB, Rosenfalck AM, Hojgaard L, Ottesen B. Obesity and sarcopenia after menopause are reversed by sex hormone replacement therapy. Obes Res. 2001; 9:622–626. PMID: 11595778.39. Chen Z, Bassford T, Green SB, Cauley JA, Jackson RD, LaCroix AZ, et al. Postmenopausal hormone therapy and body composition: a substudy of the estrogen plus progestin trial of the Women's Health Initiative. Am J Clin Nutr. 2005; 82:651–656. PMID: 16155280.40. Souza VA, Oliveira D, Barbosa SR, Correa JODA, Colugnati FAB, Mansur HN, et al. Sarcopenia in patients with chronic kidney disease not yet on dialysis: analysis of the prevalence and associated factors. PLoS One. 2017; 12:e0176230. PMID: 28448584.
Article41. Han E, Lee YH, Kim G, Kim SR, Lee BW, Kang ES, et al. Sarcopenia is associated with albuminuria independently of hypertension and diabetes: KNHANES 2008-2011. Metabolism. 2016; 65:1531–1540. PMID: 27621188.
Article42. Solheim TS, Blum D, Fayers PM, Hjermstad MJ, Stene GB, Strasser F, et al. Weight loss, appetite loss and food intake in cancer patients with cancer cachexia: three peas in a pod?: analysis from a multicenter cross sectional study. Acta Oncol. 2014; 53:539–546. PMID: 23998647.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Body Composition Analysis in Newly Diagnosed Diabetic Adolescent Girls
- The Prevalence of Vitreoretinal Diseases in a Screened Korean Population 50 Years and Older
- Response: The Relationship of Body Composition and Coronary Artery Calcification in Apparently Healthy Korean Adults (Endocrinol Metab 2013;28:33-40, Jung-Hee Yu et al.)
- Body Composition Changes in Korean Children and Adolescents
- The Effect of Regular Exercise Program on Body Composition and Body Image in Adults Using One Fitness Center