Clin Endosc.
2015 Nov;48(6):570-575. 10.5946/ce.2015.48.6.570.
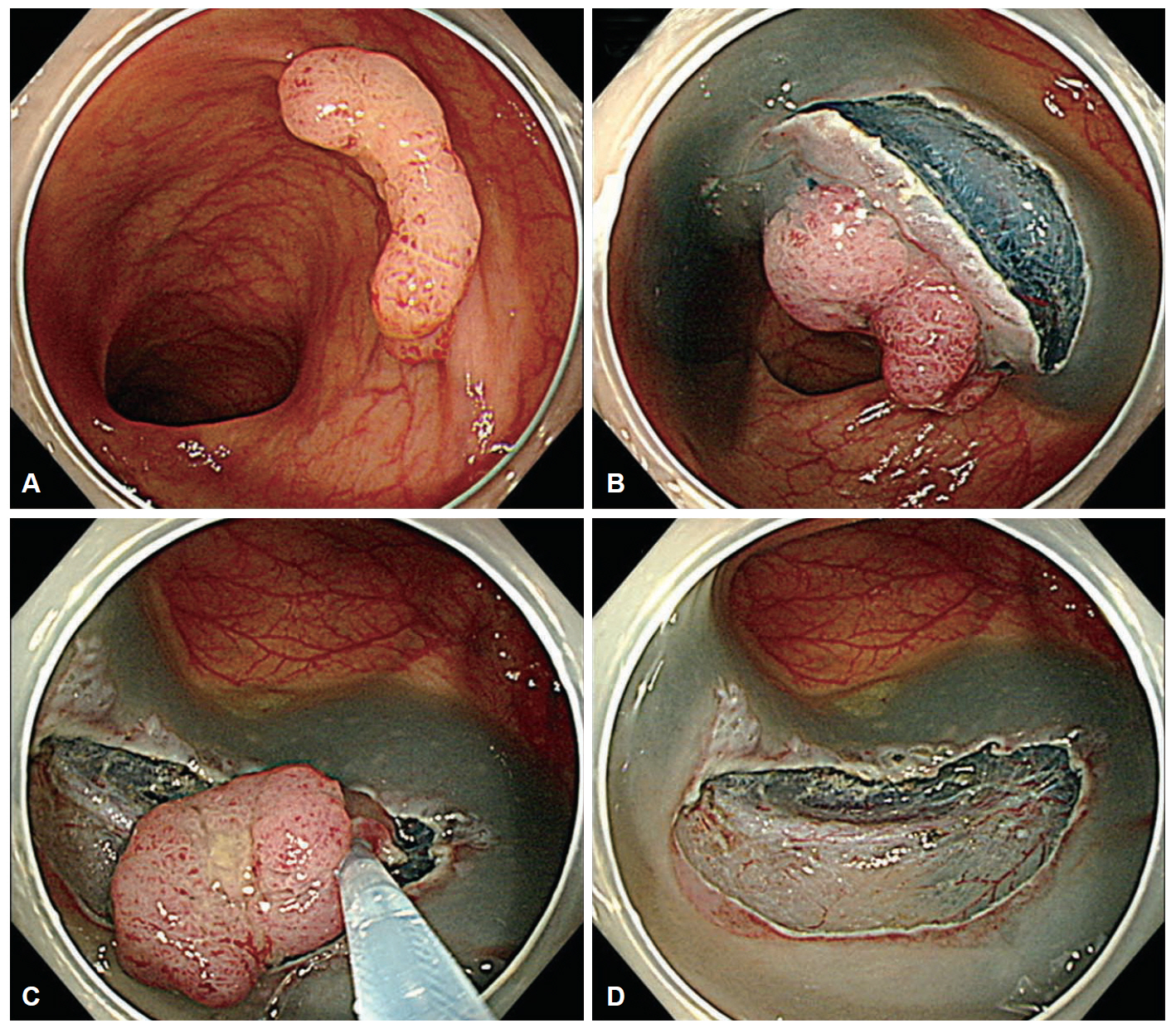
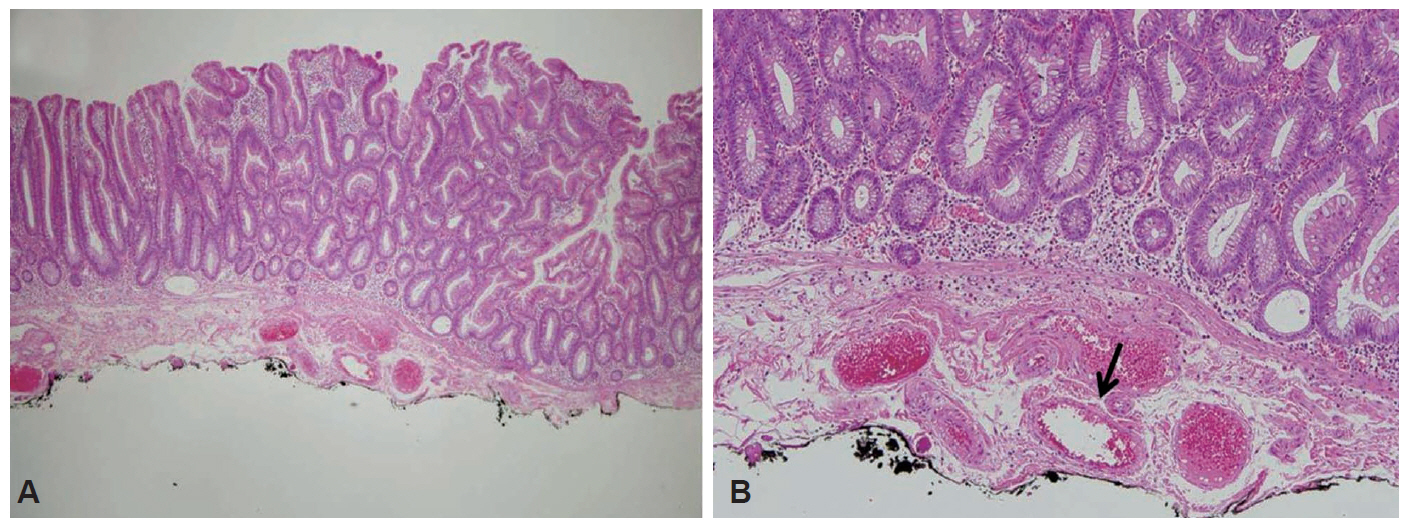
Unexpected Delayed Colon Perforation after the Endoscopic Submucosal Dissection with Snaring of a Laterally Spreading Tumor
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. jsbyeon@amc.seoul.kr
- KMID: 2380419
- DOI: http://doi.org/10.5946/ce.2015.48.6.570
Abstract
- Colonic perforation may occur as a complication of diagnostic and therapeutic colonoscopy. The risk factors for perforation after colorectal endoscopic submucosal dissection (ESD) include an inexperienced endoscopist, a large tumor size, and submucosal fibrosis. The mechanisms of perforation include unintended endoscopic resection/dissection and severe thermal injury. Here, we report a case of colon perforation that occurred after ESD with snaring of a laterally spreading tumor. The perforation was completely unexpected because there were no colorectal ESD-associated risk factors for perforation, deep dissection, or severe coagulation injury in our patient.
Figure
Reference
-
1. Raju GS, Saito Y, Matsuda T, Kaltenbach T, Soetikno R. Endoscopic management of colonoscopic perforations (with videos). Gastrointest Endosc. 2011; 74:1380–1388.
Article2. Panteris V, Haringsma J, Kuipers EJ. Colonoscopy perforation rate, mechanisms and outcome: from diagnostic to therapeutic colonoscopy. Endoscopy. 2009; 41:941–951.
Article3. Mizushima T, Kato M, Iwanaga I, et al. Technical difficulty according to location, and risk factors for perforation, in endoscopic submucosal dissection of colorectal tumors. Surg Endosc. 2015; 29:133–139.
Article4. Isomoto H, Nishiyama H, Yamaguchi N, et al. Clinicopathological factors associated with clinical outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms. Endoscopy. 2009; 41:679–683.
Article5. Xiao YF, Bai JY, Yu J, et al. Endoscopic treatment of delayed colon perforation: the enteroscopy overtube approach. Endoscopy. 2014; 46:503–508.
Article6. Hagel AF, Boxberger F, Dauth W, Kessler HP, Neurath MF, Raithel M. Colonoscopy-associated perforation: a 7-year survey of in-hospital frequency, treatment and outcome in a German university hospital. Colorectal Dis. 2012; 14:1121–1125.
Article7. Araghizadeh FY, Timmcke AE, Opelka FG, Hicks TC, Beck DE. Colonoscopic perforations. Dis Colon Rectum. 2001; 44:713–716.
Article8. Fujishiro M, Yahagi N, Kakushima N, et al. Outcomes of endoscopic submucosal dissection for colorectal epithelial neoplasms in 200 consecutive cases. Clin Gastroenterol Hepatol. 2007; 5:678–683.
Article9. Nakamura F, Saito Y, Sakamoto T, et al. Potential perioperative advantage of colorectal endoscopic submucosal dissection versus laparoscopy-assisted colectomy. Surg Endosc. 2015; 29:596–606.
Article10. Saito Y, Uraoka T, Yamaguchi Y, et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc. 2010; 72:1217–1225.
Article11. Kim ES, Cho KB, Park KS, et al. Factors predictive of perforation during endoscopic submucosal dissection for the treatment of colorectal tumors. Endoscopy. 2011; 43:573–578.
Article12. Byeon JS, Yang DH, Kim KJ, et al. Endoscopic submucosal dissection with or without snaring for colorectal neoplasms. Gastrointest Endosc. 2011; 74:1075–1083.
Article13. Lohsiriwat V. Colonoscopic perforation: incidence, risk factors, management and outcome. World J Gastroenterol. 2010; 16:425–430.
Article14. Yang DH, Byeon JS, Lee KH, et al. Is endoscopic closure with clips effective for both diagnostic and therapeutic colonoscopy-associated bowel perforation? Surg Endosc. 2010; 24:1177–1185.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Synchronous Colonic Laterally Spreading Tumors Treated by Sequential Endoscopic Submucosal Dissection Performed on Two Consecutive Days
- A Case of Pneumorrhachis and Pneumoscrotum Following Colon Endoscopic Submucosal Dissection
- Submerging Endoscopic Submucosal Dissection Leads to Successful En Bloc Resection of Colonic Laterally Spreading Tumor with Submucosal Fat
- Endoscopic Treatment Strategy for Large Laterally Spreading Tumor: Endoscopic Piecemeal Mucosal Resection or Endoscopic Submucosal Dissection
- Perforation of a Gastric Tear during Esophageal Endoscopic Submucosal Dissection under General Anesthesia