J Korean Ophthalmol Soc.
2014 Jul;55(7):1099-1105.
A Case of Optic Disc Hemorrhage Associated with Buried Optic Nerve Head Drusen
- Affiliations
-
- 1Department of Ophthalmology, Daegu Fatima Hospital, Daegu, Korea. mjmom99@naver.com
Abstract
- PURPOSE
We report a case of optic disc hemorrhage associated with buried optic nerve head drusen in a pediatric patient.
CASE SUMMARY
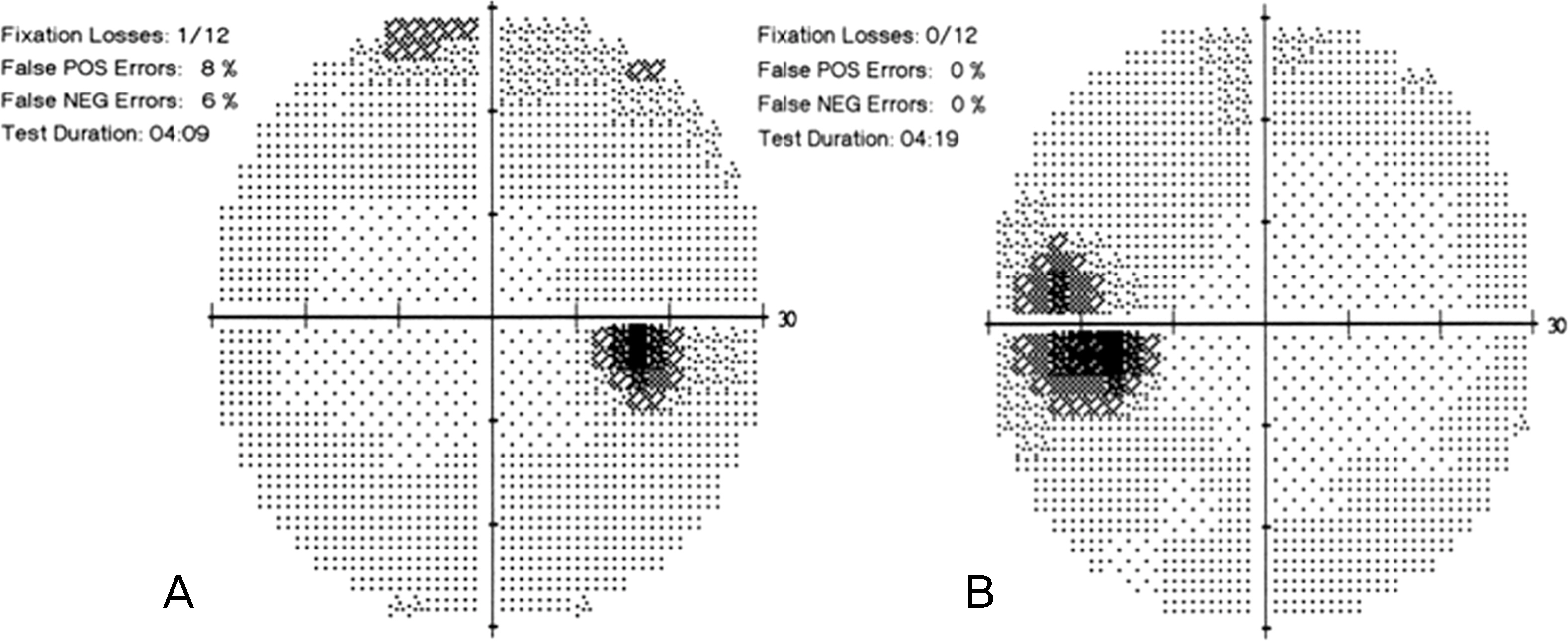
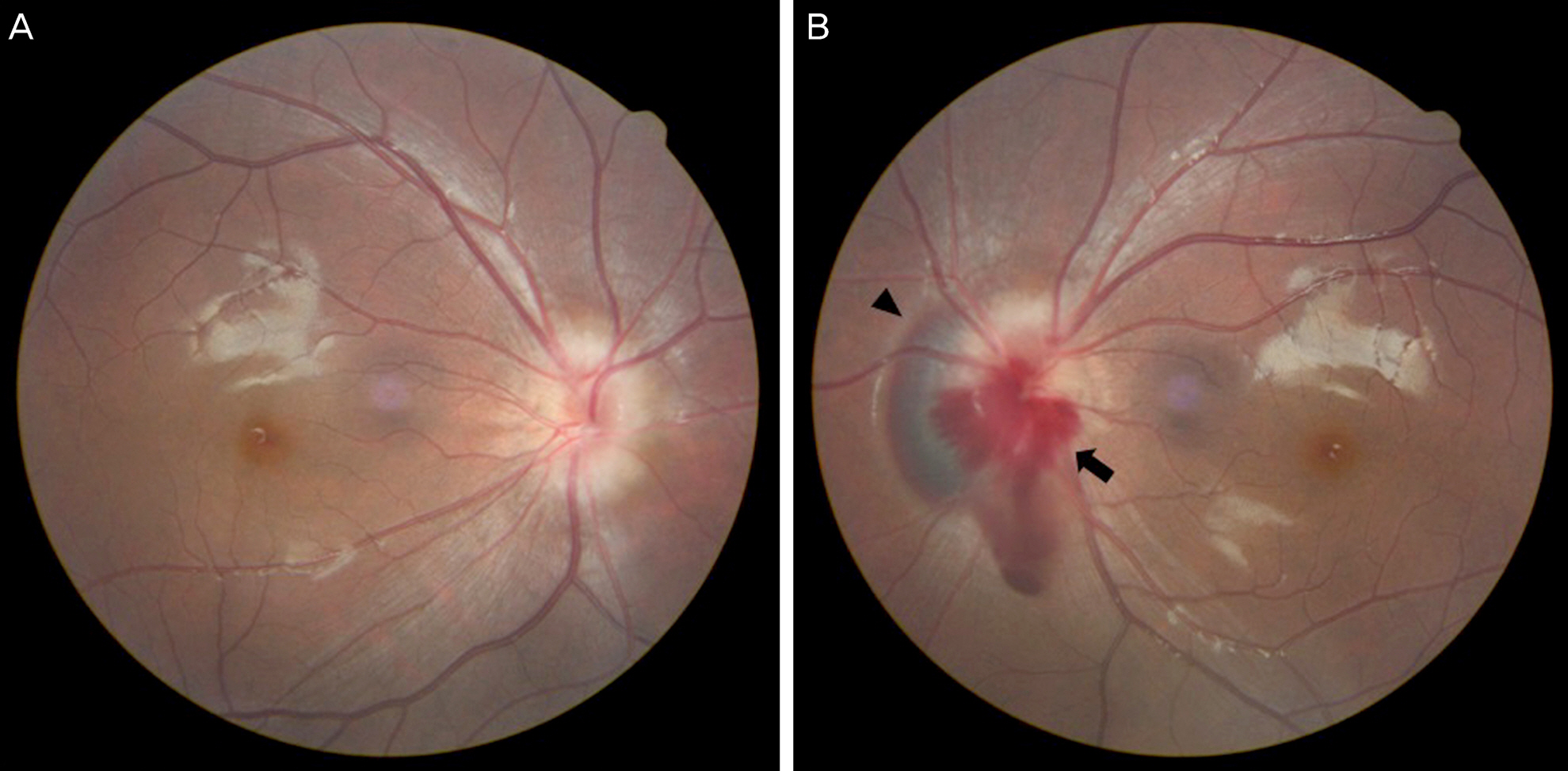
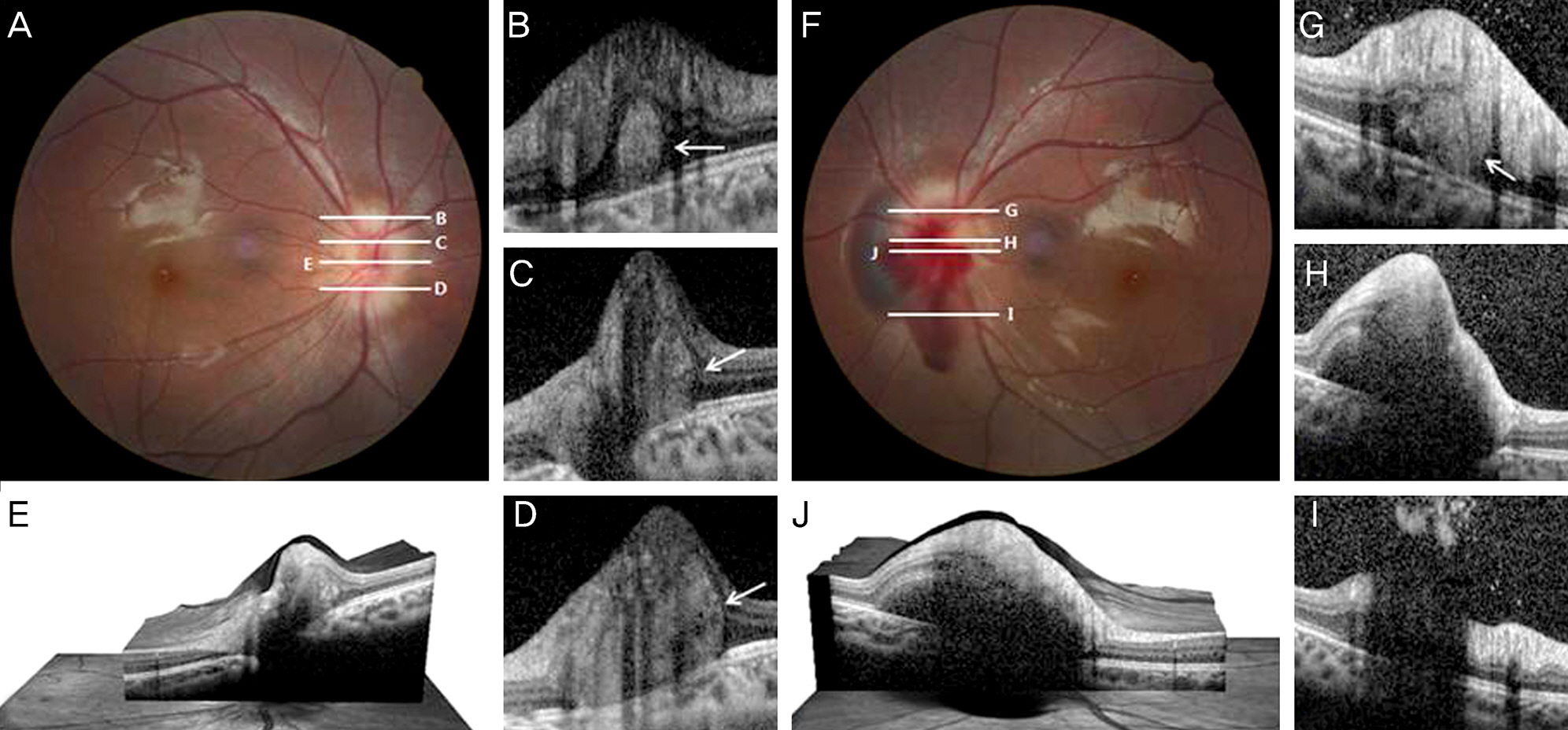
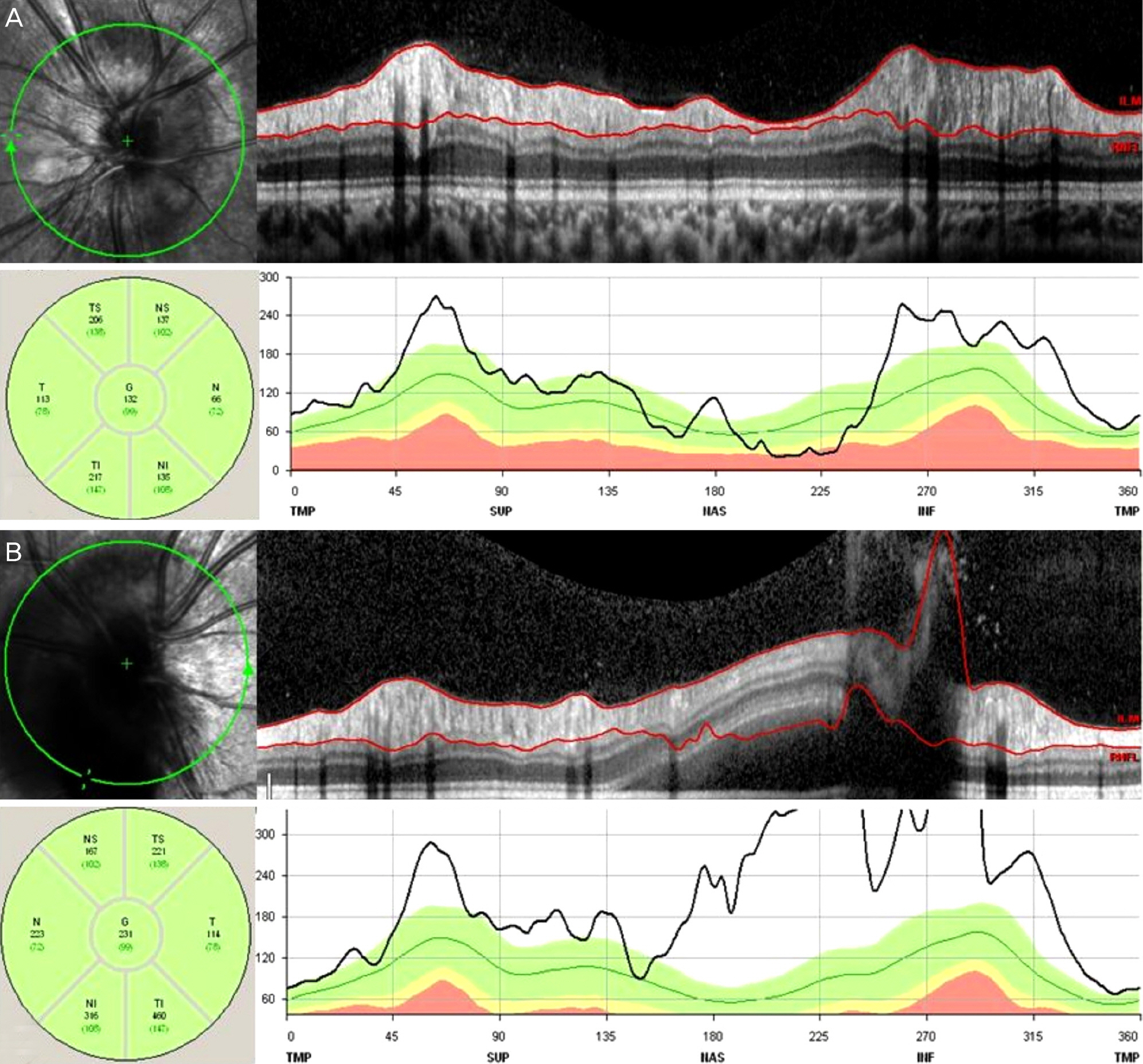
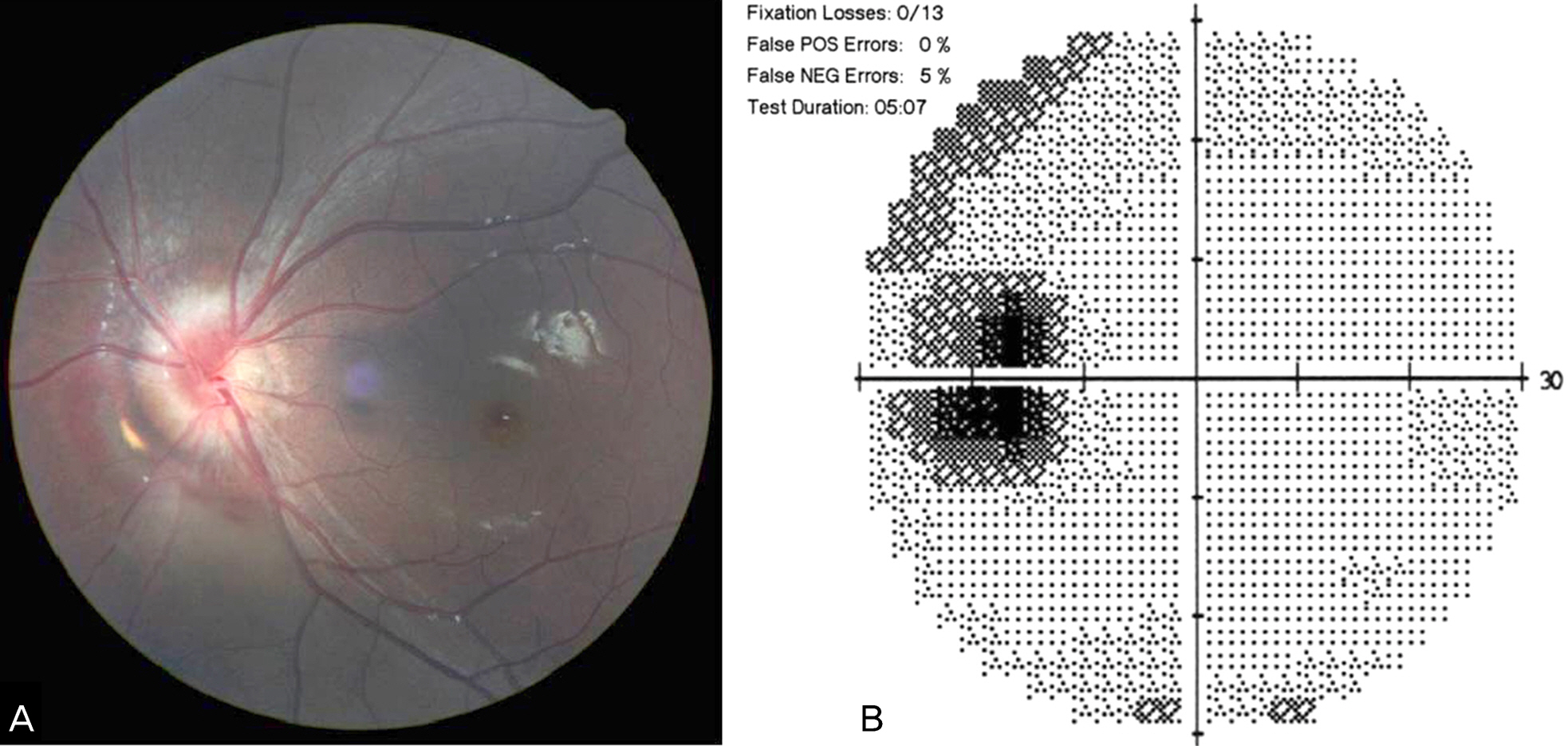
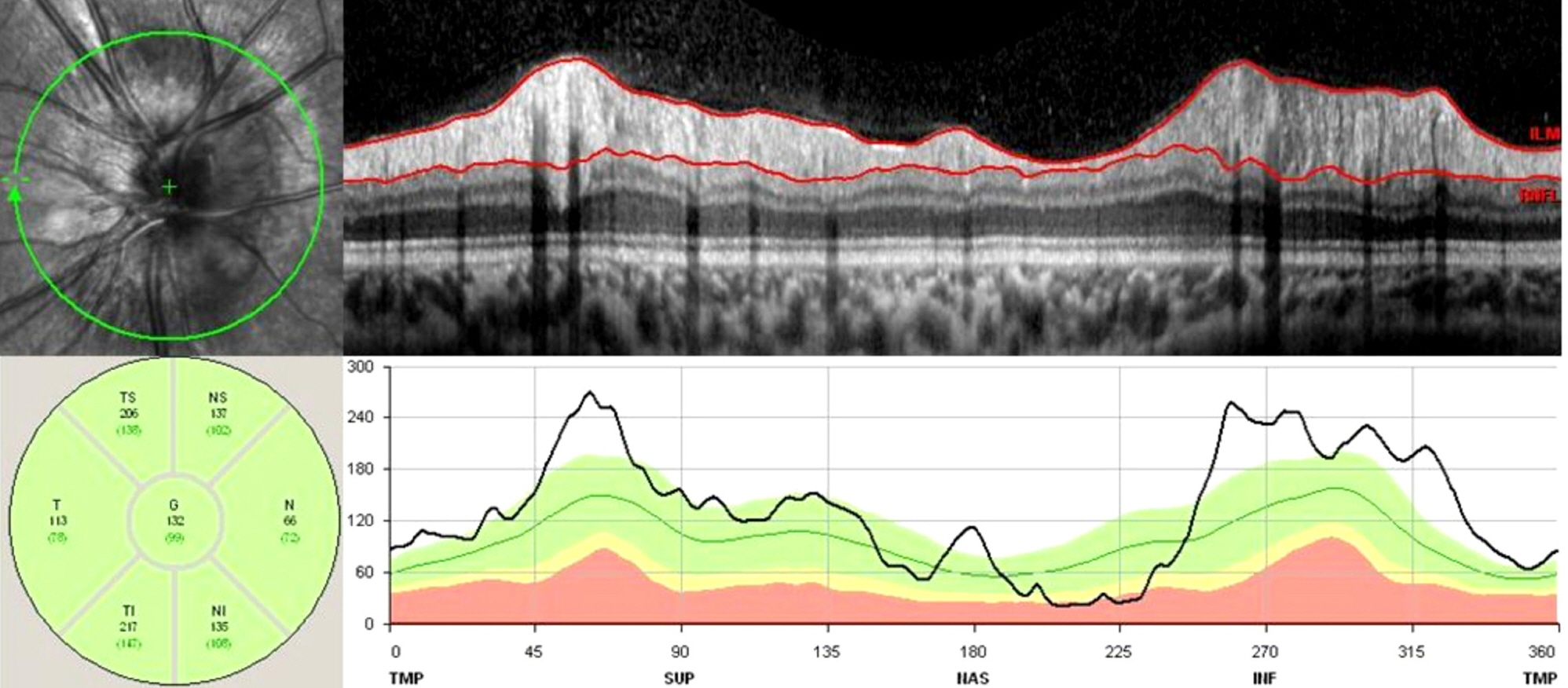
A 10-year-old female visited our clinic with a floating sensation in her left eye, 2 days in duration. Best corrected visual acuity was 1.0 in both eyes. Intraocular pressure, light reflex, relative afferent pupillary defect and color vision were normal. The patient showed a small optic disc with blurred, irregular margins in both eyes, and optic disc hemorrhage in the left eye on fundus examination. Visual field examination revealed an enlarged blind spot in the left eye. To achieve correct diagnosis, brain MRI was performed and revealed normal findings. On spectral-domain optical coherence tomography (OCT), hyper-reflective and heterogeneous mass like lesions were found with buried optic nerve head drusen.
CONCLUSIONS
In general, optic nerve head drusen, has a good prognosis; however, visual field defects or hemorrhagic complications can occur, therefore, correct diagnosis and regular follow-up are necessary.
MeSH Terms
Figure
Reference
-
References
1. Lee KM, Woo SJ, Hwang JM. Morphologic characteristics of optic nerve head drusen on spectral-domain optical coherence tomography. Am J Ophthalmol. 2013; 155:1139–47.
Article2. Lee KM, Woo SJ, Hwang JM. Differentiation of optic nerve head drusen and optic disc edema with spectral-domain optical coherence tomography. Ophthalmology. 2011; 118:971–7.
Article3. Neffendorf JE, Mulholland C, Quinlan M, Lyons CJ. Disc drusen complicated by optic disc hemorrhage in childhood. Can J Ophthalmol. 2010; 45:537–8.
Article4. Auw-Haedrich C, Staubach F, Witschel H. Optic disk drusen. Surv Ophthalmol. 2002; 47:515–32.
Article5. Sanders TE, Gay AJ, Newman M. Hemorrhagic complications of drusen of the optic disk. Am J Ophthalmol. 1971; 71:204–17.
Article6. Mullie MA, Sanders MD. Scleral canal size and optic nerve head drusen. Am J Ophthalmol. 1985; 99:356–9.
Article7. Harris MJ, Fine SL, Owens SL. Hemorrhagic complications of optic nerve drusen. Am J Ophthmol. 1981; 92:70–6.
Article8. Johnson LN, Diehl ML, Hamm CW, et al. Differentiating optic disc edema from optic nerve head drusen on optical coherence tomography. Arch Ophthalmol. 2009; 127:45–9.
Article9. Grippo TM, Shihadeh WA, Schargus M, et al. Optic nerve head drusen and visual field loss in normotensive and hypertensive eyes. J Glaucoma. 2008; 17:100–4.
Article10. Chaudhry NA, Lavaque AJ, Shah A, Liggett PE. Photodynamic therapy for choroidal neovascular memebrane secondary to optic nerve drusen. Ophthalmic Surg Lasers Imaging. 2005; 36:70–2.11. Knape RM, Zavaleta EM, Clark CL 3rd, et al. Intravitreal bevacizumab treatment of bilateral peripapillary choroidal neo- vascularization from optic nerve head drusen. J AAPOS. 2011; 15:87–90.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bilateral Optic Disc Drusen Mimicking Papilledema
- Anti-Vascular Endothelial Growth Factor Therapy for Choroidal Neovascularization Secondary to Optic Nerve Head Drusen
- Optic Nerve Head Drusen Mimicking Optic Nerve Tumor
- Optical Coherence Tomography Findings of Optic Nerve Head Drusen in Children and Adolescents
- Comparison of Optic Disc Appearance in Anterior ischemic optic neuropathy and Optic neuritis