J Korean Ophthalmol Soc.
2012 Jun;53(6):761-766.
Effects of Transient Prone Position on Vault and Anterior Chamber Angle in ICL Implanted Patients
- Affiliations
-
- 1B&VIIT Eye Center, Seoul, Korea. hunny502@hanmail.net
Abstract
- PURPOSE
To evaluate the effects of transient prone position on vault and anterior chamber angle parameters in ICL implanted patients.
METHODS
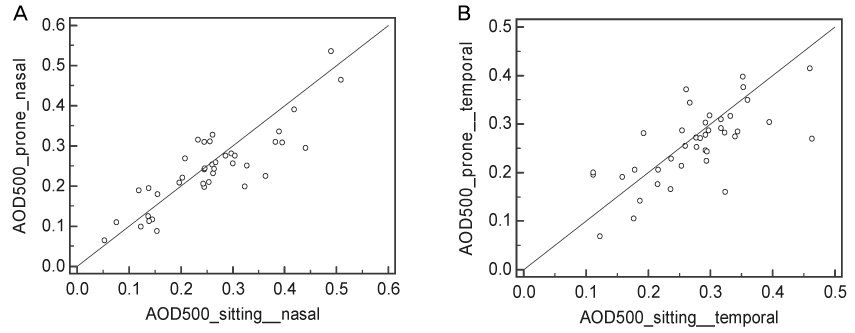
40 eyes of 20 ICL implanted patients with at least 1 month of follow-up were included in the present study. The central ICL vault and anterior chamber parameters including angle opening distance at 500 (AOD500) were measured with the Visante anterior segment optical coherence tomography (OCT) (Carl Zeiss, Dublin, CA) in both the sitting and prone positions by tilting the OCT 90 degrees in the vertical axis and having the patient fixate downwards towards the floor.
RESULTS
The mean central vault was 0.55 +/- 0.21 mm (SD) and 0.59 +/- 0.21 mm (SD) in the sitting and prone positions, respectively (p < 0.0001). The nasal and temporal AOD500 were 0.26 +/- 0.11 mm and 0.28 +/- 0.08 mm, respectively in the sitting position, which decreased to 0.24 +/- 0.10 mm and 0.26 +/- 0.08 mm in the prone position, however, both were not statistically significant (p = 0.08, p = 0.09). AOD500 was inversely correlated with vault (r = -0.47; p = 0.0024). There were no significant correlations between increase of vault and anterior chamber depth or white to white nor ICL vault.
CONCLUSIONS
Transient prone positioning of ICL implanted patients can induce a significant increase in ICL vault.
Keyword
MeSH Terms
Figure
Reference
-
1. Ieong A, Hau SC, Rubin GS, Allan BD. Quality of life in high myopia before and after implantable Collamer lens implantation. Ophthalmology. 2010. 117:2295–2300.2. Rayner SA, Bhikoo R, Gray T. Spherical implantable collamer lenses for myopia and hyperopia: 126 eyes with 1-year follow up. Clin Experiment Ophthalmol. 2010. 38:21–26.3. Kamiya K, Shimizu K, Igarashi A, et al. Four-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Arch Ophthalmol. 2009. 127:845–850.4. Khalifa YM, Moshirfar M, Mifflin MD, et al. Cataract development associated with collagen copolymer posterior chamber phakic intraocular lenses: clinicopathological correlation. J Cataract Refract Surg. 2010. 36:1768–1774.5. Khalifa YM, Goldsmith J, Moshirfar M. Bilateral explantation of Visian Implantable Collamer Lenses secondary to bilateral acute angle closure resulting from a non-pupillary block mechanism. J Refract Surg. 2010. 26:991–994.6. Chung TY, Park SC, Lee MO, et al. Changes in iridocorneal angle structure and trabecular pigmentation with STAAR implantable collamer lens during 2 years. J Refract Surg. 2009. 25:251–258.7. Kojima T, Maeda M, Yoshida Y, et al. Posterior chamber phakic implantable collamer lens: changes in vault during 1 year. J Refract Surg. 2010. 26:327–332.8. Alfonso JF, Lisa C, Abdelhamid A, et al. Three-year follow-up of subjective vault following myopic implantable collamer lens implantation. Graefes Arch Clin Exp Ophthalmol. 2010. 248:1827–1835.9. Kamiya K, Shimizu K, Kawamorita T. Changes in vaulting and the effect on refraction after phakic posterior chamber intraocular lens implantation. J Cataract Refract Surg. 2009. 35:1582–1586.10. Petternel V, Köppl CM, Dejaco-Ruhswurm I, et al. Effect of accommodation and pupil size on the movement of a posterior chamber lens in the phakic eye. Ophthalmology. 2004. 111:325–331.11. Lindland A, Heger H, Kugelberg M, Zetterström C. Vaulting of myopic and toric Implantable Collamer Lenses during accommodation measured with Visante optical coherence tomography. Ophthalmology. 2010. 117:1245–1250.12. Bechmann M, Ullrich S, Thiel MJ, et al. Imaging of posterior chamber phakic intraocular lens by optical coherence tomography. J Cataract Refract Surg. 2002. 28:360–363.13. Mérula RV, Cronemberger S, Diniz Filho A, Calixto N. New comparative ultrasound biomicroscopic findings between fellow eyes of acute angle closure and glaucomatous eyes with narrow angle. Arq Bras Oftalmol. 2008. 71:793–798.14. Marchini G, Pagliarusco A, Toscano A, et al. Ultrasound biomicroscopic and conventional ultrasonographic study of ocular dimensions in primary angle-closure glaucoma. Ophthalmology. 1998. 105:2091–2098.15. Ramani KK, Mani B, Ronnie G, et al. Gender variation in ocular biometry and ultrasound biomicroscopy of primary angle closure suspects and normal eyes. J Glaucoma. 2007. 16:122–128.16. Friedman DS, Gazzard G, Foster P, et al. Ultrasonographic biomicroscopy, Scheimpflug photography, and novel provocative tests in contralateral eyes of Chinese patients initially seen with acute angle closure. Arch Ophthalmol. 2003. 121:633–642.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effect of Lens Thickness to Anterior Chamber Depth on the Vault after ICL Implantation
- The Benefits of One Day, One Eye Surgery in Bilateral ICL Implantation
- Effects of Prone Positioning on Critical Distance in Iris-Claw Phakic Intraocular Lens-Implanted Eyes
- The Analysis of Vault Change after Posterior Chamber Phakic Intraocular Lens Size Exchange
- Long-Term Changes in Tilt, Decentration and Anterior Chamber Depth After Implantable Collamer Lens Insertion