Anesth Pain Med.
2017 Jan;12(1):91-94. 10.17085/apm.2017.12.1.91.
Implantable drug delivery systems with morphine in fibromyalgia: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea. mhsjshgma@gmail.com
- KMID: 2369675
- DOI: http://doi.org/10.17085/apm.2017.12.1.91
Abstract
- The fibromyalgia syndrome (FMS) could be approached by various treatments modalities including education, aerobic exercise, cognitive behavioral therapy, tricyclic antidepressants, serotonin norepinephrine reuptake inhibitors, pregabalin, and so on. If other treatments fail, opioids including morphine should be considered. In this case report, we describe the case of a 44-year-old woman who was diagnosed with FMS three years ago, and suffered from severe intractable pain, side effects from other drugs, and opioid tolerance. Administration of morphine via an implantable drug delivery system resulted in significant improvement in the patient's pain intensity, fibromyalgia impact questionnaire score, and sleep disturbance. Our case demonstrates that an implantable drug delivery system with morphine can be a potential treatment option for refractory fibromyalgia patients.
MeSH Terms
-
Adult
Analgesics, Opioid
Antidepressive Agents, Tricyclic
Cognitive Therapy
Drug Delivery Systems*
Education
Exercise
Female
Fibromyalgia*
Humans
Injections, Spinal
Morphine*
Norepinephrine
Pain, Intractable
Pregabalin
Serotonin
Analgesics, Opioid
Antidepressive Agents, Tricyclic
Morphine
Norepinephrine
Pregabalin
Serotonin
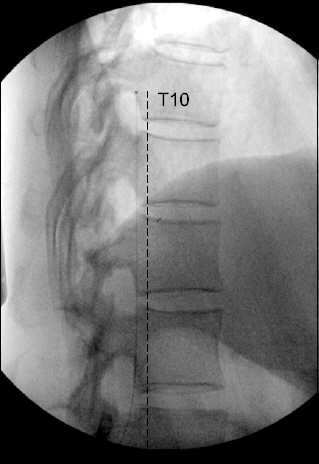
Figure
Reference
-
1. Kim C, Kim H, Kim J. Prevalence of chronic widespread pain and fibromyalgia syndrome: a Korean hospital-based study. Rheumatol Int. 2012; 32:3435–42. DOI: 10.1007/s00296-011-2195-1. PMID: 22057141.2. Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). 2010; 62:600–10. DOI: 10.1002/acr.20140. PMID: 20461783.3. Jay GW, Barkin RL. Fibromyalgia. Dis Mon. 2015; 61:66–111. DOI: 10.1016/j.disamonth.2015.01.002. PMID: 25769552.4. Ver Donck A, Vranken JH, Puylaert M, Hayek S, Mekhail N, Van Zundert J. Intrathecal drug administration in chronic pain syndromes. Pain Pract. 2014; 14:461–76. PMID: 24118774.5. Calandre EP, Rico-Villademoros F, Slim M. An update on pharmacotherapy for the treatment of fibromyalgia. Expert Opin Pharmacother. 2015; 16:1347–68. DOI: 10.1517/14656566.2015.1047343. PMID: 26001183.6. Maestú C, Blanco M, Nevado A, Romero J, Rodríguez-Rubio P, Galindo J, et al. Reduction of pain thresholds in fibromyalgia after very low-intensity magnetic stimulation: a double-blinded, randomized placebo-controlled clinical trial. Pain Res Manag. 2013; 18:e101–6. DOI: 10.1155/2013/270183. PMID: 24308025. PMCID: PMC3917800.7. Robinson RL, Kroenke K, Mease P, Williams DA, Chen Y, D’Souza D, et al. Burden of illness and treatment patterns for patients with fibromyalgia. Pain Med. 2012; 13:1366–76. DOI: 10.1111/j.1526-4637.2012.01475.x. PMID: 22958298.8. Bengtsson M, Bengtsson A, Jorfeldt L. Diagnostic epidural opioid blockade in primary fibromyalgia at rest and during exercise. Pain. 1989; 39:171–80. DOI: 10.1016/0304-3959(89)90004-3.9. Russell IJ, Orr MD, Littman B, Vipraio GA, Alboukrek D, Michalek JE, et al. Elevated cerebrospinal fluid levels of substance P in patients with the fibromyalgia syndrome. Arthritis Rheum. 1994; 37:1593–601. DOI: 10.1002/art.1780371106. PMID: 7526868.10. Kondo I, Marvizon JC, Song B, Salgado F, Codeluppi S, Hua XY, et al. Inhibition by spinal mu- and delta-opioid agonists of afferent-evoked substance P release. J Neurosci. 2005; 25:3651–60. DOI: 10.1523/JNEUROSCI.0252-05.2005. PMID: 15814796.11. Falco FJ, Patel VB, Hayek SM, Deer TR, Geffert S, Zhu J, et al. Intrathecal infusion systems for long-term management of chronic non-cancer pain: an update of assessment of evidence. Pain Physician. 2013; 16(2 Suppl):SE185–216. PMID: 23615891.12. Rhee SM, Choi EJ, Lee PB, Nahm FS. Catheter obstruction of intrathecal drug administration system -a case report-. Korean J Pain. 2012; 25:47–51. DOI: 10.3344/kjp.2012.25.1.47. PMID: 22259717. PMCID: PMC3259138.13. Duarte RV, Raphael JH, Sparkes E, Southall JL, LeMarchand K, Ashford RL. Long-term intrathecal drug administration for chronic nonmalignant pain. J Neurosurg Anesthesiol. 2012; 24:63–70. DOI: 10.1097/ANA.0b013e31822ff779. PMID: 21904220.14. Duarte RV, Raphael JH, Haque MS, Southall JL, Ashford RL. A predictive model for intrathecal opioid dose escalation for chronic non-cancer pain. Pain Physician. 2012; 15:363–9. PMID: 22996848.15. Moulin DE, Inturrisi CE, Foley KM. Cerebrospinal fluid pharmacokinetics of intrathecal morphine sulfate and D-Ala2-D-Leu5-en kephalin. Ann Neurol. 1986; 20:218–22. DOI: 10.1002/ana.410200207. PMID: 3530119.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Totally Implanted Port System for Terminal Cancer Pain: Problems and Complications
- Implantable Intrathecal Drug Delivery Pump in Complex Regional Pain Syndrome Patient : A case report
- Implantable Devices for Sustained, Intravesical Drug Delivery
- An Intrathecally Located Broken Catheter Used for an Intrathecal Drug Delivery System
- Implantation of an Intrathecal Drug Administration System : A report of two cases