Kosin Med J.
2017 Jun;32(1):36-46. 10.7180/kmj.2017.32.1.36.
Hemodynamic Effects of Co-administration of Midazolam during Anesthesia Induction with Propofol and Remifentanil in Hypertensive Patients
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, College of Medicine Kosin University, Busan, Korea. kimkh6266@naver.com
- KMID: 2384832
- DOI: http://doi.org/10.7180/kmj.2017.32.1.36
Abstract
OBJECTIVES
Propofol, midazolam and remifentanil are commonly used for clinical anesthesia. We compared the effects of midazolam-propofol-remifentanil and propofol-remifentanil on hemodynamic responses during anesthesia induction in hypertensive patients.
METHODS
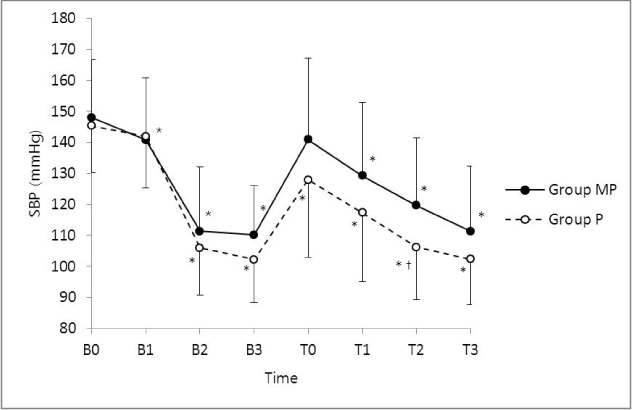
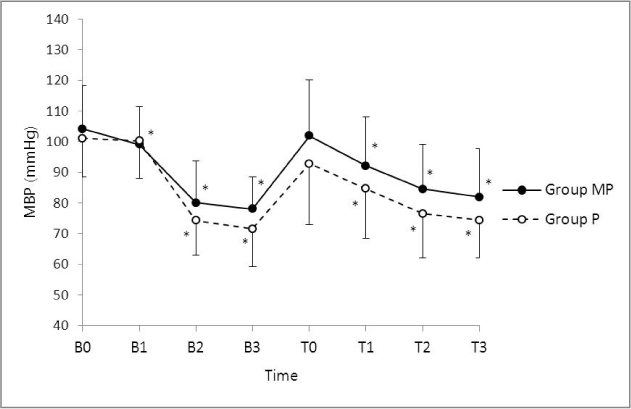
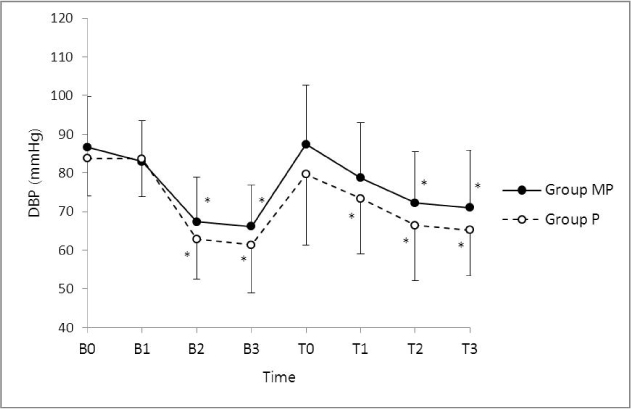
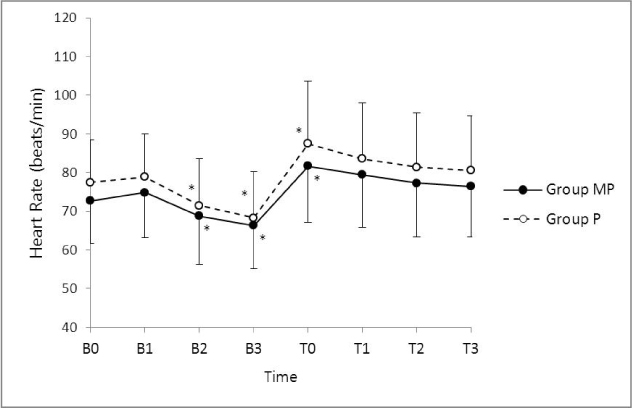
Seventy-six hypertensive patients with ASA II-III were assigned to receive midazolam-propofol (group MP; n = 38) or propofol (group P; n = 38). Anesthesia was induced with midazolam 0.03 mg/kg (group MP) or saline 0.03 ml/kg (group P). After two minutes, propofol 1.0 mg/kg (group MP) or 1.5 mg/kg (group P) i.v. bolus was administered. Simultaneously, 4 ng/ml of remifentanil target controlled infusion (TCI) was administered in both groups. Anesthesia was maintained using sevoflurane and 2 ng/ml of remifentanil TCI. Systolic, diastolic, and mean blood pressure (SBP, DBP, and MBP) and heart rate (HR) were measured before induction, 2 min after midazolam or normal saline, 2 min after propofol, 1 min after rocuronium, and immediately, 1 min, 2 min, and 3 min after intubation.
RESULTS
SBP, DBP, and MBP decreased after propofol administration and increased immediately after intubation in both groups (P < 0.05). After intubation, SBP, DBP, and MBP decreased more than baseline values in either group. Although the overall BP of Group P was lower than that of Group MP, there were no significant differences except for SBP at 2min after intubation (P < 0.05). HR was no significant difference in either group.
CONCLUSION
Our results suggest that midazolam-propofol-remifentanil has similar hemodynamic effect with propofol-remifentanil during anesthesia induction in hypertensive patients.
MeSH Terms
Figure
Reference
-
1. Short TG, Chui PT. Propofol and midazolam act synergistically in combination. Br J Anaesth. 1991; 67:539–545.
Article2. Mc Clune S, McKay AC, Wright PM, Patterson CC, Clarke RS. Synergistic interaction between midazolam and propofol. Br J Anaesth. 1992; 69:240–245.
Article3. Cressey DM, Claydon P, Bhaskaran NC, Reilly CS. Effect of midazolam pretreatment on induction dose requirments of propofol in combination with fentanyl in younger and older adults. Anaesthesia. 2001; 56:108–113.
Article4. Wilder-Smith OH, Ravussin PA, Decosterd LA, Despland PA, Bissonnette B. Midazolam premedication reduces propofol dose requirements for multiple anesthetic endpoints. Can J Anaesth. 2001; 48:439–445.
Article5. Prys-Roberts C, Greene LT, Meloche R, Foëx P. Studies of anaesthesia in relation to hypertension. II: Hemodynamic consequences of induction and endotracheal intubation. 1971. Br J Anaesth. 1998; 80:106–122.
Article6. Stone JG, Foëx P, Sear JW, Johnson LL, Khambatta HJ, Triner L. Risk of myocardial ischaemia during anaesthesia in treated and untreated hypertensive patients. Br J Anaesth. 1988; 61:675–679.
Article7. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997; 86:10–23.
Article8. Hendrickx JF, Eger EI 2nd, Sonner JM, Shafer SL. Is synergy the rule? A review of anesthetic interactions producing hypnosis and immobility. Anesth Analg. 2008; 107:494–506.
Article9. Win NN, Kohase H, Yoshikawa F, Wakita R, Takahashi M, Kondo N, et al. Haemodynamic changes and heart rate variability during midazolam-propofol co-induction. Anaesthesia. 2007; 62:561–568.
Article10. Lee SH, Han JI, Kim CH. Target-controlled infusion of remifentanil during propofol induction in hypertensive patients: effects of three different remifentanil concentrations on hemodynamic changes. Korean J Anesthesiol. 2007; 53:S12–S18.
Article11. Djaiani G, Ribes-Pastor MP. Propofol auto-co-induction as an alternative to midazolam co–induction for ambulatory surgery. Anaesthesia. 1999; 54:63–67.
Article12. Pagel PS, Warltier DC. Negative inotropic effects of propofol as evaluated by the regional preload recruitable stroke work relationship in chronically instrumented dogs. Anesthesiology. 1993; 78:100–108.
Article13. Larsen R, Rathgeber , Bagdahn A, Lange H, Rieke H. Effects of propofol on cardiovascular dynamics and coronary blood flow in geriatric patients: A comparison with etomidate. Anaesthesia. 1988; 43:Suppl. 25–31.
Article14. Rosow C. Remifentanil: A unique opioid analgesic. Anesthesiology. 1993; 79:875–876.15. Gwak MS, Choi SJ, Yoon JS, Lee JY, Yang MK, Kim GS, et al. Hemodynamic responses to rapid sequence endotracheal intubation using propofol and rocuronium at three different doses of remifentanil infusion. Korean J Anesthesiol. 2006; 50:385–389.
Article16. Park SJ, Shim YH, Yoo JH, Nam SH, Lee JW. Low-dose remifentanil to modify hemodynamic responses to tracheal intubation: comparison in normotensive and untreated/treated hypertensive Korean patients. Korean J Anesthesiol. 2012; 62:135–141.
Article17. Kang HS, Yu SB, Kim DS, Ryu SJ, Chang TH, Kim SH, et al. The effects of remifentanil and lidocaine on the cardiovascular responses to tracheal intubation in hypertensive patients. Korean J Anesthesiol. 2009; 57:20–25.
Article18. Hogue CW Jr, Bowdle TA, O'Leary C, Duncalf D, Miguel R, Pitts M, et al. A multicenter evaluation of total intravenous anesthesia with remifentanil and propofol for elective inpatient surgery. Anesth Analg. 1996; 83:279–285.
Article19. Maguire AM, Kumar N, Parker JL, Rowbotham DJ, Thompson JP. Comparison of effects of remifentanil and alfentanil on cardiovascular response to tracheal intubation in hypertensive patients. Br J Anaesth. 2001; 86:90–93.
Article20. Kazama T, Ikeda K, Morita K, Kikura M, Ikeda T, Kurita T, et al. Investigation of effective anesthesia induction doses using a wide range of infusion rates with undiluted and diluted propofol. Anesthesiology. 2000; 92:1017–1028.
Article21. De Castro V, Godet G, Mencia G, Raux M, Coriat P. Target-controlled infusion for remifentanil in vascular patients improves hemodynamics and decreases remifentanil requirement. Anesth Analg. 2003; 96:33–38.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effects of midazolam and remifentanil on induction of anesthesia and hemodynamics during tracheal intubation under target-controlled infusion of propofol
- Changes of Bispectral Index and Auditory Evoked Potential Index during General Anesthesia with Propofol, Midazolam and Ketamine
- The Effect of Co-administration of Midazolam on Induction and Recovery Using Continuous Propofol Infusion
- Hemodynamic Changes between Different Remifentanil Administration Methods during Induction in the Elderly
- Comparison of Remifentanil-Propofol and Remifentanil-Sevoflurane Anesthesia for Pediatric Tonsillectomy