Korean J Gastroenterol.
2017 Jun;69(6):368-371. 10.4166/kjg.2017.69.6.368.
Malignant Melanoma of the Anus Found during Routine Colonoscopy in Ulcerative Colitis
- Affiliations
-
- 1Department of Internal Medicine, Kosin University College of Medicine, Busan, Korea. moonone70@hanmail.net
- KMID: 2384365
- DOI: http://doi.org/10.4166/kjg.2017.69.6.368
Abstract
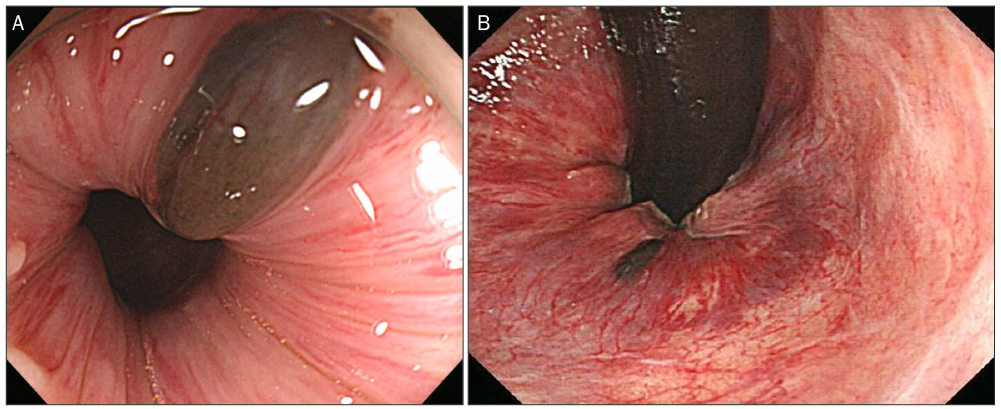
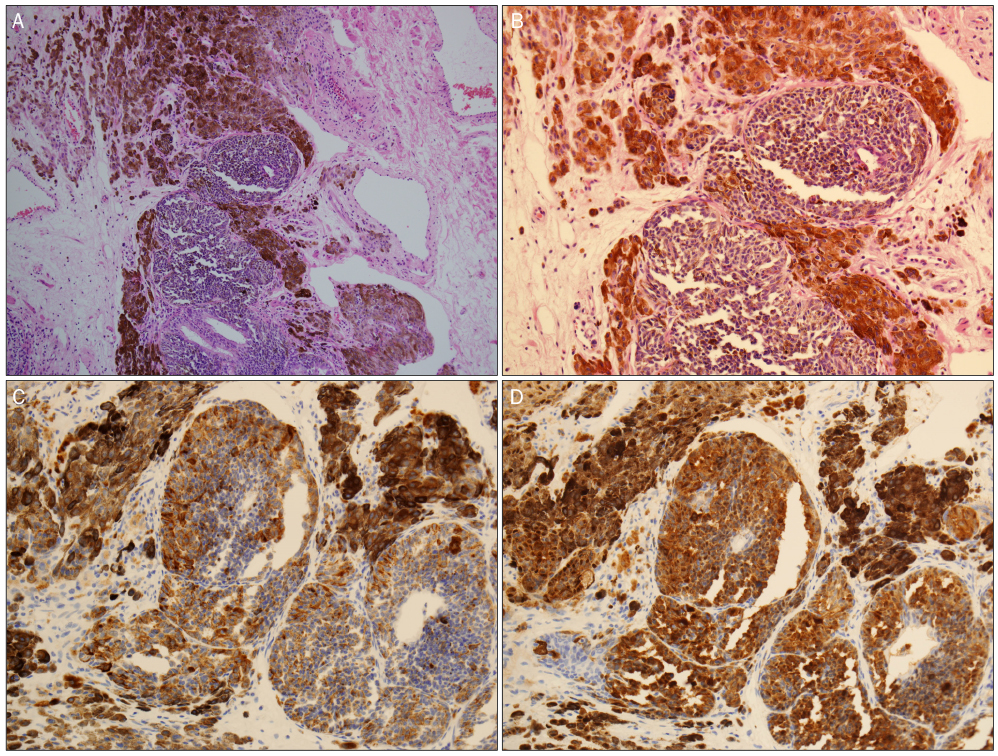
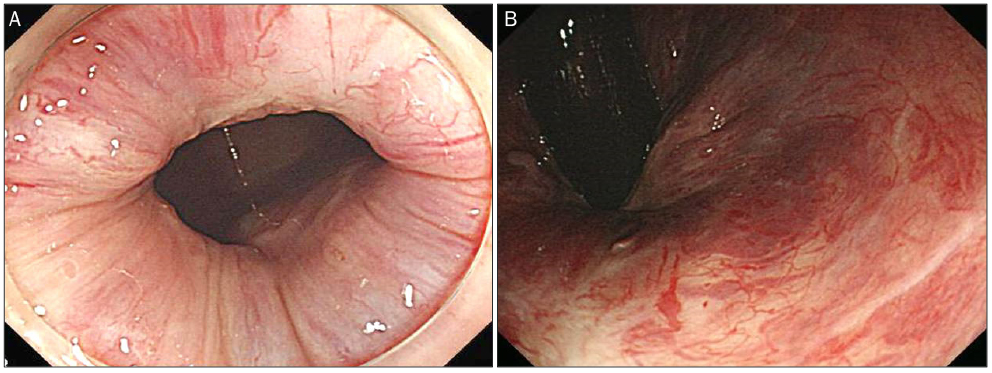
- Inflammatory bowel disease (IBD) is characterized by recurrent or chronic inflammation of the gastrointestinal tract, which results in increased risk of developing cancer. Anorectal malignant melanoma is often misdiagnosed as either hemorrhoids or benign anorectal conditions in inflammatory bowel disease. Therefore, the overall prognosis and survival of IBD are poor. To date, the best treatment strategy remains controversial. Only early diagnosis and complete excision yield survival benefit. Here, we report a 64-year-old woman with ulcerative colitis, who was found to have anal malignant melanoma on routine colonoscopy. The lesion was confined to the mucosa with no distant metastasis. She underwent complete trans-anal excision. There was no recurrence at the four-year follow-up. Physicians should be aware of increased risk of cancer development in IBD patients and remember the importance of meticulous inspection of the anal canal.
Keyword
MeSH Terms
Figure
Reference
-
1. Kappelman MD, Farkas DK, Long MD, et al. Risk of cancer in patients with inflammatory bowel diseases: a nationwide population-based cohort study with 30 years of follow-up evaluation. Clin Gastroenterol Hepatol. 2014; 12:265–273.e1.2. Pei W, Zhou H, Chen J, Liu Q. Treatment and prognosis analysis of 64 cases with anorectal malignant melanoma. Zhonghua Wei Chang Wai Ke Za Zhi. 2016; 19:1305–1308.3. Ng WK, Wong SH, Ng SC. Changing epidemiological trends of inflammatory bowel disease in Asia. Intest Res. 2016; 14:111–119.4. Garg SK, Loftus EV Jr. Risk of cancer in inflammatory bowel disease: going up, going down, or still the same? Curr Opin Gastroenterol. 2016; 32:274–281.5. Shah SB, Pickham D, Araya H, et al. Prevalence of anal dysplasia in patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2015; 13:1955–1961.e1.6. Slesser AA, Bhangu A, Bower M, Goldin R, Tekkis PP. A systematic review of anal squamous cell carcinoma in inflammatory bowel disease. Surg Oncol. 2013; 22:230–237.7. Singh S, Nagpal SJ, Murad MH, et al. Inflammatory bowel disease is associated with an increased risk of melanoma: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014; 12:210–218.8. Kim ER, Chang DK. Colorectal cancer in inflammatory bowel disease: the risk, pathogenesis, prevention and diagnosis. World J Gastroenterol. 2014; 20:9872–9881.9. Abbas AM, Almukhtar RM, Loftus EV Jr, Lichtenstein GR, Khan N. Risk of melanoma and non-melanoma skin cancer in ulcerative colitis patients treated with thiopurines: a nationwide retrospective cohort. Am J Gastroenterol. 2014; 109:1781–1793.10. Cheung MC, Perez EA, Molina MA, et al. Defining the role of surgery for primary gastrointestinal tract melanoma. J Gastrointest Surg. 2008; 12:731–738.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Non-Hodgkin's Lymphoma in Ulcerative Colitis
- A Case of Malignant Lymphoma in Patient with Ulcerative Colitis
- Malignant change of chronic ulcerative colitis : report of a case
- Usefulness of Magnifying Chromoscopy in Ulcerative Colitis
- A Case of Acute Pancreatitis associated with Ulcerative Colitis