J Korean Ophthalmol Soc.
2008 Sep;49(9):1397-1405.
The Effect of an Anti-oxidative and Anti-inflammatory Functional Dietary Supplement in Dry Eye Syndrome
- Affiliations
-
- 1Department of Ophthalmology, College of Medicine, Chung-Ang University, Seoul, Korea. jck50ey@kornet.net
- 2Department of Ophthalmology, College of Medicine, Chonnam National University, Gwangju, Korea.
Abstract
- PURPOSE
To evaluate the effect of Optibiol(R), which is composed of multiple anti-oxidative and anti-inflammatory dietary elements, on the symptoms, clinical manifestations, and expression of various inflammatory cytokines in dry eye patients.
METHODS
Patients suffering from dry eye were given Optibiol(R) for 3 months. They completed questionnaires regarding dry eye symptom and underwent slit lamp biomicroscopic examinations, tear film breakup times, Shirmer tests, and conjunctival fluorescein staining examinations on a monthly basis during the intake of Optibiol(R). Sampling of serum and tears was conducted at baseline and 3 months after taking Optibiol(R), and various inflammatory cytokines in the serum and tears were measured with multiplex bead immunoassay.
RESULTS
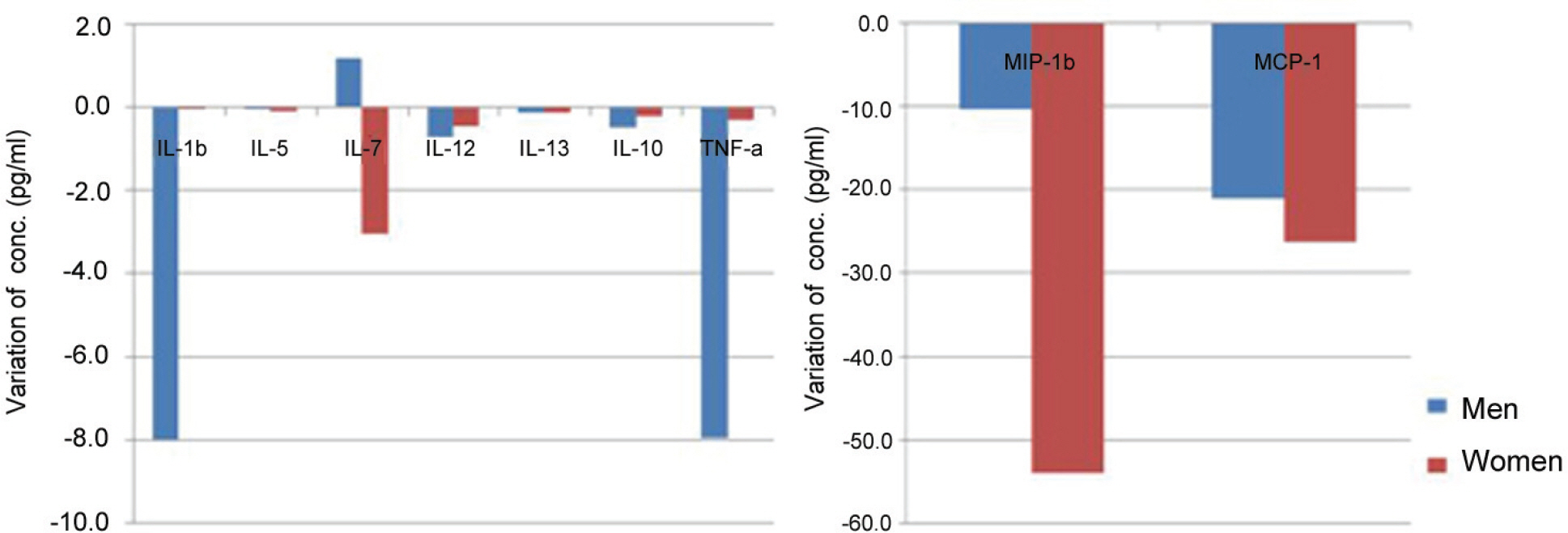
Sixty-three patients were included in this study. After taking Optibiol(R), the dry eye symptoms, Schirmer scores, tear film breakup times, and conjunctival staining scores (Oxford scale) showed significant improvement, and the expression of most inflammatory cytokines had decreased: in particular, IL-1 beta and MIP-1 beta in serum, and IL-17 and MIP-1 beta in tears were significantly lower.
CONCLUSIONS
Optibiol(R), an anti-oxidative and anti-inflammatory functional dietary supplement, is an effective dietary supplement in patients with dry eye syndrome. We posit that the decreased expression of inflammatory cytokines is an important mechanism in this effect.
MeSH Terms
Figure
Reference
-
References
1. Calder PC. Polyunsaturated fatty acids, inflammation and immunity. Lipids. 2001; 36:1007–24.
Article2. Calder PC. n-3 polyunsaturated fatty acids, inflammation and immunity: pouring oil on troubled waters or another fishy tale? Nutr Res. 2001; 21:309–41.3. Calder PC. n-3 fatty acids and cardiovascular disease: evidence explained and mechanisms explored. Clin Sci. 2004; 107:1–11.
Article4. Paiva SA, Russell RM. Beta carotene and other carotenoids as antioxidants. J Am Coll Nutr. 1999; 18:426–33.5. Snodderly DM. Evidence for protection against age-related macular degeneration by carotenoids and antioxidant vitamins. Am J Clin Nutr. 1995; 62:S1448–61.
Article6. Seddon JM, Ajani UA, Sperduto RD. . Dietary carotenoids, vitamins A, C, and E, and advanced age-related macular degeneration. JAMA. 1994; 272:1413–20.
Article7. Age-Related Eye Disease Study Research Group A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001; 119:1417–36.8. Age-Related Eye Disease Study Research Group A randomized, placebo controlled, clinical trial of high-dose supplementation with vitamins C and E and beta carotene for age-related cataract and vision loss: AREDS report no. 9. Arch Ophthalmol. 2001; 119:1439–52.9. Bron AJ. The Doyne Lecture. Reflections on the tears. Eye. 1997; 11:583–602.10. Lemp MA. The definition and classification of dry eye disease: report of the Definition and Classification Subcom mittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.11. Her J, Yu SI, Seo SG. Clinical effects of various antiinflammatory therapies in dry eye syndrome. J Korean Ophthalmol Soc. 2006; 47:1901–10.12. Stephen C, Pflugfelder SC. Antiinflammatory therapy for dry eye. Am J Ophthalmol. 2004; 137:337–42.13. Tatlipinar S, Akpek EK. Topical cyiclosporin in the treatment of ocular surface disorder. Br J Ophthalmol. 2005; 89:1363–7.14. Mrukwa-Kominek E, Rogowska-Godela A, Gierek-Ciaciura S. Effect of anti-inflammatory therapy on the treatment of dry eye syndrome. Klin Oczna. 2007; 109:79–84.15. Creuzot C, Passemard M, Viau S. . Improvement of dry eye symptoms with polyunsaturated fatty acids. J Fr Ophtalmol. 2006; 29((8)):868–73.16. Sherry B, Tekamp-Olson P, Gallegos C. . Resolution of the two components of macrophage inflammatory protein 1, and cloning and characterization of one of those components, macrophage inflammatory protein 1? . J Exp Med. 1988; 168:2251–9.17. Menten P, Wuyts A, Van Damme J. Macrophage inflammatory protein-1. Cytokine Growth Factor Rev. 2002; 13:455–81.
Article18. Mrugacz M, Zelazowska B, Bakunowicz-Lazarczyk A. . Elevated Tear Fluid Levels of MIP-1? in Patients with Cystic Fibrosis. J Interferon Cytokine Res. 2007; 27:491–6.
Article19. Yoon KC, De Paiva Cs, Qi H. . Expression of Th-1 Chemokines and Chemokine Receptors on the Ocular Surface of C57BL/6 Mice: Effects of Desiccating Stress. Invest Ophthalmol Vis Sci. 2007; 48:2561–9.
Article20. Suzuki Y, Ohgami K, Shiratori K. . Suppressive effects of astaxanthin against rat endotoxin-induced uveitis by inhibiting the NF-kappaB signaling pathway. Exp Eye Res. 2006; 82:275–81.21. Zhao Y, Yu W, Hu W, Yuan Y. Anti-inflammatory and anticoagulant activities of lycopene in mice. Nutrition Research. 2003; 23:1591–5.
Article22. Nakamura S, Shibuya M, Nakashima H. . Involvement of Oxidative Stress on Corneal Epithelial Alterations in a Blink-Suppressed Dry Eye. Invest Ophthalmol Vis Sci. 2007; 48:1552–8.
Article23. Tüzün A, Erdil A, Inal V. . Oxidative stress and antioxidant capacity in patients with inflammatory bowel disease. Clin Biochem. 2002; 35:569–72.
Article24. Francisco PG, Esther M, Salvador C, Tomas A. Anti-inflamatory action of pluchea sagittalis: involvement of an antioxidant mechanism. Life Sci. 1996; 59:2033–40.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Trends in the Recognition and Treatment of Dry Eye: A Survey of Ophthalmologists
- Current Practice Pattern for Dry Eye Patients in South Korea: A Multicenter Study
- Prevalence and Clinical Aspects of Sjogren Syndrome in Dry Eye Patients
- Anti-Inflammatory Effect of Phlorotannin on Chronic Nonbacterial Prostatitis in a Rat Model
- Beneficial Effects of Taurine on Metabolic Parameters in Animals and Humans