Korean J Ophthalmol.
2014 Apr;28(2):115-121. 10.3341/kjo.2014.28.2.115.
Current Practice Pattern for Dry Eye Patients in South Korea: A Multicenter Study
- Affiliations
-
- 1Department of Ophthalmology, Korea University College of Medicine, Seoul, Korea. hyomkim@hanmail.net
- 2Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- 3Department of Ophthalmology, Inje University College of Medicine, Goyang, Korea.
- 4Department of Ophthalmology, Sungkyunkwan University College of Medicine, Seoul, Korea.
- 5Department of Clinical Epidemiology and Biostatistics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 1792104
- DOI: http://doi.org/10.3341/kjo.2014.28.2.115
Abstract
- PURPOSE
To assess current practice patterns for dry eye patients in South Korea and to evaluate the preference according to the ages and clinic types of physicians.
METHODS
Dry eye patients (n = 1,612) were enrolled in this multicenter cross-sectional, observational study. The severity level of dry eye patients was classified based on the Korean guidelines for dry eye treatment. The medical records of the enrolled dry eye patients were evaluated, and the practice styles and the preferences were analyzed according to the ages and clinic types of physicians.
RESULTS
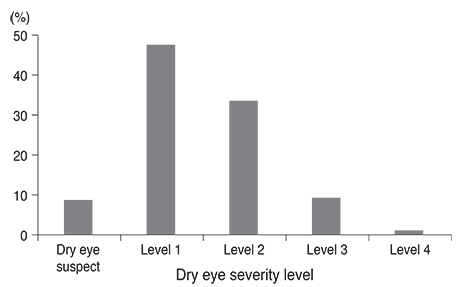
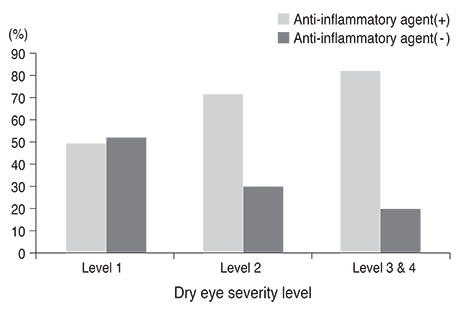
Of all patients, dry eye level 1 was most common (47.5%), followed by level 2 (33.5%), level 3 (9.1%), and level 4 (1.1%). Topical anti-inflammatory agents were used in 70.7% of patients with dry eye level 2 and in 80.6% of patients at levels 3 and 4. Topical anti-inflammatory agents were also used in 48.7% of patients with dry eye level 1. Preservative-free artificial tears were preferred at all dry eye levels. The use of topical anti-inflammatory agents did not differ with investigator ages, but older physicians preferred preserved artificial tears more than younger ones. Physicians at referral hospitals also tended to use topical anti-inflammatory agents and preservative-free artificial tears earlier, beginning at dry eye level 1, than those who worked at private eye clinics.
CONCLUSIONS
Topical anti-inflammatory agents were commonly prescribed for the treatment of dry eye patients in South Korea, even from dry eye level 1. Preservative-free artificial tears were preferred at all dry eye levels. Practice styles differed somewhat depending on the ages and clinic types of physicians.
MeSH Terms
-
Adult
Age Factors
Aged
Aged, 80 and over
Anti-Inflammatory Agents/*therapeutic use
Attitude of Health Personnel
Cross-Sectional Studies
Cyclosporine/*therapeutic use
Dry Eye Syndromes/*drug therapy
Fatty Acids, Essential/therapeutic use
Female
Humans
Lubricant Eye Drops/*therapeutic use
Male
Middle Aged
Ointments/therapeutic use
Ophthalmology/*standards
Practice Guidelines as Topic
*Professional Practice
Referral and Consultation
Republic of Korea
Severity of Illness Index
Young Adult
Anti-Inflammatory Agents
Cyclosporine
Fatty Acids, Essential
Lubricant Eye Drops
Ointments
Figure
Cited by 1 articles
-
Tear Meniscus Evaluation Using Optical Coherence Tomography in Dry Eye Patients
Na Yeon Jung, Ji Won Baek, Seong Joo Shin, Sung Kun Chung
J Korean Ophthalmol Soc. 2015;56(3):323-330. doi: 10.3341/jkos.2015.56.3.323.
Reference
-
1. Pflugfelder SC, Jones D, Ji Z, et al. Altered cytokine balance in the tear fluid and conjunctiva of patients with Sjogren's syndrome keratoconjunctivitis sicca. Curr Eye Res. 1999; 19:201–211.2. Tsubota K, Fujihara T, Saito K, et al. Conjunctival epithelium expression of HLA-DR in dry eye patients. Ophthalmologica. 1999; 213:16–19.3. Li DQ, Chen Z, Song XJ, et al. Stimulation of matrix metalloproteinases by hyperosmolarity via a JNK pathway in human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2004; 45:4302–4311.4. De Paiva CS, Corrales RM, Villarreal AL, et al. Corticosteroid and doxycycline suppress MMP-9 and inflammatory cytokine expression, MAPK activation in the corneal epithelium in experimental dry eye. Exp Eye Res. 2006; 83:526–535.5. Baudouin C. The pathology of dry eye. Surv Ophthalmol. 2001; 45:Suppl 2. S211–S220.6. Turner K, Pflugfelder SC, Ji Z, et al. Interleukin-6 levels in the conjunctival epithelium of patients with dry eye disease treated with cyclosporine ophthalmic emulsion. Cornea. 2000; 19:492–496.7. Brignole F, Pisella PJ, De Saint Jean M, et al. Flow cytometric analysis of inflammatory markers in KCS: 6-month treatment with topical cyclosporin A. Invest Ophthalmol Vis Sci. 2001; 42:90–95.8. Kunert KS, Tisdale AS, Gipson IK. Goblet cell numbers and epithelial proliferation in the conjunctiva of patients with dry eye syndrome treated with cyclosporine. Arch Ophthalmol. 2002; 120:330–337.9. Behrens A, Doyle JJ, Stern L, et al. Dysfunctional tear syndrome: a Delphi approach to treatment recommendations. Cornea. 2006; 25:900–907.10. Management and therapy of dry eye disease: report of the Management and Therapy Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:163–178.11. Jackson WB. Management of dysfunctional tear syndrome: a Canadian consensus. Can J Ophthalmol. 2009; 44:385–394.12. Wilson SE, Stulting RD. Agreement of physician treatment practices with the international task force guidelines for diagnosis and treatment of dry eye disease. Cornea. 2007; 26:284–289.13. Gasset AR, Ishii Y, Kaufman HE, et al. Cytotoxicity of ophthalmic preservatives. Am J Ophthalmol. 1974; 78:98–105.14. Wilson FM 2nd. Adverse external ocular effects of topical ophthalmic medications. Surv Ophthalmol. 1979; 24:57–88.15. Burstein NL. Corneal cytotoxicity of topically applied drugs, vehicles and preservatives. Surv Ophthalmol. 1980; 25:15–30.16. Nelson JD. Simultaneous evaluation of tear turnover and corneal epithelial permeability by fluorophotometry in normal subjects and patients with keratoconjunctivitis sicca (KCS). Trans Am Ophthalmol Soc. 1995; 93:709–753.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent treatment of dry eye
- Characteristics of Tear Lipid Layer on Tears copy in Dry Eye Symptom and Non-Dry Eye Symptom Group
- Current Trends in the Recognition and Treatment of Dry Eye: A Survey of Ophthalmologists
- Bacterial Conjuntival Flora in Dry Eye Patients
- Change of Lipid Layer in Tear Film after Cataract Surgery