J Korean Med Sci.
2016 Jan;31(1):139-146. 10.3346/jkms.2016.31.1.139.
The Effect of Emergency Medical Service Use and Inter-hospital Transfer on Prehospital Delay among Ischemic Stroke Patients: A Multicenter Observational Study
- Affiliations
-
- 1Genome Epidemiology, Department of Epidemiology, Graduate School of Public Health, Seoul National University, Seoul, Korea.
- 2Laboratory of Emergency Medical Service, Seoul National University Hospital Biomedical Research Institute, Seoul, Korea. arendt75@gmail.com
- 3Department of Emergency Medicine, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea.
- 4Department of Emergency Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2360004
- DOI: http://doi.org/10.3346/jkms.2016.31.1.139
Abstract
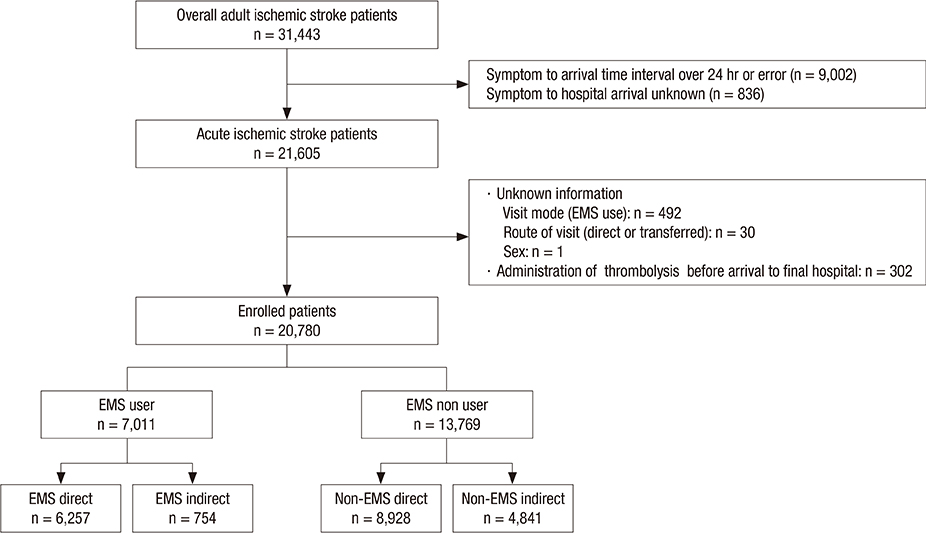
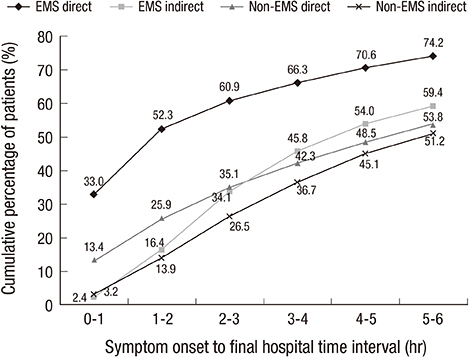
- The time between symptom onset and arrival at an emergency department (ED) (S2D) is a crucial time for optimal intravenous reperfusion care for ischemic stroke. We aimed to analyze the effect of emergency medical services (EMS) utilization and inter-hospital transfer on S2D in Korea. Ischemic stroke patients were prospectively enrolled from November 2007 to December 2012 in 23 tertiary and teaching hospital EDs in Korea. Of 31,443 adult ischemic stroke patients, 20,780 were categorized into 4 groups based on modes of EMS utilization and inter-hospital transfer: direct transport to destination ED by EMS (EMS direct; n=6,257, 30.1%), transfer after transport to another ED by EMS (EMS indirect; n=754, 3.6%), direct transport to the ED without using EMS (non-EMS direct; n=8,928, 43.0%), and transfer after visiting another hospital without using EMS (non-EMS indirect; n=4,841, 23.3%). Our primary outcome variable was of S2D within 2 hr (S2D < or =2 hr) and found that 30.8% of all patients and 52.3%, 16.4%, 25.9%, and 13.9% of EMS direct, EMS indirect, non-EMS direct, and non-EMS indirect, respectively, achieved S2D < or =2 hr. Adjusted odds ratio for S2D < or =2 hr were 6.56 (95% confidence interval [CI], 5.94-7.24), 2.27 (95% CI, 2.06-2.50), and 1.07 (95% CI, 0.87-1.33) for EMS direct, non-EMS direct, and EMS indirect, respectively. Patients directly transported to destination hospitals by the EMS show the highest proportion of therapeutic time window for optimal care in ischemic stroke.
MeSH Terms
Figure
Reference
-
1. WHO publishes definitive atlas on global heart disease and stroke epidemic. Indian J Med Sci. 2004; 58:405–406.2. Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013; 127:e6–e245.3. Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995; 333:1581–1588.4. How do stroke units improve patient outcomes? A collaborative systematic review of the randomized trials Stroke Unit Trialists Collaboration. Stroke. 1997; 28:2139–2144.5. Marler JR, Tilley BC, Lu M, Brott TG, Lyden PC, Grotta JC, Broderick JP, Levine SR, Frankel MP, Horowitz SH, et al. Early stroke treatment associated with better outcome: the NINDS rt-PA stroke study. Neurology. 2000; 55:1649–1655.6. Barber PA, Zhang J, Demchuk AM, Hill MD, Buchan AM. Why are stroke patients excluded from TPA therapy? An analysis of patient eligibility. Neurology. 2001; 56:1015–1020.7. Demaerschalk BM, Bobrow BJ, Paulsen M. Development of a metropolitan matrix of primary stroke centers: the Phoenix experience. Stroke. 2008; 39:1246–1253.8. Johnston SC, Fung LH, Gillum LA, Smith WS, Brass LM, Lichtman JH, Brown AN, Wang DZ. Utilization of intravenous tissue-type plasminogen activator for ischemic stroke at academic medical centers: the influence of ethnicity. Stroke. 2001; 32:1061–1068.9. Reed SD, Cramer SC, Blough DK, Meyer K, Jarvik JG, Wang DZ. Treatment with tissue plasminogen activator and inpatient mortality rates for patients with ischemic stroke treated in community hospitals. Stroke. 2001; 32:1832–1840.10. Rudd AG, Hoffman A, Grant R, Campbell JT, Lowe D. Stroke thrombolysis in England, Wales and Northern Ireland: how much do we do and how much do we need? J Neurol Neurosurg Psychiatry. 2011; 82:14–19.11. Saver JL, Smith EE, Fonarow GC, Reeves MJ, Zhao X, Olson DM, Schwamm LH. GWTG-Stroke Steering Committee and Investigators. The "golden hour" and acute brain ischemia: presenting features and lytic therapy in >30,000 patients arriving within 60 minutes of stroke onset. Stroke. 2010; 41:1431–1439.12. Berglund A, Svensson L, Sjostrand C, von Arbin M, von Euler M, Wahlgren N, Engerstrom L, Hojeberg B, Kall TB, Mjornheim S, et al. Higher prehospital priority level of stroke improves thrombolysis frequency and time to stroke unit: the Hyper Acute STroke Alarm (HASTA) study. Stroke. 2012; 43:2666–2670.13. Kim HJ, Ahn JH, Kim SH, Hong ES. Factors associated with prehospital delay for acute stroke in Ulsan, Korea. J Emerg Med. 2011; 41:59–63.14. Kim YS, Park SS, Bae HJ, Cho AH, Cho YJ, Han MK, Heo JH, Kang K, Kim DE, Kim HY, et al. Stroke awareness decreases prehospital delay after acute ischemic stroke in Korea. BMC Neurol. 2011; 11:2.15. Sun CH, Nogueira RG, Glenn BA, Connelly K, Zimmermann S, Anda K, Camp D, Frankel MR, Belagaje SR, Anderson AM, et al. "Picture to puncture": a novel time metric to enhance outcomes in patients transferred for endovascular reperfusion in acute ischemic stroke. Circulation. 2013; 127:1139–1148.16. Ahn KO, Shin SD, Suh GJ, Cha WC, Song KJ, Kim SJ, Lee EJ, Ong ME. Epidemiology and outcomes from non-traumatic out-of-hospital cardiac arrest in Korea: A nationwide observational study. Resuscitation. 2010; 81:974–981.17. Ministry of Public Safety and Security. The standard protocols for 119 emergency medical service providers. accessed on 5 December 2015. Available at http://www.prism.go.kr/homepage/researchCommon/retrieveResearchDetailPopup.do?research_id=1660000-201200020.18. Morris DL, Rosamond W, Madden K, Schultz C, Hamilton S. Prehospital and Emergency Department Delays After Acute Stroke: The Genentech Stroke Presentation Survey. Stroke. 2000; 31:2585–2590.19. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, Khatri P, McMullan PW Jr, Qureshi AI, Rosenfield K, et al. American Heart Association Stroke C, Council on Cardiovascular N, Council on Peripheral Vascular D, Council on Clinical C. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947.20. George MG, Tong X, McGruder H, Yoon P, Rosamond W, Winquist A, Hinchey J, Wall HK, Pandey DK. Centers for Disease C, Prevention. Paul Coverdell National Acute Stroke Registry Surveillance - four states, 2005-2007. MMWR Surveill Summ. 2009; 58:1–23.21. Kwan J, Hand P, Sandercock P. A systematic review of barriers to delivery of thrombolysis for acute stroke. Age Ageing. 2004; 33:116–121.22. Harraf F, Sharma AK, Brown MM, Lees KR, Vass RI, Kalra L. A multicentre observational study of presentation and early assessment of acute stroke. BMJ. 2002; 325:17.23. Lacy CR, Suh DC, Bueno M, Kostis JB. Delay in presentation and evaluation for acute stroke: Stroke Time Registry for Outcomes Knowledge and Epidemiology (S.T.R.O.K.E.). Stroke. 2001; 32:63–69.24. Wein TH, Staub L, Felberg R, Hickenbottom SL, Chan W, Grotta JC, Demchuk AM, Groff J, Bartholomew LK, Morgenstern LB. Activation of emergency medical services for acute stroke in a nonurban population: the T.L.L. Temple Foundation Stroke Project. Stroke. 2000; 31:1925–1928.25. Kim YS, Park SS, Bae HJ, Heo JH, Kwon SU, Lee BC, Lee SH, Oh CW, Yoon BW. Public awareness of stroke in Korea: a population-based national survey. Stroke. 2012; 43:1146–1149.26. Prabhakaran S, Ward E, John S, Lopes DK, Chen M, Temes RE, Mohammad Y, Lee VH, Bleck TP. Transfer delay is a major factor limiting the use of intra-arterial treatment in acute ischemic stroke. Stroke. 2011; 42:1626–1630.27. Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field. Prospective validation of the Los Angeles prehospital stroke screen (LAPSS). Stroke. 2000; 31:71–76.28. Brandler ES, Sharma M, Sinert RH, Levine SR. Prehospital stroke scales in urban environments: a systematic review. Neurology. 2014; 82:2241–2249.29. Studnek JR, Asimos A, Dodds J, Swanson D. Assessing the validity of the Cincinnati prehospital stroke scale and the medic prehospital assessment for code stroke in an urban emergency medical services agency. Prehosp Emerg Care. 2013; 17:348–353.30. Ahn KO, Shin SD, Park CB, Song KJ, Hong KJ, Lee SC, Moon S, Cha WC. Validation of pre-hospital stroke screens by ambulance service personnel: A prospective observation study. J Korean Soc Emerg Med. 2013; 24:272–278.31. Nedeltchev K, Arnold M, Brekenfeld C, Isenegger J, Remonda L, Schroth G, Mattle HP. Pre- and in-hospital delays from stroke onset to intra-arterial thrombolysis. Stroke. 2003; 34:1230–1234.32. Lim CD, Ryoo HW, Hwang YH, Lee MJ, Shin SJ, Ahn JY, Kim JK, Park JB, Seo KS. Urban-rural gap in the prehospital delay of acute stroke patients. J Korean Soc Emerg Med. 2013; 24:664–673.33. Lee D, Ahn KO, Shin SD, Park HA, Roa YS, Cha WC, Lee SC. Impacts of urbanization on delay in transferred ischemic stroke patients. J Korean Soc Emerg Med. 2014; 25:392–400.34. Schroeder EB, Rosamond WD, Morris DL, Evenson KR, Hinn AR. Determinants of use of emergency medical services in a population with stroke symptoms: the Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke. 2000; 31:2591–2596.35. Rosamond WD, Gorton RA, Hinn AR, Hohenhaus SM, Morris DL. Rapid response to stroke symptoms: the Delay in Accessing Stroke Healthcare (DASH) study. Acad Emerg Med. 1998; 5:45–51.36. Jin H, Zhu S, Wei JW, Wang J, Liu M, Wu Y, Wong LK, Cheng Y, Xu E, Yang Q, et al. Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke. 2012; 43:362–370.37. Jorgensen HS, Nakayama H, Reith J, Raaschou HO, Olsen TS. Factors delaying hospital admission in acute stroke: the Copenhagen Stroke Study. Neurology. 1996; 47:383–387.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Influencing Prehospital and Inhospital Time Delays for Ischemic Stroke Patients
- Prehospital Delay Factors After Stroke and Paramedic Identification of Stroke Patients in a Metropolitan City Emergency Medical Service System
- Factors Related to Prehospital Delay Time in Patients with Stroke
- Urban-Rural Gap in the Prehospital Delay of Acute Stroke Patients
- Prehospital Notification from the Emergency Medical Service Reduces the Transfer and Intra-Hospital Processing Times for Acute Stroke Patients