Prenatal Maternal Distress and Allergic Diseases in Offspring: Review of Evidence and Possible Pathways
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
- 2Department of Psychiatry, Ajou University School of Medicine, Suwon, Korea.
- 3Department of Pediatrics, Chonnam National University Hospital, Gwangju, Korea.
- 4Department of Pediatrics, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 5Department of Pediatrics, Childhood Asthma Atopy Center, Environmental Health Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. sjhong@amc.seoul.kr
- KMID: 2371720
- DOI: http://doi.org/10.4168/aair.2017.9.3.200
Abstract
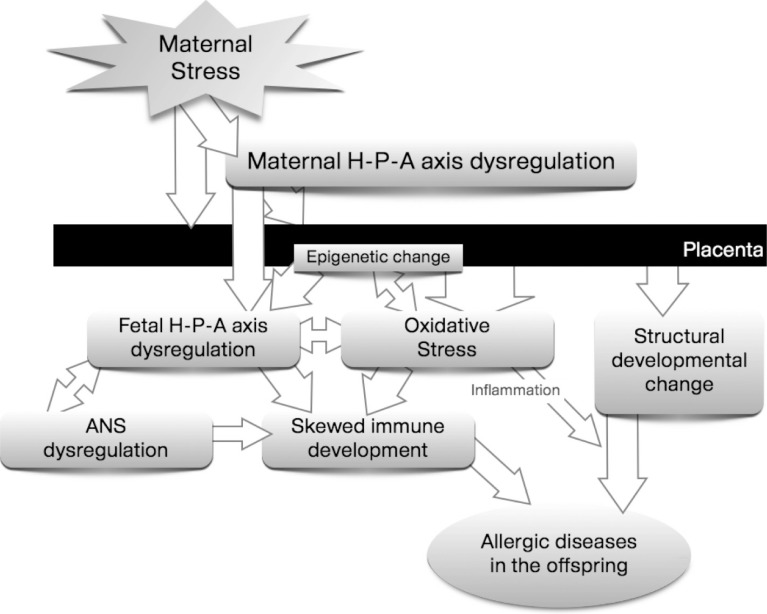
- Recent studies have suggested a close association between prenatal maternal distress and allergic diseases in the offspring. We selected relevant birth-cohort or national registry studies using a keyword search of the PubMed database and summarized current evidence on the impact of prenatal maternal distress on the development of offspring's allergic diseases. Moreover, we postulated possible pathways linking prenatal distress and allergic diseases based on relevant human and animal studies. Both dysregulated hypothalamic-pituitary-adrenal axis and increased oxidative stress may cause structural (altered brain/lung development) and functional (skewed immune development) changes, which may predispose the fetus to developing allergic diseases during childhood. Although many facts are yet to be discovered, changes in the placental response and epigenetic modification are presumed to mediate the whole process from maternal distress to allergic diseases. Maternal prenatal distress can also interact with other physical or environmental factors, including familial or physical factors, indoor and outdoor pollutants, and early childhood psychological distress. The gut-microbiome-brain axis and the role of the microbiome as an immune modulator should be considered when investigating the stress-allergy relationship and exploring potential intervention modalities. Further research is needed, and particular attention should be given to defining the most vulnerable subjects and critical time periods. To this end, studies exploring relevant biomarkers are warranted, which can enable us to explore adequate intervention strategies.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Leukocyte Telomere Length Reflects Prenatal Stress Exposure, But Does Not Predict Atopic Dermatitis Development at 1 Year
Dong In Suh, Mi-Jin Kang, Yoon Mee Park, Jun-Kyu Lee, So-Yeon Lee, Youn Ho Sheen, Kyung Won Kim, Kangmo Ahn, Hye-Sung Won, Mi-Young Lee, Suk-Joo Choi, Ja-Young Kwon, Hee Jin Park, Jong Kwan Jun, Soo-Jong Hong, Young Yull Koh
Allergy Asthma Immunol Res. 2019;11(3):357-366. doi: 10.4168/aair.2019.11.3.357.Complementary Participation of Genetics and Epigenetics in Development of NSAID-exacerbated Respiratory Disease
Jong-Uk Lee, Jong Sook Park, Hun Soo Chang, Choon-Sik Park
Allergy Asthma Immunol Res. 2019;11(6):779-794. doi: 10.4168/aair.2019.11.6.779.The risk of preschool asthma at 2–4 years is not associated with leukocyte telomere length at birth or at 1 year of age
Dong In Suh, Mi-Jin Kang, Yoon Mee Park, Jun-Kyu Lee, So-Yeon Lee, Youn Ho Sheen, Kyung Won Kim, Kangmo Ahn, Soo-Jong Hong
Asia Pac Allergy. 2019;9(4):. doi: 10.5415/apallergy.2019.9.e33.
Reference
-
1. Asher MI, Montefort S, Björkstén B, Lai CK, Strachan DP, Weiland SK, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multicountry cross-sectional surveys. Lancet. 2006; 368:733–743. PMID: 16935684.
Article2. Padmanabhan V, Cardoso RC, Puttabyatappa M. Developmental programming, a pathway to disease. Endocrinology. 2016; 157:1328–1340. PMID: 26859334.
Article3. Trump S, Bieg M, Gu Z, Thürmann L, Bauer T, Bauer M, et al. Prenatal maternal stress and wheeze in children: novel insights into epigenetic regulation. Sci Rep. 2016; 6:28616. PMID: 27349968.
Article4. Rosa MJ, Just AC, Tamayo Y, Schnaas L, Svensson K, Wright RO, et al. Prenatal and postnatal stress and wheeze in Mexican children: sex-specific differences. Ann Allergy Asthma Immunol. 2016; 116:306–312.e1. PMID: 26822280.5. Chang HY, Suh DI, Yang SI, Kang MJ, Lee SY, Lee E, et al. Prenatal maternal distress affects atopic dermatitis in offspring mediated by oxidative stress. J Allergy Clin Immunol. 2016; 138:468–475.e5. PMID: 27016803.
Article6. Lee A, Mathilda Chiu YH, Rosa MJ, Jara C, Wright RO, Coull BA, et al. Prenatal and postnatal stress and asthma in children: temporal- and sex-specific associations. J Allergy Clin Immunol. 2016; 138:740–747.e3. PMID: 26953156.
Article7. Liu X, Olsen J, Agerbo E, Yuan W, Sigsgaard T, Li J. Prenatal stress and childhood asthma in the offspring: role of age at onset. Eur J Public Health. 2015; 25:1042–1046. PMID: 26116689.
Article8. Bandoli G, von Ehrenstein O, Ghosh JK, Flores ME, Dunkel Schetter C, Ritz B. Prenatal maternal stress and the risk of lifetime wheeze in young offspring: an examination by stressor and maternal ethnicity. J Immigr Minor Health. 2016; 18:987–995. PMID: 26343048.
Article9. Hovland V, Riiser A, Mowinckel P, Carlsen KH, Lødrup Carlsen KC. Early risk factors for pubertal asthma. Clin Exp Allergy. 2015; 45:164–176. PMID: 25220447.
Article10. Chiu YH, Coull BA, Sternthal MJ, Kloog I, Schwartz J, Cohen S, et al. Effects of prenatal community violence and ambient air pollution on childhood wheeze in an urban population. J Allergy Clin Immunol. 2014; 133:713–722.e4. PMID: 24200349.
Article11. Hartwig IR, Sly PD, Schmidt LA, van Lieshout RJ, Bienenstock J, Holt PG, et al. Prenatal adverse life events increase the risk for atopic diseases in children, which is enhanced in the absence of a maternal atopic predisposition. J Allergy Clin Immunol. 2014; 134:160–169. PMID: 25117802.
Article12. Larsen AD, Schlünssen V, Christensen BH, Bonde JP, Obel C, Thulstrup AM, et al. Exposure to psychosocial job strain during pregnancy and odds of asthma and atopic dermatitis among 7-year old children - a prospective cohort study. Scand J Work Environ Health. 2014; 40:639–648. PMID: 25162986.
Article13. Turcotte-Tremblay AM, Lim R, Laplante DP, Kobzik L, Brunet A, King S. Prenatal maternal stress predicts childhood asthma in girls: project ice storm. Biomed Res Int. 2014; 2014:201717. PMID: 24895550.
Article14. Guxens M, Sonnenschein-van der Voort AM, Tiemeier H, Hofman A, Sunyer J, de Jongste JC, et al. Parental psychological distress during pregnancy and wheezing in preschool children: the Generation R Study. J Allergy Clin Immunol. 2014; 133:59–67. 67.e1–67.e12. PMID: 23777854.
Article15. Chiu YH, Coull BA, Cohen S, Wooley A, Wright RJ. Prenatal and postnatal maternal stress and wheeze in urban children: effect of maternal sensitization. Am J Respir Crit Care Med. 2012; 186:147–154. PMID: 22582161.16. Khashan AS, Wicks S, Dalman C, Henriksen TB, Li J, Mortensen PB, et al. Prenatal stress and risk of asthma hospitalization in the offspring: a Swedish population-based study. Psychosom Med. 2012; 74:635–641. PMID: 22753636.17. Fang F, Höglund CO, Arck P, Lundholm C, Långström N, Lichtenstein P, et al. Maternal bereavement and childhood asthma-analyses in two large samples of Swedish children. PLoS One. 2011; 6:e27202. PMID: 22087265.
Article18. Reyes M, Perzanowski MS, Whyatt RM, Kelvin EA, Rundle AG, Diaz DM, et al. Relationship between maternal demoralization, wheeze, and immunoglobulin E among inner-city children. Ann Allergy Asthma Immunol. 2011; 107:42–49.e1. PMID: 21704884.
Article19. Wood RA, Bloomberg GR, Kattan M, Conroy K, Sandel MT, Dresen A, et al. Relationships among environmental exposures, cord blood cytokine responses, allergy, and wheeze at 1 year of age in an inner-city birth cohort (Urban Environment and Childhood Asthma study). J Allergy Clin Immunol. 2011; 127:913–919. 919.e1–919.e6. PMID: 21333343.
Article20. Wen HJ, Wang YJ, Lin YC, Chang CC, Shieh CC, Lung FW, et al. Prediction of atopic dermatitis in 2-yr-old children by cord blood IgE, genetic polymorphisms in cytokine genes, and maternal mentality during pregnancy. Pediatr Allergy Immunol. 2011; 22:695–703. PMID: 21539617.
Article21. Cookson H, Granell R, Joinson C, Ben-Shlomo Y, Henderson AJ. Mothers' anxiety during pregnancy is associated with asthma in their children. J Allergy Clin Immunol. 2009; 123:847–853.e11. PMID: 19348924.
Article22. Sausenthaler S, Rzehak P, Chen CM, Arck P, Bockelbrink A, Schäfer T, et al. Stress-related maternal factors during pregnancy in relation to childhood eczema: results from the LISA Study. J Investig Allergol Clin Immunol. 2009; 19:481–487.23. Suglia SF, Staudenmayer J, Cohen S, Enlow MB, Rich-Edwards JW, Wright RJ. Cumulative stress and cortisol disruption among Black and Hispanic pregnant women in an urban cohort. Psychol Trauma. 2010; 2:326–334. PMID: 21423846.
Article24. Braido F, Baiardini I, Scichilone N, Musarra A, Menoni S, Ridolo E, et al. Illness perception, mood and coping strategies in allergic rhinitis: are there differences among ARIA classes of severity? Rhinology. 2014; 52:66–71. PMID: 24618631.
Article25. Wright RJ, Cohen RT, Cohen S. The impact of stress on the development and expression of atopy. Curr Opin Allergy Clin Immunol. 2005; 5:23–29. PMID: 15643340.
Article26. Grieger JA, Clifton VL, Tuck AR, Wooldridge AL, Robertson SA, Gatford KL. In utero programming of allergic susceptibility. Int Arch Allergy Immunol. 2016; 169:80–92. PMID: 27044002.
Article27. McEwen BS. Central effects of stress hormones in health and disease: Understanding the protective and damaging effects of stress and stress mediators. Eur J Pharmacol. 2008; 583:174–185. PMID: 18282566.
Article28. Wright RJ. Stress-related programming of autonomic imbalance: role in allergy and asthma. Chem Immunol Allergy. 2012; 98:32–47. PMID: 22767056.
Article29. Bellinger DL, Lubahn C, Lorton D. Maternal and early life stress effects on immune function: relevance to immunotoxicology. J Immunotoxicol. 2008; 5:419–444. PMID: 19404876.30. O'Donnell K, O'Connor TG, Glover V. Prenatal stress and neurodevelopment of the child: focus on the HPA axis and role of the placenta. Dev Neurosci. 2009; 31:285–292. PMID: 19546565.31. Corwin EJ, Guo Y, Pajer K, Lowe N, McCarthy D, Schmiege S, et al. Immune dysregulation and glucocorticoid resistance in minority and low income pregnant women. Psychoneuroendocrinology. 2013; 38:1786–1796. PMID: 23541234.
Article32. Teixeira JM, Fisk NM, Glover V. Association between maternal anxiety in pregnancy and increased uterine artery resistance index: cohort based study. BMJ. 1999; 318:153–157. PMID: 9888905.
Article33. Sternberg EM. Neural regulation of innate immunity: a coordinated nonspecific host response to pathogens. Nat Rev Immunol. 2006; 6:318–328. PMID: 16557263.
Article34. Fryer AD, Jacoby DB. Muscarinic receptors and control of airway smooth muscle. Am J Respir Crit Care Med. 1998; 158:S154–S160. PMID: 9817739.
Article35. Entringer S, Buss C, Swanson JM, Cooper DM, Wing DA, Waffarn F, Wadhwa PD. Fetal programming of body composition, obesity, and metabolic function: the role of intrauterine stress and stress biology. J Nutr Metab. 2012; 2012:632548. PMID: 22655178.
Article36. Manti S, Marseglia L, D'Angelo G, Cuppari C, Cusumano E, Arrigo T, et al. “Cumulative Stress”: the effects of maternal and neonatal oxidative stress and oxidative stress-inducible genes on programming of atopy. Oxid Med Cell Longev. 2016; 2016:8651820. PMID: 27504149.
Article37. Nathan C, Cunningham-Bussel A. Beyond oxidative stress: an immunologist's guide to reactive oxygen species. Nat Rev Immunol. 2013; 13:349–361. PMID: 23618831.
Article38. Martino D, Prescott S. Epigenetics and prenatal influences on asthma and allergic airways disease. Chest. 2011; 139:640–647. PMID: 21362650.
Article39. Su RC, Becker AB, Kozyrskyj AL, Hayglass KT. Epigenetic regulation of established human type 1 versus type 2 cytokine responses. J Allergy Clin Immunol. 2008; 121:57–63.e3. PMID: 17980413.
Article40. Oberlander TF, Weinberg J, Papsdorf M, Grunau R, Misri S, Devlin AM. Prenatal exposure to maternal depression, neonatal methylation of human glucocorticoid receptor gene (NR3C1) and infant cortisol stress responses. Epigenetics. 2008; 3:97–106. PMID: 18536531.
Article41. Devlin AM, Brain U, Austin J, Oberlander TF. Prenatal exposure to maternal depressed mood and the MTHFR C677T variant affect SLC6A4 methylation in infants at birth. PLoS One. 2010; 5:e12201. PMID: 20808944.
Article42. Wright RJ. Perinatal stress and early life programming of lung structure and function. Biol Psychol. 2010; 84:46–56. PMID: 20080145.
Article43. Merlot E, Couret D, Otten W. Prenatal stress, fetal imprinting and immunity. Brain Behav Immun. 2008; 22:42–51. PMID: 17716859.
Article44. Bito T, Nishigori C. Impact of reactive oxygen species on keratinocyte signaling pathways. J Dermatol Sci. 2012; 68:3–8. PMID: 22771322.
Article45. Alford SH, Zoratti E, Peterson EL, Maliarik M, Ownby DR, Johnson CC. Parental history of atopic disease: disease pattern and risk of pediatric atopy in offspring. J Allergy Clin Immunol. 2004; 114:1046–1050. PMID: 15536408.
Article46. Xuan W, Marks GB, Toelle BG, Belousova E, Peat JK, Berry G, et al. Risk factors for onset and remission of atopy, wheeze, and airway hyperresponsiveness. Thorax. 2002; 57:104–109. PMID: 11828037.
Article47. Hinz D, Bauer M, Röder S, Olek S, Huehn J, Sack U, et al. Cord blood Tregs with stable FOXP3 expression are influenced by prenatal environment and associated with atopic dermatitis at the age of one year. Allergy. 2012; 67:380–389. PMID: 22187950.
Article48. McCormick CM, Smythe JW, Sharma S, Meaney MJ. Sex-specific effects of prenatal stress on hypothalamic-pituitary-adrenal responses to stress and brain glucocorticoid receptor density in adult rats. Brain Res Dev Brain Res. 1995; 84:55–61. PMID: 7720217.
Article49. Wainstock T, Anteby E, Glasser S, Shoham-Vardi I, Lerner-Geva L. The association between prenatal maternal objective stress, perceived stress, preterm birth and low birthweight. J Matern Fetal Neonatal Med. 2013; 26:973–977. PMID: 23339660.
Article50. Lødrup Carlsen KC, Jaakkola JJ, Nafstad P, Carlsen KH. In utero exposure to cigarette smoking influences lung function at birth. Eur Respir J. 1997; 10:1774–1779. PMID: 9272918.51. Herberth G, Bauer M, Gasch M, Hinz D, Röder S, Olek S, et al. Maternal and cord blood miR-223 expression associates with prenatal tobacco smoke exposure and low regulatory T-cell numbers. J Allergy Clin Immunol. 2014; 133:543–550. PMID: 23978443.
Article52. Zhu Z, Li X, Chen W, Zhao Y, Li H, Qing C, et al. Prenatal stress causes gender-dependent neuronal loss and oxidative stress in rat hippocampus. J Neurosci Res. 2004; 78:837–844. PMID: 15499594.
Article53. Noakes PS, Thomas R, Lane C, Mori TA, Barden AE, Devadason SG, et al. Association of maternal smoking with increased infant oxidative stress at 3 months of age. Thorax. 2007; 62:714–717. PMID: 17356057.
Article54. Kim BJ, Seo JH, Jung YH, Kim HY, Kwon JW, Kim HB, et al. Air pollution interacts with past episodes of bronchiolitis in the development of asthma. Allergy. 2013; 68:517–523. PMID: 23347096.
Article55. Perera F, Tang WY, Herbstman J, Tang D, Levin L, Miller R, et al. Relation of DNA methylation of 5′-CpG island of ACSL3 to transplacental exposure to airborne polycyclic aromatic hydrocarbons and childhood asthma. PLoS One. 2009; 4:e4488. PMID: 19221603.
Article56. Caldji C, Diorio J, Meaney MJ. Variations in maternal care in infancy regulate the development of stress reactivity. Biol Psychiatry. 2000; 48:1164–1174. PMID: 11137058.
Article57. Wright RJ, Finn P, Contreras JP, Cohen S, Wright RO, Staudenmayer J, et al. Chronic caregiver stress and IgE expression, allergen-induced proliferation, and cytokine profiles in a birth cohort predisposed to atopy. J Allergy Clin Immunol. 2004; 113:1051–1057. PMID: 15208584.
Article58. Chida Y, Hamer M, Steptoe A. A bidirectional relationship between psychosocial factors and atopic disorders: a systematic review and meta-analysis. Psychosom Med. 2008; 70:102–116. PMID: 18158379.
Article59. Alati R, O'Callaghan M, Najman JM, Williams GM, Bor W, Lawlor DA. Asthma and internalizing behavior problems in adolescence: a longitudinal study. Psychosom Med. 2005; 67:462–470. PMID: 15911911.
Article60. Collins SM, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol. 2012; 10:735–742. PMID: 23000955.
Article61. Evrensel A, Ceylan ME. Fecal microbiota transplantation and its usage in neuropsychiatric disorders. Clin Psychopharmacol Neurosci. 2016; 14:231–237. PMID: 27489376.
Article62. Davis DJ, Bryda EC, Gillespie CH, Ericsson AC. Microbial modulation of behavior and stress responses in zebrafish larvae. Behav Brain Res. 2016; 311:219–227. PMID: 27217102.
Article63. Azad MB, Kozyrskyj AL. Perinatal programming of asthma: the role of gut microbiota. Clin Dev Immunol. 2012; 2012:932072. PMID: 22110540.
Article64. Noval Rivas M, Burton OT, Wise P, Zhang YQ, Hobson SA, Garcia Lloret M, et al. A microbiota signature associated with experimental food allergy promotes allergic sensitization and anaphylaxis. J Allergy Clin Immunol. 2013; 131:201–212. PMID: 23201093.
Article65. Liu AH. Revisiting the hygiene hypothesis for allergy and asthma. J Allergy Clin Immunol. 2015; 136:860–865. PMID: 26449798.
Article66. Seo JH, Kim HY, Jung YH, Lee E, Yang SI, Yu HS, et al. Interactions between innate immunity genes and early-life risk factors in allergic rhinitis. Allergy Asthma Immunol Res. 2015; 7:241–248. PMID: 25840711.
Article67. Yu J. Gene-environment interactions should be considered in future studies to understand the association between prenatal folate supplementation and asthma development. Allergy Asthma Immunol Res. 2015; 7:523–524. PMID: 26333697.
Article68. Gheorghe CP, Goyal R, Mittal A, Longo LD. Gene expression in the placenta: maternal stress and epigenetic responses. Int J Dev Biol. 2010; 54:507–523. PMID: 19876832.
Article69. Wolf JM, Nicholls E, Chen E. Chronic stress, salivary cortisol, and alpha-amylase in children with asthma and healthy children. Biol Psychol. 2008; 78:20–28. PMID: 18243483.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Maternal Diet during Pregnancy or Lactation on the Development or Prevention of Allergic Diseases in Offspring
- Prenatal Exposure to Drugs and Allergic Diseases in Offspring
- Transcriptomic Alteration in the Brain and Gut of Offspring Following Prenatal Exposure to Corticosterone
- Effects of Maternal Depression on Adolescent Offspring Depression and Anxiety: Mediating Role of Emotional Trauma in a Community-Based Study
- Association between prenatal polycyclic aromatic hydrocarbons and infantile allergic diseases modified by maternal glutathione S-transferase polymorphisms: results from the MOCEH birth cohort