J Korean Med Sci.
2017 May;32(5):789-795. 10.3346/jkms.2017.32.5.789.
The Definition of Past Tuberculosis Affects the Magnitude of Association between Pulmonary Tuberculosis and Respiratory Dysfunction: Korea National Health and Nutrition Examination Survey, 2008–2012
- Affiliations
-
- 1Department of Family Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea. kskim@catholic.ac.kr
- 2Division of Pulmonology Medicine, Department of Internal Medicine, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- KMID: 2375079
- DOI: http://doi.org/10.3346/jkms.2017.32.5.789
Abstract
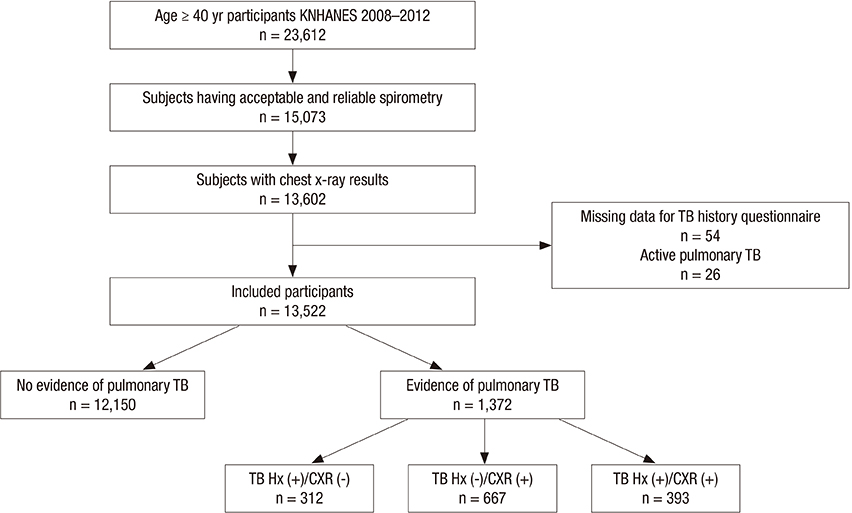
- Tuberculosis (TB) is associated with an increased risk of chronic lung impairment. The aim of this study was to compare the clinical characteristics and lung functions according to definition of past TB. We used the population-based, Korea National Health and Nutrition Examination Survey (KNHANES) (2008-2012) to analyze 13,522 subjects age 40 years or older who underwent spirometry and chest X-ray (CXR). Subjects with TB lesions on CXR (with or without a history of TB) were older, more likely to be male, ever smokers, and of low socioeconomic status than subjects with only a history of TB or without evidence of TB. Airflow obstruction (AFO) was associated with only a history of TB (odds ratio [OR] 1.53, 95% confidence interval [CI] 0.95-2.46), only TB lesion on CXR (OR 2.37, 95% CI 1.80-3.12), and both a history and TB lesions on CXR (OR 4.47, 95% CI 3.07-6.51) after adjustment for gender, age, body mass index, education, income, and smoking amount (P for trend < 0.001). Spirometric restriction was associated with only a history of TB (OR 1.29, 95% CI 0.80-2.08), only TB lesions on CXR (OR 2.03, 95% CI 1.49-2.76), and both a history and TB lesions on CXR (OR 2.65, 95% CI 1.74-4.05) after adjustment for the above variables (P for trend < 0.001). How to define past TB in population study affects the magnitude of association between past TB and respiratory dysfunction. Without considering TB lesions on CXR, the association between TB and respiratory dysfunction could be underestimated.
MeSH Terms
Figure
Reference
-
1. World Health Organization. Global tuberculosis report 2015 [Internet]. Geneva, Switzerland: World Health Organization;2015. accessed on 11 October 2016. Available at http://www.who.int/tb/publications/global_report/en/.2. Vecino M, Pasipanodya JG, Slocum P, Bae S, Munguia G, Miller T, Fernandez M, Drewyer G, Weis SE. Evidence for chronic lung impairment in patients treated for pulmonary tuberculosis. J Infect Public Health. 2011; 4:244–252.3. Dheda K, Booth H, Huggett JF, Johnson MA, Zumla A, Rook GA. Lung remodeling in pulmonary tuberculosis. J Infect Dis. 2005; 192:1201–1209.4. Byrne AL, Marais BJ, Mitnick CD, Lecca L, Marks GB. Tuberculosis and chronic respiratory disease: a systematic review. Int J Infect Dis. 2015; 32:138–146.5. Allwood BW, Myer L, Bateman ED. A systematic review of the association between pulmonary tuberculosis and the development of chronic airflow obstruction in adults. Respiration. 2013; 86:76–85.6. Amaral AF, Coton S, Kato B, Tan WC, Studnicka M, Janson C, Gislason T, Mannino D, Bateman ED, Buist S, et al. Tuberculosis associates with both airflow obstruction and low lung function: BOLD results. Eur Respir J. 2015; 46:1104–1112.7. Menezes AM, Hallal PC, Perez-Padilla R, Jardim JR, Muiño A, Lopez MV, Valdivia G, Montes de Oca M, Talamo C, Pertuze J, et al. Tuberculosis and airflow obstruction: evidence from the PLATINO study in Latin America. Eur Respir J. 2007; 30:1180–1185.8. Caballero A, Torres-Duque CA, Jaramillo C, Bolívar F, Sanabria F, Osorio P, Orduz C, Guevara DP, Maldonado D. Prevalence of COPD in five Colombian cities situated at low, medium, and high altitude (PREPOCOL study). Chest. 2008; 133:343–349.9. Lam KB, Jiang CQ, Jordan RE, Miller MR, Zhang WS, Cheng KK, Lam TH, Adab P. Prior TB, smoking, and airflow obstruction: a cross-sectional analysis of the Guangzhou Biobank Cohort Study. Chest. 2010; 137:593–600.10. Lee SW, Kim YS, Kim DS, Oh YM, Lee SD. The risk of obstructive lung disease by previous pulmonary tuberculosis in a country with intermediate burden of tuberculosis. J Korean Med Sci. 2011; 26:268–273.11. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.12. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319–338.13. Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009; 374:733–743.14. Lee SJ, Kim SW, Kong KA, Ryu YJ, Lee JH, Chang JH. Risk factors for chronic obstructive pulmonary disease among never-smokers in Korea. Int J Chron Obstruct Pulmon Dis. 2015; 10:497–506.15. Mbatchou Ngahane BH, Nouyep J, Nganda Motto M, Mapoure Njankouo Y, Wandji A, Endale M, Afane Ze E. Post-tuberculous lung function impairment in a tuberculosis reference clinic in Cameroon. Respir Med. 2016; 114:67–71.16. Plit ML, Anderson R, Van Rensburg CE, Page-Shipp L, Blott JA, Fresen JL, Feldman C. Influence of antimicrobial chemotherapy on spirometric parameters and pro-inflammatory indices in severe pulmonary tuberculosis. Eur Respir J. 1998; 12:351–356.17. Rhee CK, Yoo KH, Lee JH, Park MJ, Kim WJ, Park YB, Hwang YI, Kim YS, Jung JY, Moon JY, et al. Clinical characteristics of patients with tuberculosis-destroyed lung. Int J Tuberc Lung Dis. 2013; 17:67–75.18. O’Toole RF, Shukla SD, Walters EH. TB meets COPD: An emerging global co-morbidity in human lung disease. Tuberculosis (Edinb). 2015; 95:659–663.19. Fletcher C, Peto R. The natural history of chronic airflow obstruction. BMJ. 1977; 1:1645–1648.20. Løkke A, Lange P, Scharling H, Fabricius P, Vestbo J. Developing COPD: a 25 year follow up study of the general population. Thorax. 2006; 61:935–939.21. Bates MN, Khalakdina A, Pai M, Chang L, Lessa F, Smith KR. Risk of tuberculosis from exposure to tobacco smoke: a systematic review and meta-analysis. Arch Intern Med. 2007; 167:335–342.22. Slama K, Chiang CY, Enarson DA, Hassmiller K, Fanning A, Gupta P, Ray C. Tobacco and tuberculosis: a qualitative systematic review and meta-analysis. Int J Tuberc Lung Dis. 2007; 11:1049–1061.23. Inghammar M, Ekbom A, Engström G, Ljungberg B, Romanus V, Löfdahl CG, Egesten A. COPD and the risk of tuberculosis--a population-based cohort study. PLoS One. 2010; 5:e10138.24. Lee CH, Kim K, Hyun MK, Jang EJ, Lee NR, Yim JJ. Use of inhaled corticosteroids and the risk of tuberculosis. Thorax. 2013; 68:1105–1113.25. Horsburgh CR Jr. Priorities for the treatment of latent tuberculosis infection in the United States. N Engl J Med. 2004; 350:2060–2067.26. Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CP, Gustafsson P, Hankinson J, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005; 26:948–968.27. Wesołowski S, Boros P. Restrictive pattern in spirometry: does FEV(1)/FVC need to be increased? Pneumonol Alergol Pol. 2011; 79:382–387.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Drug Resistance of Mycobacterium tuberculosis isolated from Patients discovered in the Third National Tuberculosis Prevalence Survey in 1975 in Korea
- Lessons We have Learnt from the Fright Against Tuberculosis During the Past 100 Years
- Classification of Pulmonary Tubercu1osis -Diagnostic standards and Classification of Tuberculosis, Published by National Tuberculosis and Respiratory Disease Association, New York, 1969
- Chemotherapy of Pulmonary Tuberculosis
- A survey of deaths in hospitalized patients for pulmonary tuberculosis