Korean Circ J.
2017 Mar;47(2):263-269. 10.4070/kcj.2016.0359.
Prognostic Implication of the QRS Axis and its Association with Myocardial Scarring in Patients with Left Bundle Branch Block
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea. seil@snu.ac.kr
- KMID: 2377468
- DOI: http://doi.org/10.4070/kcj.2016.0359
Abstract
- BACKGROUND AND OBJECTIVES
Left bundle branch block (LBBB) with left axis deviation (LAD) has a worse prognosis than LBBB with a normal axis, and myocardial dysfunction has been suggested as a cause of left axis deviation. This study investigated the prognostic significance of the QRS axis in patients with LBBB and analyzed its relationship with the amount of myocardial scarring.
SUBJECTS AND METHODS
A total of 829 patients were diagnosed with LBBB at Seoul National University Hospital from October 2004 to June 2014. Of these, 314 who were asymptomatic and had no previous history of cardiac disease were included in the present study. Myocardial scarring was calculated using the Selvester QRS scoring system, and LAD was defined as a QRS axis between -180° and -30°.
RESULTS
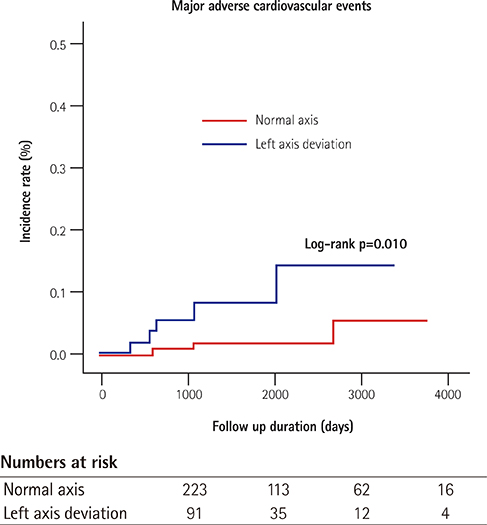
Of the total patients, 91 (29%) had LAD, and patients were followed for a median of 30 months. During follow-up, two patients were hospitalized for de novo heart failure, four had pacemaker implants, and 10 died. There was a significant inverse correlation between myocardial scar score and the QRS axis (r=-0.356, p<0.001). Patients with concomitant LAD had a higher rate of major cardiac adverse events compared with patients with a normal axis (5.5% vs. 1.3%, log-rank p=0.010); the prognostic value was attenuated in multivariable analysis (hazard ratio 4.117; 95% confidence interval 0.955-17.743; p=0.058).
CONCLUSION
Concomitant LAD is an indicator of poor prognosis for patients with LBBB and may be associated with greater myocardial scarring.
MeSH Terms
Figure
Cited by 2 articles
-
Left Axis Deviation in Patients with Acute Heart Failure with Left Bundle Branch Block: Does It Really Matter?
Eue-Keun Choi
Korean Circ J. 2018;48(11):1012-1013. doi: 10.4070/kcj.2018.0222.Prognostic Significance of Left Axis Deviation in Acute Heart Failure Patients with Left Bundle branch block: an Analysis from the Korean Acute Heart Failure (KorAHF) Registry
Ki Hong Choi, Seongwook Han, Ga Yeon Lee, Jin-Oh Choi, Eun-Seok Jeon, Hae-Young Lee, Sang Eun Lee, Jae-Joong Kim, Shung Chull Chae, Sang Hong Baek, Seok-Min Kang, Dong-Ju Choi, Byung-Su Yoo, Kye Hun Kim, Myeong-Chan Cho, Hyun-Young Park, Byung-Hee Oh
Korean Circ J. 2018;48(11):1002-1011. doi: 10.4070/kcj.2018.0048.
Reference
-
1. Haft JI, Herman MV, Gorlin R. Left bundle branch block: etiologic, hemodynamic, and ventriculographic considerations. Circulation. 1971; 43:279–287.2. Yano K, Peskoe SM, Rhoads GG, Moore JO, Kagan A. Left axis deviation and left anterior hemiblock among 8,000 Japanese-American men. Am J Cardiol. 1975; 35:809–815.3. Patel PJ, Verdino RJ. Usefulness of QRS axis change to predict mortality in patients with left bundle branch block. Am J Cardiol. 2013; 112:390–394.4. Dhingra RC, Amat-Y-Leon F, Wyndham C, Sridhar SS, Wu D, Rosen KM. Significance of left axis deviation in patients with chronic left bundle branch block. Am J Cardiol. 1978; 42:551–556.5. Lichstein E, Mahapatra R, Gupta PK, Chadda KD. Significance of complete left bundle branch block with left axis deviation. Am J Cardiol. 1979; 44:239–242.6. Parharidis G, Nouskas J, Efthimiadis G, et al. Complete left bundle branch block with left QRS axis deviation: defining its clinical importance. Acta Cardiol. 1997; 52:295–303.7. Wagner GS, Freye CJ, Palmeri ST, et al. Evaluation of a QRS scoring system for estimating myocardial infarct size. I. Specificity and observer agreement. Circulation. 1982; 65:342–347.8. Strauss DG, Selvester RH. The QRS complex--a biomarker that “images” the heart: QRS scores to quantify myocardial scar in the presence of normal and abnormal ventricular conduction. J Electrocardiol. 2009; 42:85–96.9. Lee SA, Cha MJ, Cho Y, Oh IY, Choi EK, Oh S. Paced QRS duration and myocardial scar amount: predictors of long-term outcome of right ventricular apical pacing. Heart Vessels. 2016; 31:1131–1139.10. Strauss DG, Selvester RH, Lima JA, et al. ECG quantification of myocardial scar in cardiomyopathy patients with or without conduction defects: correlation with cardiac magnetic resonance and arrhythmogenesis. Circ Arrhythm Electrophysiol. 2008; 1:327–336.11. Strauss DG, Cardoso S, Lima JA, Rochitte CE, Wu KC. ECG scar quantification correlates with cardiac magnetic resonance scar size and prognostic factors in Chagas' disease. Heart. 2011; 97:357–361.12. Loring Z, Chelliah S, Selvester RH, Wagner G, Strauss DG. A detailed guide for quantification of myocardial scar with the Selvester QRS score in the presence of electrocardiogram confounders. J Electrocardiol. 2011; 44:544–554.13. Strauss DG, Selvester RH, Wagner GS. Defining left bundle branch block in the era of cardiac resynchronization therapy. Am J Cardiol. 2011; 107:927–934.14. Pryor R, Blount SG Jr. The clinical significance of true left axis deviation. Left intraventricular blocks. Am Heart J. 1966; 72:391–413.15. Beach TB, Gracey JG, Peter RH, Grunenwald PW. Benign left bundle branch block. Ann Intern Med. 1969; 70:269–276.16. Miller WL, Hodge DO, Hammill SC. Association of uncomplicated electrocardiographic conduction blocks with subsequent cardiac morbidity in a community-based population (Olmsted County, Minnesota). Am J Cardiol. 2008; 101:102–106.17. McCrohon JA, Moon JC, Prasad SK, et al. Differentiation of heart failure related to dilated cardiomyopathy and coronary artery disease using gadolinium-enhanced cardiovascular magnetic resonance. Circulation. 2003; 108:54–59.18. Moon JC, McKenna WJ, McCrohon JA, Elliott PM, Smith GC, Pennell DJ. Toward clinical risk assessment in hypertrophic cardiomyopathy with gadolinium cardiovascular magnetic resonance. J Am Coll Cardiol. 2003; 41:1561–1567.19. Blyth KG, Groenning BA, Martin TN, et al. Contrast enhanced-cardiovascular magnetic resonance imaging in patients with pulmonary hypertension. Eur Heart J. 2005; 26:1993–1999.20. Davis JA. Anaerobic threshold: review of the concept and directions for future research. Med Sci Sports Exerc. 1985; 17:6–21.21. Gaultier C, Boule M, Thibert M, Leca F. Resting lung function in children after repair of tetralogy of Fallot. Chest. 1986; 89:561–567.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Retrograde Conduction in Complete Heart Block
- Preexcitation Syndrome with a Mahaim-type Accessory Pathway
- Rate-dependent Left Bundle Branch Block during General Anesthesia : A case report
- Supraventricular Tachycardia and Sinus Rhythm with Contralateral Bundle Branch Block Patterns
- Left Axis Deviation in Patients with Acute Heart Failure with Left Bundle Branch Block: Does It Really Matter?