J Korean Neurosurg Soc.
2018 Jan;61(1):114-119. 10.3340/jkns.2017.0202.004.
Posterior Screw Fixation in Previously Augmented Vertebrae with Bone Cement: Is It Inapplicable?
- Affiliations
-
- 1Department of Neurosurgery, Chosun University College of Medicine, Gwangju, Korea. chosunns@chosun.ac.kr
- KMID: 2403531
- DOI: http://doi.org/10.3340/jkns.2017.0202.004
Abstract
OBJECTIVE
The purpose of this study was to determine the feasibility of screw fixation in previously augmented vertebrae with bone cement. We also investigated the influence of cement distribution pattern on the surgical technique.
METHODS
Fourteen patients who required screw fixation at the level of the previous percutaneous vertebroplasty or balloon kyphoplasty were enrolled in this study. The indications for screw fixation in the previously augmented vertebrae with bone cement included delayed complications, such as cement dislodgement, cement leakage with neurologic deficits, and various degenerative spinal diseases, such as spondylolisthesis or foraminal stenosis. Clinical outcomes, including pain scale scores, cement distribution pattern, and procedure-related complications were assessed.
RESULTS
Three patients underwent posterior screw fixation in previously cemented vertebrae due to cement dislodgement or progressive kyphosis. Three patients required posterior screw fixation for cement leakage or displacement of fracture fragments with neurologic deficits. Eight patients underwent posterior screw fixation due to various degenerative spinal diseases. It was possible to insert screws in the previously augmented vertebrae regardless of the cement distribution pattern; however, screw insertion was more difficult and changed directions in the patients with cemented vertebrae exhibiting a solid pattern rather than a trabecular pattern. All patients showed significant improvements in pain compared with the preoperative levels, and no patient experienced neurologic deterioration as seen at the final follow-up.
CONCLUSION
For patients with vertebrae previously augmented with bone cement, posterior screw fixation is not a contraindication, but is a feasible option.
Keyword
MeSH Terms
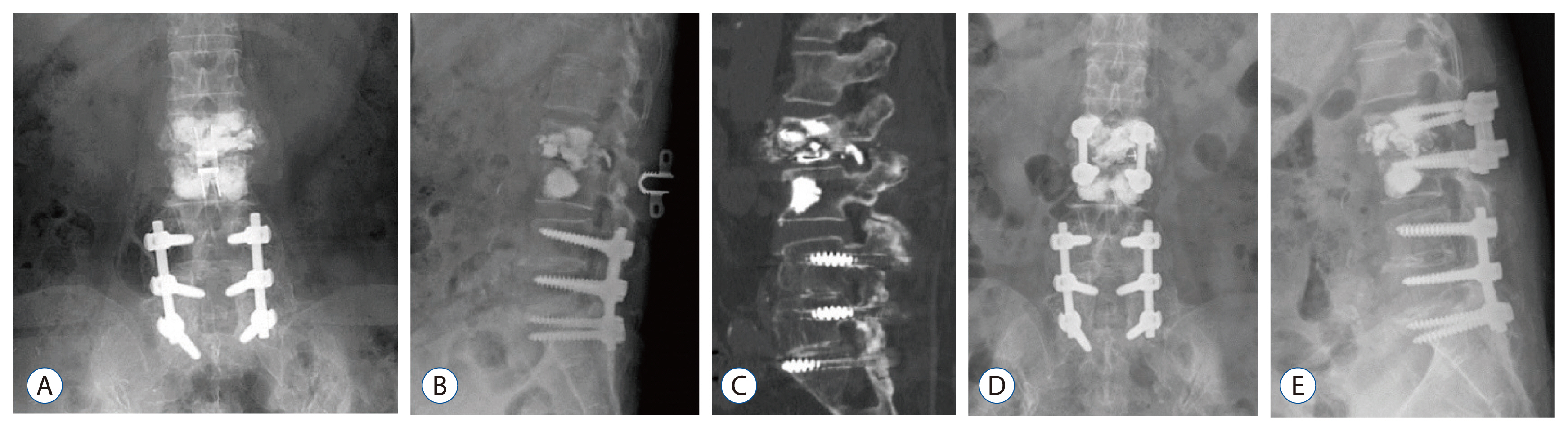
Figure
Reference
-
References
1. Graham J, Ahn C, Hai N, Buch BD. Effect of bone density on vertebral strength and stiffness after percutaneous vertebroplasty. Spine (Phila Pa 1976). 32:505–511. 2007.
Article2. Ha KY, Kim YH, Chang DG, Son IN, Kim KW, Kim SE. Causes of late revision surgery after bone cement augmentation in osteoporotic vertebral compression fractures. Asian Spine J. 7:294–300. 2013.
Article3. Jung HJ, Kim SW, Ju CI, Kim SH, Kim HS. Bone cement-augmented short segment fixation with percutaneous screws for thoracolumbar burst fractures accompanied by severe osteoporosis. J Korean Neurosurg Soc. 52:353–358. 2012.
Article4. Kim HS, Kim SH, Ju CI, Kim SW, Lee SM, Shin H. The role of bone cement augmentation in the treatment of chronic symptomatic osteoporotic compression fracture. J Korean Neurosurg Soc. 48:490–495. 2010.
Article5. Kim HS, Park SK, Joy H, Ryu JK, Kim SW, Ju CI. Bone cement augmentation of short segment fixation for unstable burst fracture in severe osteoporosis. J Korean Neurosurg Soc. 44:8–14. 2008.
Article6. Lee K, Lee SG, Kim WK, Yoo CJ, Park CW. Comparison vertebroplasty with kyphoplasty in delayed post-traumatic osteonecrosis of a vertebral body(kummell’s disease). Korean J Spine. 5:70–76. 2008.7. Oka M, Matsusako M, Kobayashi N, Uemura A, Numaguchi Y. Intravertebral cleft sign on fat-suppressed contrast-enhanced MR: correlation with cement distribution pattern on percutaneous vertebroplasty. Acad Radiol. 12:992–999. 2005.8. Trout AT, Kallmes DF, Lane JI, Layton KF, Marx WF. Subsequent vertebral fractures after vertebroplasty: association with intraosseous clefts. AJNR Am J Neuroradiol. 27:1586–1591. 2006.9. Wang HS, Kim HS, Ju CI, Kim SW. Delayed bone cement displacement following balloon kyphoplasty. J Korean Neurosurg Soc. 43:212–214. 2008.
Article10. Yang SC, Chen WJ, Yu SW, Tu YK, Kao YH, Chung KC. Revision strategies for complications and failure of vertebroplasties. Eur Spine J. 17:982–988. 2008.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cardiac Perforation Caused by Bone Cements as a Complication of Cement Augmented Pedicle Screw Fixation Using the Fenestrated Pedicle Screw: A Case Report
- Clinical Efficacy of Bone Cement Augmented Screw Fixation for the Severe Osteoporotic Spine
- Cement-Augmented Pedicle Screw Fixation in Patients with Osteoporosis : Safety, Efficacy and Complications
- Clinical Effects and Complications of Pedicle Screw Augmentation with Bone Cement: Comparison of Fenestrated Screw Augmentation and Vertebroplasty Augmentation
- Bone Cement Augmented Screw Fixation for Severe Osteoporotic Spine: Large Series of Clinical Application