Intest Res.
2018 Jan;16(1):147-150. 10.5217/ir.2018.16.1.147.
A case of pemphigus vulgaris associated with ulcerative colitis
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea. neakker@gmail.com
- 2Department of Dermatology, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- 3Department of Pathology, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea.
- KMID: 2402659
- DOI: http://doi.org/10.5217/ir.2018.16.1.147
Abstract
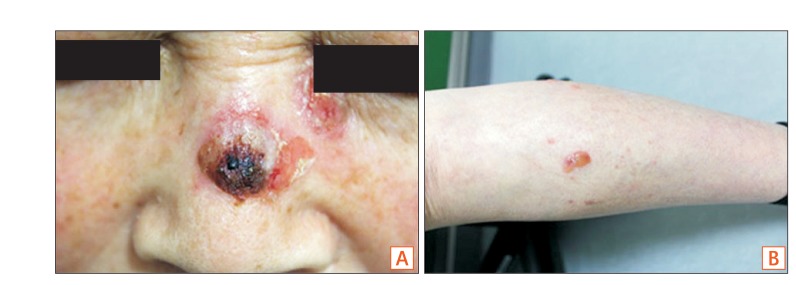
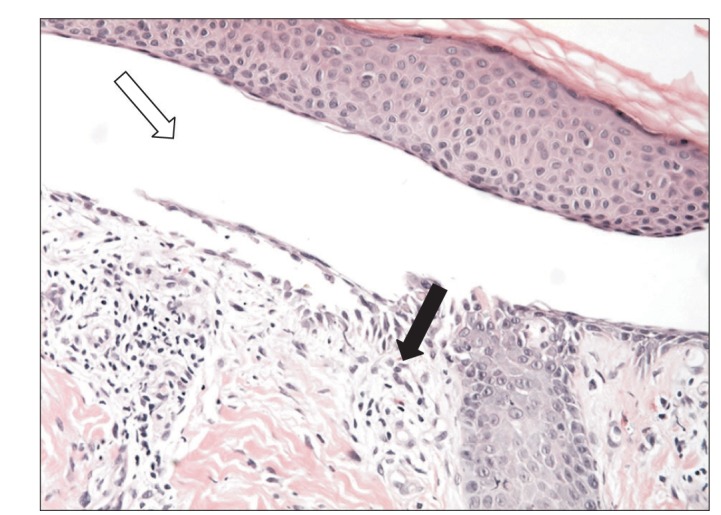
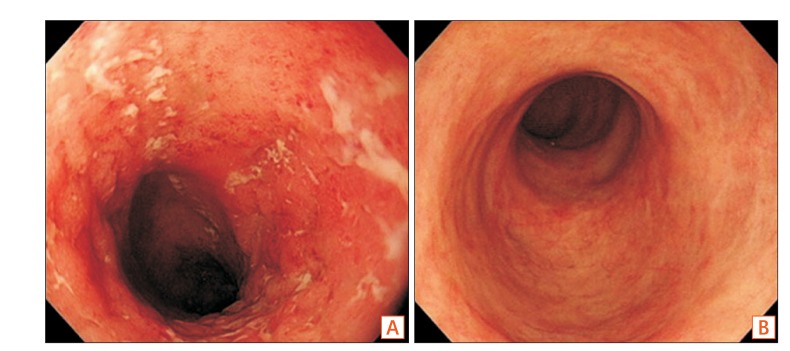
- Pemphigus vulgaris is an autoimmune bullous disorder characterized by the production of autoantibodies against the intercellular space of the epithelium. It has rarely been reported in association with inflammatory bowel disease. Ulcerative colitis is one of the forms of inflammatory bowel disease. A 62-year-old woman who had been treated for ulcerative colitis for 16 years developed pruritic bullae on the skin of her face and body. Histological findings and direct immunofluorescence examination of the skin showed pemphigus vulgaris. She was treated with systemic steroids, mesalazine, and azathioprine. Her cutaneous lesions have remained in remission and her ulcerative colitis has remained well-controlled. The relationship between pemphigus vulgaris and ulcerative colitis is unclear. An autoimmune response has been suspected in the pathogenesis of ulcerative colitis. Pemphigus vulgaris is also associated with an autoimmune mechanism. To our knowledge, this is the first case of ulcerative colitis associated with pemphigus vulgaris reported in Korea. The association may be causal.
Keyword
MeSH Terms
Figure
Reference
-
1. Mihai S, Sitaru C. Immunopathology and molecular diagnosis of autoimmune bullous diseases. J Cell Mol Med. 2007; 11:462–481. PMID: 17521373.
Article2. Areias E, Garcia e. Cutaneous manifestations of ulcerative colitis. Med Cutan Ibero Lat Am. 1987; 15:185–197. PMID: 3312861.3. Timani S, Mutasim DF. Skin manifestations of inflammatory bowel disease. Clin Dermatol. 2008; 26:265–273. PMID: 18640523.
Article4. Kneisel A, Hertl M. Autoimmune bullous skin diseases. Part 1: clinical manifestations. J Dtsch Dermatol Ges. 2011; 9:844–856. PMID: 21955378.
Article5. Amagai M. Pemphigus vulgaris. In : Bolognia J, Jorizzo J, Schaffer J, editors. Dermatology. Volume 1:3rd ed. London: Elsevier;2012. p. 461–474.6. Pemphigus: current concepts. Ann Intern Med. 1980; 92:396–405. PMID: 6986830.7. Prendiville JS, Israel DM, Wood WS, Dimmick JE. Oral pemphigus vulgaris associated with inflammatory bowel disease and herpetic gingivostomatitis in an 11-year-old girl. Pediatr Dermatol. 1994; 11:145–150. PMID: 8041655.
Article8. Delfino M, Suppa F, Piccirillo A. Pemphigus vulgaris and ulcerative colitis. Dermatologica. 1986; 172:230.9. Fabbri P, Emmi L, Vignoli L, et al. Chronic pemphigus vulgaris associated with ulcerative rectocolitis: apropos of a clinical case. G Ital Dermatol Venereol. 1986; 121:355–359. PMID: 3539774.10. Kacar S, Sezgin O, Sahin T. Pemphigus vulgaris and ulcerative colitis. Am J Gastroenterol. 2002; 97:507–508. PMID: 11866312.
Article11. Chams-Davatchi C, Esmaili N, Daneshpazhooh M, et al. Randomized controlled open-label trial of four treatment regimens for pemphigus vulgaris. J Am Acad Dermatol. 2007; 57:622–628. PMID: 17583373.
Article12. Levine JS, Burakoff R. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2011; 7:235–241. PMID: 21857821.13. Huang BL, Chandra S, Shih DQ. Skin manifestations of inflammatory bowel disease. Front Physiol. 2012; 3:13. PMID: 22347192.
Article14. Sotiriou MC, Foo CW, Scholes CT, Zone JJ. Immunobullous disease and ulcerative colitis: a case series of six patients. Br J Dermatol. 2015; 173:792–796. PMID: 25913891.
Article15. Nico MM, Hussein TP, Aoki V, Lourenço SV. Pyostomatitis vegetans and its relation to inflammatory bowel disease, pyoderma gangrenosum, pyodermatitis vegetans, and pemphigus. J Oral Pathol Med. 2012; 41:584–588. PMID: 22563766.
Article16. Watchorn RE, Ma S, Gulmann C, Keogan M, O'Kane M. Linear IgA disease associated with ulcerative colitis: the role of surgery. Clin Exp Dermatol. 2014; 39:327–329. PMID: 24635071.
Article17. Chan LS, Vanderlugt CJ, Hashimoto T, et al. Epitope spreading: lessons from autoimmune skin diseases. J Invest Dermatol. 1998; 110:103–109. PMID: 9457902.
Article18. Sachsenberg-Studer EM, Runne U, Wehrmann T, et al. Bullous colon lesions in a patient with bullous pemphigoid. Gastrointest Endosc. 2001; 54:104–108. PMID: 11427857.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Pemphigus Vulgaris
- Persistent Pemphigus Vulgaris Showing Features of Tufted Hair Folliculitis
- A Case of Cytomegalvirus Colitis Developed during the Treatment of Ulcerative Colitis
- Concurrent Bullous Pemphigoid and Pemphigus Vulgaris
- Normal Anagen Effluvium as the Presenting Sign of Pemphigus Vulgaris: a Case Report