Ann Rehabil Med.
2016 Dec;40(6):1082-1091. 10.5535/arm.2016.40.6.1082.
Risk Factors for Delirium During Acute and Subacute Stages of Various Disorders in Patients Admitted to Rehabilitation Units
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea. ohnsh@hallym.ac.kr
- KMID: 2371341
- DOI: http://doi.org/10.5535/arm.2016.40.6.1082
Abstract
OBJECTIVE
To assess the risk factors for delirium in patients admitted to a rehabilitation unit for acute or subacute neurological or musculoskeletal disorders.
METHODS
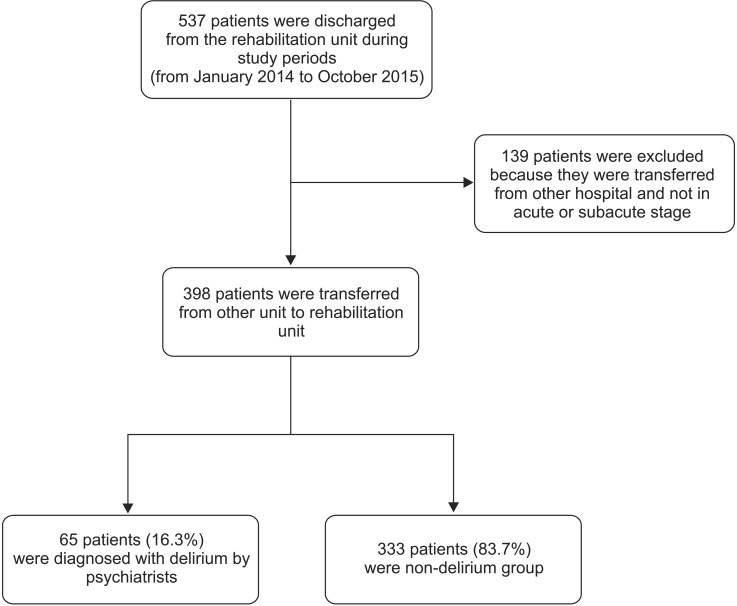
We reviewed the medical records of 537 patients admitted to a rehabilitation unit and selected 398 patients in the acute or subacute stage of various neurological or musculoskeletal disorders. Among them, patients who had suffered from delirium were categorized into the delirium group (n=65), and the other patients were categorized into the non-delirium group (n=333). As potential risk factors for delirium, the patients' diagnosis, underlying disease, demographic data, hospital stay duration, surgery, and laboratory findings were reviewed, and the differences between the two groups with respect to independent risk factors were analyzed.
RESULTS
The average age in the delirium group was higher; the hospital stay and pre-transfer periods were longer. A large proportion of the patients were admitted for musculoskeletal disorders, and many patients had diabetes mellitus, dementia, and depression as underlying diseases. Laboratory tests revealed increases in the white blood cells (WBC), glucose, blood urea nitrogen (BUN), total bilirubin, aspartate transaminase (AST), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels in the delirium group, while the hemoglobin, calcium, phosphorus, protein, albumin, and potassium levels were decreased. Depression, musculoskeletal disorders, traumatic brain injury, elevated WBC, BUN, AST, and CRP levels, and decreased potassium and phosphorus levels were identified as independent risk factors for delirium.
CONCLUSION
Risk factors treatable before delirium onset were identified in rehabilitation patients in acute and subacute stages of various disorders. Early diagnosis and prevention of these risk factors could decrease delirium occurrence and increase rehabilitation effectiveness.
Keyword
MeSH Terms
-
Aspartate Aminotransferases
Bilirubin
Blood Glucose
Blood Sedimentation
Brain Injuries
C-Reactive Protein
Calcium
Delirium*
Dementia
Depression
Diabetes Mellitus
Diagnosis
Early Diagnosis
Humans
Length of Stay
Leukocytes
Medical Records
Nitrogen
Phosphorus
Potassium
Rehabilitation*
Risk Factors*
Urea
Aspartate Aminotransferases
Bilirubin
Blood Glucose
C-Reactive Protein
Calcium
Nitrogen
Phosphorus
Potassium
Urea
Figure
Reference
-
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Association;2013. p. 596–602.2. Ali S, Patel M, Jabeen S, Bailey RK, Patel T, Shahid M, et al. Insight into delirium. Innov Clin Neurosci. 2011; 8:25–34.3. Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998; 13:234–242. PMID: 9565386.4. Kennedy RE, Nakase-Thompson R, Nick TG, Sherer M. Use of the cognitive test for delirium in patients with traumatic brain injury. Psychosomatics. 2003; 44:283–289. PMID: 12832593.
Article5. Fearing MA, Inouye SK. Delirium. Focus. 2009; 7:53–63.
Article6. Clegg A, Siddiqi N, Heaven A, Young J, Holt R. Interventions for preventing delirium in older people in institutional long-term care. Cochrane Database Syst Rev. 2014; (1):CD009537. PMID: 24488526.
Article7. Inouye SK, Bogardus ST Jr, Charpentier PA, Leo-Summers L, Acampora D, Holford TR, et al. A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med. 1999; 340:669–676. PMID: 10053175.
Article8. Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994; 97:278–288. PMID: 8092177.
Article9. Elie M, Cole MG, Primeau FJ, Bellavance F. Delirium risk factors in elderly hospitalized patients. J Gen Intern Med. 1998; 13:204–212. PMID: 9541379.
Article10. Holroyd-Leduc JM, Khandwala F, Sink KM. How can delirium best be prevented and managed in older patients in hospital? CMAJ. 2010; 182:465–470. PMID: 19687107.
Article11. Lin Y, Chen J, Wang Z. Meta-analysis of factors which influence delirium following cardiac surgery. J Card Surg. 2012; 27:481–492. PMID: 22784203.
Article12. Huai J, Ye X. A meta-analysis of critically ill patients reveals several potential risk factors for delirium. Gen Hosp Psychiatry. 2014; 36:488–496. PMID: 24950918.
Article13. van Munster BC, de Rooij SE. Delirium: a synthesis of current knowledge. Clin Med (Lond). 2014; 14:192–195. PMID: 24715133.
Article14. Hwang SW, Kang SW, Kang YG, Choi SG, Lee J, Kim MJ, et al. Risk factors of delirium in elderly inpatients. J Korean Acad Fam Med. 2002; 23:112–121.15. Ko HJ, Kim JH. Dementia and delirium among elderly patients in a general hospital medical ward. J Korean Neuropsychiatr Assoc. 1997; 36:85–91.16. Yu KD, Lee TJ, Suh YW, Chung SH, Kim EY, Kim HY, et al. Delirium in acute elderly care unit: prevalence, clinical characteristics, risk factors and prognostic significance. J Korean Geriatr Soc. 2005; 9:182–189.17. Inouye SK, Charpentier PA. Precipitating factors for delirium in hospitalized elderly persons: predictive model and interrelationship with baseline vulnerability. JAMA. 1996; 275:852–857. PMID: 8596223.
Article18. Pompei P, Foreman M, Rudberg MA, Inouye SK, Braund V, Cassel CK. Delirium in hospitalized older persons: outcomes and predictors. J Am Geriatr Soc. 1994; 42:809–815. PMID: 8046190.
Article19. Tsai MC, Chou SY, Tsai CS, Hung TH, Su JA. Comparison of consecutive periods of 1-, 2-, and 3-year mortality of geriatric inpatients with delirium, dementia, and depression in a consultation-liaison service. Int J Psychiatry Med. 2013; 45:45–57. PMID: 23805603.
Article20. Roche V. Southwestern Internal Medicine Conference. Etiology and management of delirium. Am J Med Sci. 2003; 325:20–30. PMID: 12544081.21. de Lange E, Verhaak PF, van der Meer K. Prevalence, presentation and prognosis of delirium in older people in the population, at home and in long term care: a review. Int J Geriatr Psychiatry. 2013; 28:127–134. PMID: 22513757.
Article22. Caeiro L, Ferro JM, Albuquerque R, Figueira ML. Delirium in the first days of acute stroke. J Neurol. 2004; 251:171–178. PMID: 14991351.
Article23. Inouye SK. Delirium in older persons. N Engl J Med. 2006; 354:1157–1165. PMID: 16540616.
Article24. Francis J, Martin D, Kapoor WN. A prospective study of delirium in hospitalized elderly. JAMA. 1990; 263:1097–1101. PMID: 2299782.
Article25. Turco R, Bellelli G, Morandi A, Gentile S, Trabucchi M. The effect of poststroke delirium on short-term outcomes of elderly patients undergoing rehabilitation. J Geriatr Psychiatry Neurol. 2013; 26:63–68. PMID: 23504308.
Article26. Kim NY, Kim YW. Diagnosis and treatment of post-stroke delirium. Brain Neurorehabil. 2015; 8:59–64.
Article27. Kim CH, Jon DI, Hong HJ, Jung MH, Park JY, Hong N. The risk factors of delirium in orthopedic elderly patients. J Korean Geriatr Psychiatry. 2014; 18:39–43.28. Aldemir M, Ozen S, Kara IH, Sir A, Bac B. Predisposing factors for delirium in the surgical intensive care unit. Crit Care. 2001; 5:265–270. PMID: 11737901.29. Kamel HK, Iqbal MA, Mogallapu R, Maas D, Hoffmann RG. Time to ambulation after hip fracture surgerysurgery: relation to hospitalization outcomes. J Gerontol A Biol Sci Med Sci. 2003; 58:1042–1045. PMID: 14630887.30. Jung SW, Park SC, Rim JS. The risk factor of delirium after transurethral resection of the prostate. Korean J Urol. 2006; 47:953–957.
Article31. Bickel H, Gradinger R, Kochs E, Forstl H. High risk of cognitive and functional decline after postoperative delirium. A three-year prospective study. Dement Geriatr Cogn Disord. 2008; 26:26–31. PMID: 18577850.32. McManus J, Pathansali R, Stewart R, Macdonald A, Jackson S. Delirium post-stroke. Age Ageing. 2007; 36:613–618. PMID: 17965033.
Article33. Rah UW, Kim YH, Ohn SH, Chun MH, Kim MW, Yoo WK, et al. Clinical practice guideline for stroke rehabilitation in Korea 2012. Brain Neurorehabil. 2014; 7(Suppl 1):S1–S75.
Article34. Mysiw WJ, Jackson RD. Differential diagnosis of agitation following brain injury. NeuroRehabilitation. 1995; 5:197–204. PMID: 24525534.
Article35. Dickson LR. Hypoalbuminemia in delirium. Psychosomatics. 1991; 32:317–323. PMID: 1882023.
Article36. Pol RA, van Leeuwen BL, Izaks GJ, Reijnen MM, Visser L, Tielliu IF, et al. C-reactive protein predicts postoperative delirium following vascular surgery. Ann Vasc Surg. 2014; 28:1923–1930. PMID: 25017770.
Article37. Ritchie CW, Newman TH, Leurent B, Sampson EL. The association between C-reactive protein and delirium in 710 acute elderly hospital admissions. Int Psychogeriatr. 2014; 26:717–724. PMID: 24460925.
Article38. Brauer C, Morrison RS, Silberzweig SB, Siu AL. The cause of delirium in patients with hip fracture. Arch Intern Med. 2000; 160:1856–1860. PMID: 10871981.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correction: Risk Factors for Delirium During Acute and Subacute States of Various Disorders in Patients Admitted to Rehabilitation Units
- Characteristics and Risk Factors for Delirium in The Surgical Step-Down Unit
- Risk Factors for Postoperative Delirium after Liver Transplantation in the Intensive Care Unit
- Risk Factors for Delirium in Elderly Patients Visiting an Emergency Department
- Delirium Associated with Olanzapine Therapy in an Elderly Male with Bipolar Affective Disorder