J Dent Rehabil Appl Sci.
2017 Jun;33(2):88-96. 10.14368/jdras.2017.33.2.88.
Effect of repeated learning for two dental CAD software programs
- Affiliations
-
- 1Department of Dental Science, Graduate School, Kyungpook National University, Daegu, Republic of Korea. kblee@knu.ac.kr
- 2Advanced Dental Device Development Institute, Kyungpook National University, Daegu, Republic of Korea.
- 3Department of Prosthodontics, School of Dentistry, Kyungpook National University, Daegu, Republic of Korea.
- KMID: 2388014
- DOI: http://doi.org/10.14368/jdras.2017.33.2.88
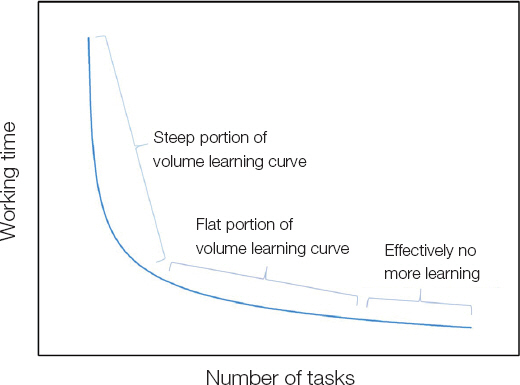
Abstract
- PURPOSE
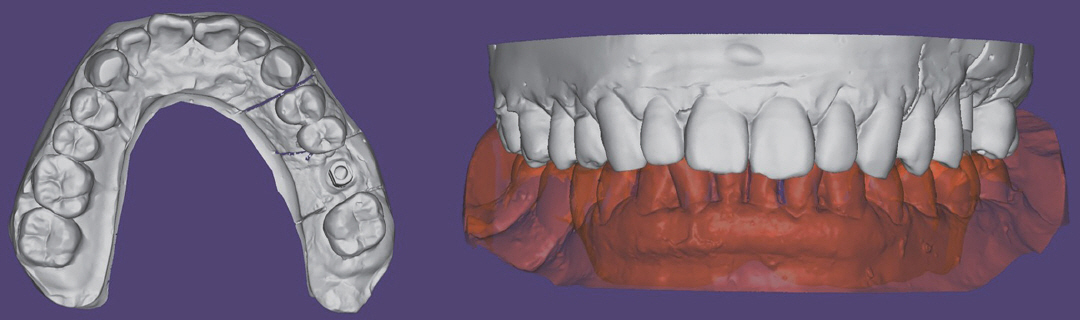
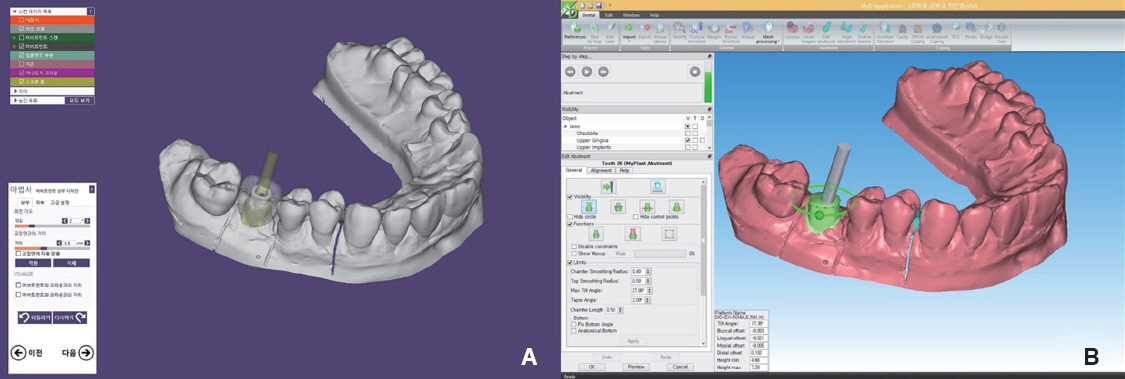
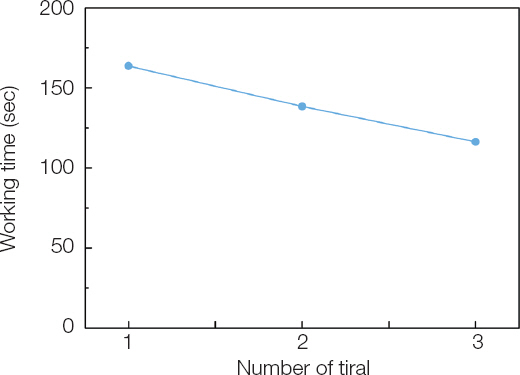
The purpose of this study is to assess the relationship between the time spent designing custom abutments and repeated learning using dental implant computer aided design (CAD) software.
MATERIALS AND METHODS
The design of customized abutments was performed four stages using the 3DS CAD software and the EXO CAD software, and measured repeatedly three times by each stage. Learning effect by repetition was presented with the learning curve, and the significance of the reduction in the total time and the time at each stage spent on designing was evaluated using the Friedman test and the Wilcoxon signed rank test. The difference in the design time between groups was analyzed using the repeated measure two-way ANOVA. Statistical analysis was performed using the SPSS statistics software (P < 0.05).
RESULTS
Repeated learning of the customized abutment design displayed a significant difference according to the number of repetition and the stage (P < 0.001). The difference in the time spent designing was found to be significant (P < 0.001), and that between the CAD software programs was also significant (P = 0.006).
CONCLUSION
Repeated learning of CAD software shortened the time spent designing. While less design time on average was spent with the 3DS CAD than with the EXO CAD, the EXO CAD showed better results in terms of learning rate according to learning effect.
Figure
Cited by 1 articles
-
Effect of abutment superimposition process of dental model scanner on final virtual model
Beom-Young Yu, Keunbada Son, Kyu-Bok Lee
J Korean Acad Prosthodont. 2019;57(3):203-210. doi: 10.4047/jkap.2019.57.3.203.
Reference
-
References
1. Duret F, Preston JD. CAD/CAM imaging in dentistry. Curr Opin Dent. 1991; 1:150–4.2. Duret F, Blouin JL, Duret B. CAD-CAM in dentistry. J Am Dent Assoc. 1988; 117:715–20. DOI: 10.14219/jada.archive.1988.0096. PMID: 3058771.3. Park JH, Kim JE, Shim JS. Digital workflow for a dental prosthesis that considers lateral mandibular relation. J Prosthet Dent. 2017; 117:340–4. DOI: 10.1016/j.prosdent.2016.07.034. PMID: 28341253.4. Lee JJ. Relationship of dental stone properties and margins setting in CAD system. updated 2017 May 9. Available from: http://www.riss.kr/search/detail/DetailView.do?p_mat_type=b.e54d9b8bc7cdb09&control_no=3a8f324dac3261eaff.e0bdc3ef48d419.5. Lewis S, Beumer J 3rd, Hornburg W, Moy P. The“UCLA” abutment. Int J Oral Maxillofac Implants. 1988; 3:183–9.6. Duke ES. The status of CAD/CAM in restorative dentistry. Compend Contin Educ Dent. 2001; 22:968–72.7. Kim HE, Cho IH. Stress analysis and fatigue failure of prefabricated and customized abutments of dental implants. J Dent Rehabil Appl Sci. 2013; 29:209–23. DOI: 10.14368/jdras.2013.29.3.209.8. Rieder CE. Customized implant abutment copings to achieve biologic, mechanical, and esthetic objectives. Int J Periodontics Restorative Dent. 1996; 16:20–9.9. Heydecke G, Sierraalta M, Razzoog ME. Evolution and use of aluminum oxide single-tooth implant abutments:a short review and presentation of two cases. Int J Prosthodont. 2002; 15:488–93.10. Hong JI. A study on user’s learn ability evaluation method using learning curve model. Graduate School of Korea University of Technology and Education, Master’s Thesis. 2007.11. Nielsen J, Landauer TK. A mathematical model of the finding of usability problems. Proceedings of the INTERACT’93 and CHI’93 conference on Human factors in computing systems. 1993; DOI: 10.1145/169059.169166.12. Hwang H. Work management. Seoul: Youngji munhwhasa;1987. p. 203–7.13. Wright TP. Factors affecting the cost of airplanes. J Aeronaut Sci. 1936; 3:122–8. DOI: 10.2514/8.155.14. Kahouli-Brahmi S. Technological learning in energy-environment-economy modelling:a survey. Energy Policy. 2008; 36:138–62. DOI: 10.1016/j.enpol.2007.09.001.15. Chambers D. Learning curves:what do dental students learn from repeated practice of clinical procedures? J Dent Educ. 2012; 76:291–302.16. Kim J. Comparison of learning curves between two different intraoral scanners. Available from: http://www.riss.kr/search/detail/DetailView.do?p_mat_type=b.e54d9b8bc7cdb09&control_no=22db7118864f83fdff.e0bdc3ef48d419. updated 2017 May 9.17. Simpson AH, Howie CR, Norrie J. Surgical trial design - learning curve and surgeon volume:determining whether inferior results are due to the procedure itself, or delivery of the procedure by the surgeon. Bone Joint Res. 2017; 6:194–5. DOI: 10.1302/2046-3758.64.BJR-2017-0051. PMID: 28377379. PMCID: PMC5415901.18. Gonzalez JM, Cohen J, Gromski MA, Saito K, Loundou A, Matthe K. Learning curve for endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) of pancreatic lesions in a novel ex-vivo simulation model. Endosc Int Open. 2016; 4:E128691. DOI: 10.1055/s-0042-118176.19. Ospina ODA, Medina ÁMR, Marulanda MC, Buitrago LMG. Cumulative Sum learning curves (CUSUM) in basic anaesthesia procedures. Rev Colomb Anestesiol. 2014; 42:142–53. DOI: 10.1016/j.rcae.2014.04.005.20. Khan N, Abboudi H, Khan MS, Dasgupta P, Ahmed K. Measuring the surgical ‘learning curve’: methods, variables and competency. BJU Int. 2014; 113:504–8. DOI: 10.1111/bju.12197. PMID: 23819461.21. Berglund C, Söderholm P. Modeling technical change in energy system analysis:analyzing the introduction of learning-by-doing in bottom-up energy models. Energy Policy. 2006; 34:1344–56. DOI: 10.1016/j.enpol.2004.09.002.22. Ray LaHood, Lisa P. Jackson. Final rule making for 2017-2025 light-duty vehicle greenhouse gas emission standards and corporate average fuel economy standards. EPA and NHTSA. 2012; 3–24.23. Jirapinyo P, Abidi WM, Aihara H, Zaki T, Tsay C, Imaeda AB, Thompson CC. Preclinical endoscopic training using a part-task simulator:learning curve assessment and determination of threshold score for advancement to clinical endoscopy. Surg Endosc. 2017; Feb. 22. doi:10.1007/s00464-0175436-x. [Epub ahead of print].24. Arai T, Lefèvre T, Hovasse T, Hayashida K, Watanabe Y, O’Connor SA, Benamer H, Garot P, Cormier B, Bouvier E, Morice MC, Chevalier B. Evaluation of the learning curve for transcatheter aortic valve implantation via the transfemoral approach. Int J Cardiol. 2016; 203:491–7. DOI: 10.1016/j.ijcard.2015.10.178. PMID: 26547745 .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluating usability of and satisfaction with two types of dental CAD software
- Comparative study of two CAD software programs on consistency between custom abutment design and the output
- Comparative analysis of distance measurement on the rendering screen between dental CAD programs
- Use of the surface-based registration function of computer-aided design/computer-aided manufacturing software in medical simulation software for three-dimensional simulation of orthognathic surgery
- Three-dimensional evaluation of the machinability of monolithic CAD/CAM-generated posterior crowns by nano-hybrid ceramic