Chonnam Med J.
2017 Jan;53(1):64-68. 10.4068/cmj.2017.53.1.64.
Biomarkers Predicting Survival of Sepsis Patients Treated with Continuous Renal Replacement Therapy
- Affiliations
-
- 1Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea. drmsk@jnu.ac.kr
- KMID: 2367341
- DOI: http://doi.org/10.4068/cmj.2017.53.1.64
Abstract
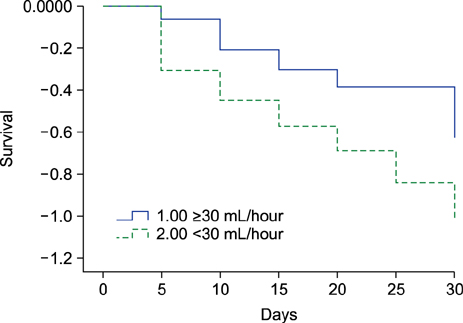
- The present study investigated the prognostic factors predicting survival of patients with sepsis and acute kidney injury (AKI) undergoing continuous renal replacement therapy (CRRT). This retrospective observational study included 165 sepsis patients treated with CRRT. The patients were divided into two groups; the survivor group (n=73, 44.2%) vs. the nonsurvivor group (n=92, 55.8%). AKI was defined by the 2012 Kidney Disease: Improving Global Outcomes Clinical Practice Guidelines. We analyzed medical histories, clinical characteristics and laboratory findings of the enrolled patients when they started CRRT. In addition, we performed binary logistic regression and cox regression analysis. In the survivor group, urine output during the first day was significantly higher compared with the nonsurvivor group (55.7±66.3 vs. 26.6±46.4, p=0.001). Patients with urine output <30 mL/hour during the 1st day showed worse outcomes than ≥30 mL/hour in the logistic regression (hazard ratio 2.464, 95% confidence interval 1.152-5.271, p=0.020) and the cox regression analysis (hazard ratio 1.935, 95% confidence interval 1.147-3.263, p=0.013). In conclusion, urine output may predict survival of septic AKI patients undergoing CRRT. In these patients, urine output <30 mL/hour during the first day was the strongest risk factor for in-hospital mortality.
MeSH Terms
Figure
Reference
-
1. Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992; 101:1644–1655.
Article2. Rangel-Frausto MS, Pittet D, Costigan M, Hwang T, Davis CS, Wenzel RP. The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study. JAMA. 1995; 273:117–123.
Article3. Russell JA, Singer J, Bernard GR, Wheeler A, Fulkerson W, Hudson L, et al. Changing pattern of organ dysfunction in early human sepsis is related to mortality. Crit Care Med. 2000; 28:3405–3411.
Article4. Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001; 29:1303–1310.
Article5. Gerlach H, Toussaint S. Sepsis therapy--Why change-management of sepsis can lower its lethality. Anasthesiol Intensivmed Notfallmed Schmerzther. 2006; 41:614–624.6. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003; 348:1546–1554.
Article7. Annane D, Aegerter P, Jars-Guincestre MC, Guidet B. CUB-Réa Network. Current epidemiology of septic shock: the CUB-Réa Network. Am J Respir Crit Care Med. 2003; 168:165–172.8. Brivet FG, Kleinknecht DJ, Loirat P, Landais PJ. Acute renal failure in intensive care units--causes, outcome, and prognostic factors of hospital mortality; a prospective, multicenter study. French Study Group on Acute Renal Failure. Crit Care Med. 1996; 24:192–198.
Article9. Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, et al. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002; 30:2051–2058.
Article10. Druml W. Acute renal failure is not a "cute" renal failure. Intensive Care Med. 2004; 30:1886–1890.
Article11. Joannidis M, Metnitz PG. Epidemiology and natural history of acute renal failure in the ICU. Crit Care Clin. 2005; 21:239–249.
Article12. Neveu H, Kleinknecht D, Brivet F, Loirat P, Landais P. Prognostic factors in acute renal failure due to sepsis. Results of a prospective multicentre study. The French Study Group on Acute Renal Failure. Nephrol Dial Transplant. 1996; 11:293–299.
Article13. Bellomo R, Kellum JA, Ronco C. Defining and classifying acute renal failure: from advocacy to consensus and validation of the RIFLE criteria. Intensive Care Med. 2007; 33:409–413.
Article14. Section 2: AKI Definition. Kidney Int Suppl (2011). 2012; 2:19–36.15. Ali T, Khan I, Simpson W, Prescott G, Townend J, Smith W, et al. Incidence and outcomes in acute kidney injury: a comprehensive population-based study. J Am Soc Nephrol. 2007; 18:1292–1298.
Article16. Thakar CV, Christianson A, Freyberg R, Almenoff P, Render ML. Incidence and outcomes of acute kidney injury in intensive care units: a Veterans Administration study. Crit Care Med. 2009; 37:2552–2558.
Article17. Joannidis M, Metnitz B, Bauer P, Schusterschitz N, Moreno R, Druml W, et al. Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med. 2009; 35:1692–1702.
Article18. Mandelbaum T, Lee J, Scott DJ, Mark RG, Malhotra A, Howell MD, et al. Empirical relationships among oliguria, creatinine, mortality, and renal replacement therapy in the critically ill. Intensive Care Med. 2013; 39:414–419.
Article19. Coca SG, Yalavarthy R, Concato J, Parikh CR. Biomarkers for the diagnosis and risk stratification of acute kidney injury: a systematic review. Kidney Int. 2008; 73:1008–1016.
Article20. Charlton JR, Portilla D, Okusa MD. A basic science view of acute kidney injury biomarkers. Nephrol Dial Transplant. 2014; 29:1301–1311.
Article21. Alge JL, Arthur JM. Biomarkers of AKI: a review of mechanistic relevance and potential therapeutic implications. Clin J Am Soc Nephrol. 2015; 10:147–155.
Article22. Soong J, Soni N. Sepsis: recognition and treatment. Clin Med (Lond). 2012; 12:276–280.
Article23. Wald R, Deshpande R, Bell CM, Bargman JM. Survival to discharge among patients treated with continuous renal replacement therapy. Hemodial Int. 2006; 10:82–87.
Article24. Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, et al. Discontinuation of continuous renal replacement therapy: a post hoc analysis of a prospective multicenter observational study. Crit Care Med. 2009; 37:2576–2582.
Article25. Kawarazaki H, Uchino S, Tokuhira N, Ohnuma T, Namba Y, Katayama S, et al. Who may not benefit from continuous renal replacement therapy in acute kidney injury? Hemodial Int. 2013; 17:624–632.
Article26. Wu VC, Ko WJ, Chang HW, Chen YW, Lin YF, Shiao CC, et al. Risk factors of early redialysis after weaning from postoperative acute renal replacement therapy. Intensive Care Med. 2008; 34:101–108.
Article27. Ostermann M, Chang RW. Correlation between parameters at initiation of renal replacement therapy and outcome in patients with acute kidney injury. Crit Care. 2009; 13:R175.
Article28. Cerdá J, Cerdá M, Kilcullen P, Prendergast J. In severe acute kidney injury, a higher serum creatinine is paradoxically associated with better patient survival. Nephrol Dial Transplant. 2007; 22:2781–2784.
Article29. Stevens LA, Levey AS. Measured GFR as a confirmatory test for estimated GFR. J Am Soc Nephrol. 2009; 20:2305–2313.
Article30. Mehta RL. Acute kidney injury: Urine output in AKI--the canary in the coal mine? Nat Rev Nephrol. 2013; 9:568–570.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Update on Sepsis Biomarkers
- Continuous Renal Replacement Therapy in Children
- Eosinophil count and neutrophil-to-lymphocyte count ratio as biomarkers for predicting early-onset neonatal sepsis
- Overview of Pediatric Continuous Renal Replacement Therapy in Acute Kidney Injury
- Renal Replacement Therapies on the Outcomes of Acute Renal Failure Patients in ICU